Abstract
Paraganglioma, also termed extra-adrenal pheochromocytoma, may be observed at the base of the skull and neck as well as within the mediastinum and periaortic region. The clinical symptoms of paraganglioma of the urinary bladder include intermittent hypertensive attacks, micturition, headaches and palpitations due to high catecholamine levels; these types of paragangliomas are extremely rare. However, certain bladder paragangliomas do not present with any of these symptoms; thus, surgeons are not pre-warned on how to prepare for their resection. Surgery to remove pheochromocytomas may therefore result in an intraoperative hypertensive crisis and increase the mortality rate. This infrequent type of paraganglioma is only recognized through histological examination following surgery. The current study reports the case of a 61-year-old male with urinary bladder paraganglioma. The patient presented with hypertension, which was controlled to within a normal range using diovan and norvasc treatment; in addition, the patient's blood pressure was not altered with urination or postural changes. The patient was not administered an α-blocking agent or a blood volume expander prior to the surgery, and during the partial cystectomy no hypertensive crisis occurred.
Keywords: pheochromocytoma, non-functioning paraganglioma, urinary bladder
Introduction
Paraganglioma, which is also referred to as extra-adrenal pheochromocytoma, is an uncommon type of neuroendocrine neoplasm with an estimated incidence rate of 3 per million population; in addition, paragangliomas have been observed in patients of all age-groups (1). Paragangliomas are known to occur at the base of the skull base and neck as well as within the mediastinum and periaortic region. It is estimated that ~10% of all paragangliomas are malignant and metastasize at sites where chromaffin tissue is rarely observed (2,3). In the genitourinary tract, the urinary bladder is the primary site for paragangliomas (79.2%), followed by the urethra (12.7%), pelvis (4.9%) and ureter (3.2%) (3,4). In addition, urinary bladder paragangliomas account for 0.06% of all bladder tumors and 6% of extra-adrenal pheochromocytomas (5).
Paragangliomas of the bladder present with the clinical symptoms of pheochromocytoma, which include headaches, palpitations and fainting as a result of the induction of catecholamine release from functional bladder paragangliomas when urinating (6). A proportion of patients present with the clinical symptoms of bladder tumors, such as hematuria. Out of these urinary bladder paragangliomas, 10–15% are non-functioning and a further 10% have hormonal activities that do not manifest clinically. Therefore, these paragangliomas are occasionally diagnosed incorrectly; thus, surgeons are unprepared and the surgery to remove paragangliomas may result in an intraoperative hypertensive crisis and increase the mortality rate (7).
Several reviews have been published on paragangliomas of the urinary bladder (8,9); however, non-functioning paragangliomas of the urinary bladder have rarely been reported (10). The present study reports the case of an asymptomatic patient with non-functioning paraganglioma of the bladder, which was detected as a mass on urinary ultrasonography scans.
Case report
Written informed consent was obtained from the patient prior to the publication of this case report and any accompanying images.
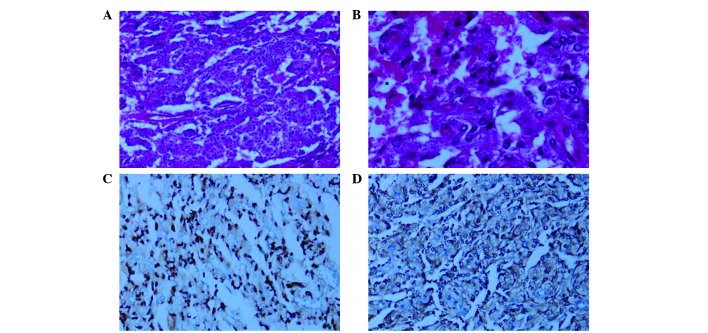
The bladder mass of a 61-year-old male patient was observed in January 2014 using urinary ultrasonography during a medical examination at the West China Hospital of Sichuan University (Chengdu, China). The ultrasound study (EPIQ 5, Philips Diagnostic Ultrasound System and Transducers, Bothell, WA, USA) revealed a mass (3.7×2.5×3.7 cm) on the left anterior wall of the bladder; in addition, color Doppler sonography indicated that the mass had predominantly arterial vascularization (Fig. 1). The patient was then admitted. The patient had a 10-year history of hypertensive disease (the highest blood pressure recorded was 168/100 mmHg); however, the patient's blood pressure had been controlled to 120/80 mmHg through treatment with diovan (80 mg, once-a-day) and norvasc (5 mg, once-a-day). The patient had no history of hematuria, headaches, palpitations or dizziness associated with micturition or postural changes. Routine blood and urine tests demonstrated no abnormalities.
