Abstract
Objective: Cognitive models suggest that the self-concept of persons with psychosis can be fundamentally affected. Self-concepts were found to be related to different symptom domains when measured concurrently. Longitudinal investigations to disentangle the possible causal associations are rare.
Method: We examined a sample of 160 people with a diagnosis of schizophrenia who took part in a psychotherapy study. All participants had the DSM-IV diagnosis of a schizophrenia and pronounced negative symptoms. Neurocognition, symptoms, and self-concepts were assessed at two time points 12 months apart. Structural equation modeling was used to test whether symptoms influence self-concepts (scar-model) or self-concepts affect symptoms (vulnerability model).
Results: Negative symptoms correlated concurrently with self-concepts. Neurocognitive deficits are associated with more negative self-concepts 12 months later. Interpersonal self-concepts were found to be relevant for paranoia.
Conclusion: The findings implicate that if deficits in neurocognition are present, fostering a positive self-concept should be an issue in therapy. Negative interpersonal self-concept indicates an increased risk for paranoid delusions in the course of 1 year. New aspects for cognitive models in schizophrenia and clinical implications are discussed.
Keywords: cognitive models, structural equation modeling, self-esteem, psychological model, self-schema
Introduction
In cognitive models of paranoid delusions and negative symptoms negative self-concepts in terms of reduced self-efficacy, self-acceptance, self-esteem, and expectancies for pleasure play a major role (Rector et al., 2005; Kesting and Lincoln, 2013). Self-concepts integrate cognitive, emotional, and motivational reflections of the self. For the emotional aspect, self-esteem, as an evaluative self-concept, is a prominent factor as well as an important outcome in mental health research. Self-concepts are central to the health care of people with schizophrenic psychoses as a core element of quality of life (Weinberg et al., 2012) as well as a potential mediator between treatment and outcome. Self-esteem in schizophrenia was found to be linked to depression (Cavelti et al., 2012a), quality of life (Staring et al., 2009), functional outcomes (Vracotas et al., 2012), negative symptoms (Palmier-Claus et al., 2011a), and positive symptoms (Barrowclough et al., 2003; Thewissen et al., 2011).
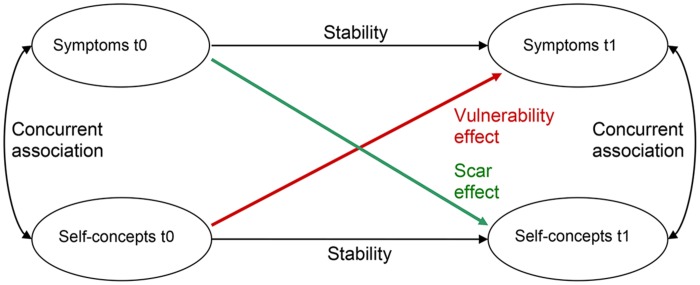
The relationship between symptoms and self-concepts are typically discussed in two ways (Klein et al., 2011). First, negative self-concepts can be regarded as vulnerability for higher symptom severity as the capability for coping with stressful events might be reduced (Zubin and Spring, 1977; Bentall et al., 1994). Second, symptoms might induce negative changes in the self-concepts, which may be considered as a scar (Lewinsohn et al., 1981). The ideas of the vulnerability and the scar model are summarized graphically in Figure 1. In a meta-analysis of 77 studies with representative, non-representative, and clinical samples the vulnerability model showed stronger effects than the scar model for depression (Sowislo and Orth, 2013).
FIGURE 1.
Theoretical model integrating the scar and the vulnerability model at two time points (t0 and t1); adapted from Sowislo and Orth (2013).
