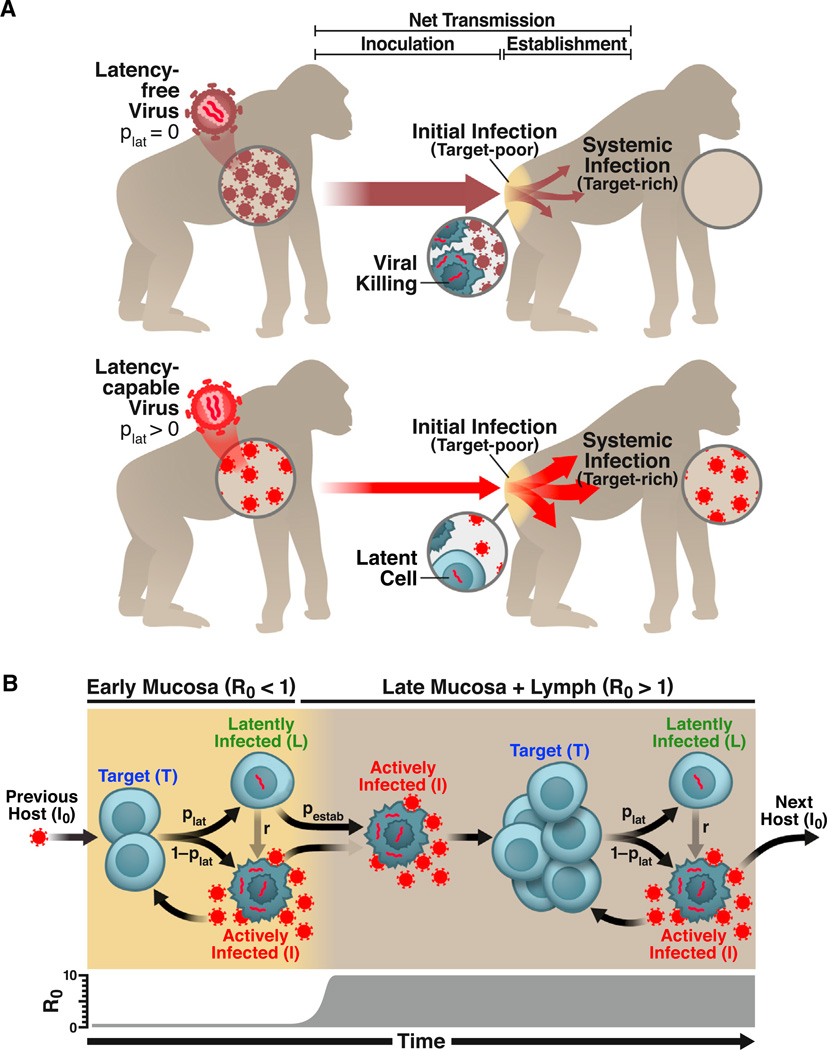
Figure 1. HIV Latency as a Bet-Hedging Strategy for Maximizing Viral Transmission.
(A) Schematic of the lentiviral transmission process. Lentiviral transmission is illustrated as a two-compartment process, beginning with viral inoculation in the mucosa and progressing—in some cases—to systemic infection in the lymphoid tissue, where >98% of CD4+ T cells reside (Murphy, 2011). The parameter plat reflects the probability that an HIV-infected cell enters latency. An HIV strain incapable of entering latency (plat = 0) would generate increased viral loads during systemic infection, transferring more virions to new hosts. However, the latency-incapable virions would rapidly destroy the small CD4+ T cell population initially present in the mucosa of the new host—reducing the probability of systemic infection (upper). In contrast, an HIV strain capable of entering latency (plat > 0) would generate lower viral loads during systemic infection, transferring fewer virions to new hosts. Yet, the relatively few transferred virions would not destroy all mucosal target cells. By entering long-lived latency in some mucosal cells, the latency-capable strain would increase its probability of surviving initial infection to establish systemic infection (lower).
(B) Schematic of the two-compartment model of lentiviral transmission. The two major processes controlling the probability of lentiviral transmission (ptransmission) are: (1) the inoculum of infected cells (I0) and (2) the probability that an infected cell in the inoculum survives initial infection to establish systemic infection (pestab). (Right to left) HIV enters a host mucosal site, but due to the small number of permissive target cells in the early mucosa (prior to day 6), R0 < 1. To successfully establish systemic infection, the virus must avoid extinction until R0 > 1. Critically, the likelihood of an actively infected cell or a free viral particle surviving until day 6 to initiate systemic infection is negligible since virus-producing cells die within 40 hr of infection and viral progeny are cleared from the system ~100-fold more rapidly. In contrast, latently infected cells are long-lived and can reactivate once R0 > 1 to initiate systemic viral expansion. Therefore, despite reducing long-term viral loads, latency may increase ptransmission by increasing viral survival during initial infection. This would make latency evolutionarily beneficial at the population scale.
See also Figure S1