Figure 1.
(A) An ultrasound identified a mass (3.7×2.5×3.7 cm) on the left anterior wall of bladder and (B) color Doppler sonography revealed that this mass had predominantly arterial vascularization.
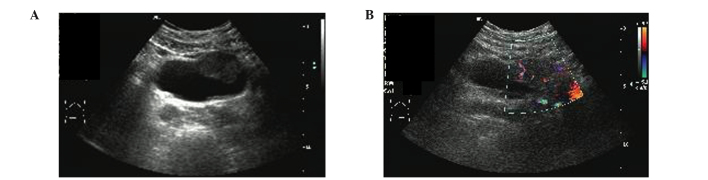
A computed tomography (CT) scan (SOMATOM Sensation64 MSCT, Siemens AG, Berlin, Germany) of the patient's abdomen and pelvis revealed a 3.9×3.6 cm mass on the left anterior aspect of the bladder, which protruded into the bladder cavity; the mass had well-defined borders and there was no thickening of the bladder wall surrounding the mass. On the plain CT images, it appeared that the mass had a homogeneous iso-density (Fig. 2A); however, contrast-enhanced CT images demonstrated that the degree of enhancement of the tumor was markedly increased compared with that of the bladder wall (Fig. 2B). Metastatic disease of the other abdominal organ systems was not observed on ultrasound examination or CT scans. The solitary submucosal mass on the left anterior aspect of the bladder with normal mucosal covering was confirmed by cystoscopy (Olympus Cystoscope A4620, Olympus Corporation, Tokyo, Japan).
Figure 2.
(A) Plain CT image demonstrating the homogeneous iso-density of the mass. (B) Contrast-enhanced CT image showing that the degree of enhancement of the tumor was increased compared with that of the bladder wall. CT, computed tomography.
On the basis of these examinations, the patient was diagnosed with a bladder tumor and underwent a partial cystectomy. The entire tumor was resected and during the intervention, no hypertensive crisis occurred.
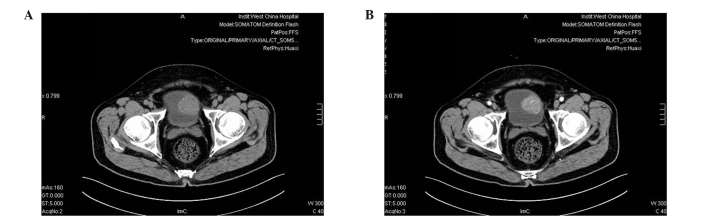
Pathological analysis demonstrated that the mass on the left anterior aspect of the bladder was a paraganglioma. It was confirmed using positive immunohistochemical stains for neuron-specific enolase (mouse anti-human monoclonal NSE; cat. no. M0873; Dako, Glostrup, Denmark; dilution, 1:100; incubation, 1 h at 37°C) and chromagranin (mouse anti-human monoclonal chromagranin; cat. no. ZM-0076; ZSGB-BIO, Beijing, China; dilution, 1:150; incubation, 1 h at 37°C) as well as negative immunoreactions for muscle-specific actin (MSA) (mouse anti-human monoclonal MSA; cat. no. 0032; Fuzhou Maixin Biotechnology Development Co., Ltd., Fuzhou, China; 1:60, incubation, 1 h at 37°C), desmin (mouse anti-human monoclonal desmin; cat. no. M0760; Dako; dilution, 1:100; incubation, 1 h at 37°C), pan cytokeratin (mouse anti-human monoclonal PCK; cat. no. ZA-0573; ZSGB-BIO; dilution, 1:100; incubation, 1 h at 37°C) and epithelial membrane antigen (mouse anti-human monoclonal EMA; cat. no. M0613; Dako; dilution, 1:100; incubation, 1 h at 37°C) were negative. The Ki-67 labeling index was ~5% (Fig. 3).
Figure 3.
(A and B) Hematoxylin-eosin staining of epithelioid cells demonstrates their arrangement in nests in paraganglioma (magnification, x40 and x400, respectively). Positive immunostaining for (C) chromogranin and (D) neurone-specific enolase (magnification, x200).
The patient demonstrated good postoperative recovery and at 3 months follow-up the patient felt well, with no signs of recurrence. The patient's blood pressure was not affected by the operation; however, continuation of diovan and norvasc treatment is required to control the hypertension to within a normal range.
Discussion
Paragangliomas account for ~10% of pheochromocytoma and 800 cases are diagnosed annually in the USA (2). Paragangliomas are observed in patients of all ages; however, they have been found to occur more frequently during the 2nd decade of life and the ratio of female to male patients is 3:2 (11–13). The most common site for paragangliomas is the organ of Zuckerkandl at the distal aorta or aortic bifurcation and less commonly, they are observed in the head, neck, thorax and bladder (14). The first case of a paraganglioma of the bladder was described by Zimmerman et al (15) in 1953. Pheochromocytomas and paragangliomas may secrete catecholamines and these substances are responsible for symptoms, including headache, palpitations and fainting. Hypertensive crises may be triggered by inducing the release of catecholamine during urination if the bladder paraganglioma is functional. Therefore endocrine tests, including those for metanephrines, vanillylmandelic acid, epinephrine, norepinephrine and dopamine in a 24-h urine and serum sample, must be performed when a case of urinary bladder paraganglioma is suspected. However, 10–15% of such tumors are non-functioning and a further 10% have hormonal activities that do not manifest clinically (11). This type of tumor does not have produce typical test results from blood or urine samples collected at the occurrence of typical symptoms. If the surgeons are unprepared for the resection of paragangliomas during pheochromocytoma surgery, it may result in intraoperative hypertensive crises and increase the risk of mortality. Therefore, when a paraganglioma of the bladder is suspected and the basal catecholamine levels appear normal, it may be beneficial for diagnosis to measure the plasma catecholamine concentrations prior to, during and following micturition (16).
Imaging examinations are essential for preoperative localization and qualitative analysis. The sensitivities of the localizing examination for ultrasound, CT scan, magnetic resonance imaging and 131I-metaiodobenzylguanidine are 89, 64–100, 88–100 and 62–88%, respectively (11,17,18). Positron emission tomography (PET) has an increased accuracy compared with MIBG scans for the localization of paragangliomas due to the higher spatial resolution of PET scanning (19).
Bladder paragangliomas are frequently treated surgically. The surgical options include radical cystectomy, partial cystectomy and transurethral resection. It was estimated that ~3% of patients treated by the above therapies succumbed to their cancer. However, it is important to note that ≥20% of patients had recurrence or metastases at the last known follow-up (20,21). The present case report may be helpful to standardize the reporting guidelines of paraganglioma cases in order to better understand its natural progression and outcomes.
The current study presented the case of a 61-year-old male with urinary bladder paraganglioma. Notably, the patient did not exhibit any of the typical symptoms associated with bladder paraganglioma, such as headache, palpitations and postural changes, and thus initially a diagnosis of paraganglioma was not considered. For patients who are suspected to have paraganglioma, it is necessary to stabilize hypertension prior to surgical treatment with α-blocking agents. In the present case, partial cystectomy was performed without the pre-operative adminstration of α-blocking agents and fortunately, no hypertensive crisis or bleeding occurred during surgery.
It is extremely difficult to pre-operatively diagnose asymptomatic bladder paraganglioma. Based on the present case and previous studies, if CT or cystoscopy reveals a mass with well-defined borders that is located in the submucosa with an intact surface, a diagnosis of bladder paraganglioma must be considered and subsequent preoperative preparations must be performed to reduce the risk of intraoperative hypertensive crisis.
References
- 1.Tischler AS. Pheochromocytoma and extra-adrenal paraganglioma: Updates. Arch Pathol Lab Med. 2008;132:1272–1284. doi: 10.5858/2008-132-1272-PAEPU. [DOI] [PubMed] [Google Scholar]
- 2.Elder EE, Elder G, Larsson C. Pheochromocytoma and functional paraganglioma syndrome: No longer the 10% tumor. J Surg Oncol. 2005;89:193–201. doi: 10.1002/jso.20177. [DOI] [PubMed] [Google Scholar]
- 3.Dahm P, Gschwend JE. Malignant non-urothelial neoplasms of the urinary bladder: A review. Eur Urol. 2003;44:672–681. doi: 10.1016/S0302-2838(03)00416-0. [DOI] [PubMed] [Google Scholar]
- 4.Hanji AM, Rohan VS, Patel JJ, Tankshali RA. Pheochromocytoma of the urinary bladder: A rare cause of severe hypertension. Saudi J Kidney Dis Transpl. 2012;23:813–816. doi: 10.4103/1319-2442.98167. [DOI] [PubMed] [Google Scholar]
- 5.Pastor-Guzmán JM, López-García S, Giménez-Bachs JM, et al. Paraganglioma of the bladder: Controversy regarding treatment. Urol Int. 2004;73:270–275. doi: 10.1159/000080841. [DOI] [PubMed] [Google Scholar]
- 6.Sheps SG, Jiang NS, Klee GG, van Heerden JA. Recent developments in the diagnosis and treatment of pheochromocytoma. Mayo Clin Proc. 1990;65:88–95. doi: 10.1016/S0025-6196(12)62113-2. [DOI] [PubMed] [Google Scholar]
- 7.Messerli FH, Finn M, MacPhee AA. Pheochromocytoma of the urinary bladder. Systemic hemodynamics and circulating catecholamine levels. JAMA. 1982;247:1863–1864. doi: 10.1001/jama.1982.03320380055031. [DOI] [PubMed] [Google Scholar]
- 8.Feng N, Li X, Gao HD, Liu ZL, Shi LJ, Liu WZ. Urinary bladder malignant paraganglioma with vertebral metastasis: A case report with literature review. Chin J Cancer. 2013;32:624–628. doi: 10.5732/cjc.012.10317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Beilan J, Lawton A, Hajdenberg J, Rosser CJ. Locally advanced paraganglioma of the urinary bladder: A case report. BMC Res Notes. 2013;6:156. doi: 10.1186/1756-0500-6-156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Li S, Lui S, Li F, Yue Q, Huang X, Gong Q. Unsuspected paraganglioma of the urinary bladder with intraoperative hypertensive crises: A case report. Exp Ther Med. 2013;6:1067–1069. doi: 10.3892/etm.2013.1242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lucon AM, Pereira MA, Mendonça BB, Halpern A, Wajchenbeg BL, Arap S. Pheochromocytoma: Study of 50 cases. J Urol. 1997;157:1208–1212. doi: 10.1016/S0022-5347(01)64925-5. [DOI] [PubMed] [Google Scholar]
- 12.Bolli V, Cerioni M, Martino A, et al. Unusual benign mass of the bladder in children: Report of 2 cases. Radiol Med. 1996;92:154–156. (In Italian) [PubMed] [Google Scholar]
- 13.Kouame BD, Lardy H, Michalak S, Lacombe A, Mercier C, Robert M. Bladder paraganglioma (pheochromocytoma): A rare tumor in children. Apropos of a case. Ann Urol (Paris) 1998;32:363–366. (In French) [PubMed] [Google Scholar]
- 14.Lee KY, Oh YW, Noh HJ, et al. Extraadrenal paragangliomas of the body: Imaging features. AJR Am J Roentgenol. 2006;187:492–504. doi: 10.2214/AJR.05.0370. [DOI] [PubMed] [Google Scholar]
- 15.Zimmerman IJ, Biron RE, MacMahon HE. Pheochromocytoma of the urinary bladder. N Engl J Med. 1953;249:25–26. doi: 10.1056/NEJM195307022490106. [DOI] [PubMed] [Google Scholar]
- 16.Lecube A, Peña A, Hernández C, Simó R. Bladder pheochromocytoma: A variation in the plasma catecholamines during micturition. Med Clin (Barc) 1999;112:477–478. (In Spanish) [PubMed] [Google Scholar]
- 17.Bravo EL. Evolving concepts in the pathophysiology, diagnosis and treatment of pheochromocytoma. Endocr Rev. 1994;15:356–368. doi: 10.1210/edrv-15-3-356. [DOI] [PubMed] [Google Scholar]
- 18.Jalil ND, Pattou FN, Combemale F, et al. Effectiveness and limits of preoperative imaging studies for the localisation of pheochromocytomas and paragangliomas: A review of 282 cases. French Association of Surgery (AFC), and The French Association of Endocrine Surgeons (AFCE) Eur J Surg. 1998;164:23–28. doi: 10.1080/110241598750004913. [DOI] [PubMed] [Google Scholar]
- 19.Pacak K, Eisenhofer G, Goldstein DS. Functional imaging of endocrine tumors: Role of positron emission tomography. Endocr Rev. 2004;25:568–580. doi: 10.1210/er.2003-0032. [DOI] [PubMed] [Google Scholar]
- 20.Jansen R, Zaslau S. Paraganglioma of the bladder. Clin Adv Hematol Oncol. 2012;10:839–841. [PubMed] [Google Scholar]
- 21.Tsai CC, Wu WJ, Chueh KS, et al. Paraganglioma of the urinary bladder first presented by bladder bloody tamponade: Two case reports and review of the literatures. Kaohsiung J Med Sci. 2011;27:108–113. doi: 10.1016/j.kjms.2010.05.005. [DOI] [PubMed] [Google Scholar]