Although the course of self-concepts and symptoms has been studied extensively in depressive disorders, evidence is scarce in psychotic disorders. Most available studies refer to the development and course of paranoia. Cognitive models state that dysfunctional self-concepts contribute to paranoid delusions (Bentall et al., 1994; Garety et al., 2001; Freeman et al., 2002). Recent clinical (Thewissen et al., 2011), non-clinical (Thewissen et al., 2008), and experimental evidence (Palmier-Claus et al., 2011b; Kesting et al., 2013) elucidated the association between self-concepts and positive symptoms, especially paranoid delusions. Particularly the relationship between self-esteem, stigma, insight, depression, and positive symptoms has been studied comprehensively (Lysaker et al., 2007; Cavelti et al., 2012b; Erickson and Lysaker, 2012). In their review regarding this topic, Kesting and Lincoln (2013) concluded that negative interpersonal self-concepts and low self-esteem can lead to persecutory delusions.
Neurocognition is a reliable predictor of functional outcome (Green et al., 2000; Bowie et al., 2010). These cognitive dysfunctions are relative stable through the course of the illness and are merely unaffected by medication (Harvey and Keefe, 2001). Neurocognitive deficits are even present in first-episode populations (Reichenberg et al., 2009). Verbal memory performance is enhanced in the year after remission of positive symptoms but performance levels remain impaired (Wittorf et al., 2004). The same picture is shown for high-risk patients; the deficits are viable before onset, but improve over time (Bora and Murray, 2014). Intensified programs of cognitive remediation can yield to better cognitive performance and functioning (Wykes et al., 2011; Sanchez et al., 2014).
In the cognitive model of negative symptoms, defeatist beliefs are related to symptoms like avolition, anhedonia, and affective flattening (Rector et al., 2005). Some studies confirmed these associations between self-reported expectancies about competences, success, or acceptance, and observer-rated negative symptoms (Grant and Beck, 2009). In the same study the authors found that defeatist beliefs about oneself mediate the association between neurocognition and functional outcome, supporting the scar model for neurocognition. Furthermore, interpersonal self-concepts and self-esteem correlated with negative symptoms (Lincoln et al., 2011). Palmier-Claus et al. (2011b) reported data supporting the vulnerability model for negative symptoms in early psychosis. In their study, the change in self-concepts predicted the course of negative symptoms.
Self-concepts can play a substantial role for subjective well being and for recovery. Especially self-esteem and self-efficacy have been pointed out as important personal traits within the recovery process (Yanos and Moos, 2007). Self-concepts are targets in narrative enhancement therapy (Yanos et al., 2011), schema-therapy (Bortolon et al., 2013), meta cognitive therapy (Moritz et al., 2014), and acceptance, and commitment therapy (Gaudiano and Herbert, 2006). Especially in the narrative enhancement therapy fragmented self-narratives and self-stigma are targeted. These approaches could enrich cognitive behavioral therapy for psychosis (Tai and Turkington, 2009) as well as self-concepts could give a new focus for family interventions (Hesse et al., 2015; Yesufu-Udechuku et al., 2015).
In the present study, our purpose was to examine the plausibility of the scar and vulnerability models regarding the clinically most significant areas of symptoms and neurocognition in people with schizophrenic psychosis. First, we expected that all symptom domains, including neurocognitive deficits, are associated with self-concepts. Second, we expected to find further evidence for the vulnerability effect referring to positive and negative symptoms and a scar effect referring to neurocognition.
Materials and Methods
Subjects and Procedures
The original sample comprised 198 outpatients who participated in a randomized controlled trial for the treatment of negative symptoms with cognitive behavioral therapy in three University Hospitals (TONES-study, ISRCTN25455020; Klingberg et al., 2009, 2011). All participants gave written informed consent. The study was conducted in accordance with the Declaration of Helsinki and the guidelines of the local University ethics committees (Tuebingen, Frankfurt, and Duesseldorf). The DSM-IV diagnosis of schizophrenia was confirmed by a structured clinical interview (SCID-I). Assessment of symptoms was performed by trained raters. The inclusion and exclusion criteria are reported in detail in the study protocol (Klingberg et al., 2009). Study participants had to have at least moderate negative symptoms and no severe depressive (PANNS G07, depression ≥6) or severe positive symptoms [any item of the standard PANSS positive scale (P1, P2, P3, P4, P5, P6, P7) ≥6]. The study population represents a more homogenous subgroup of people diagnosed with schizophrenia, than a random or unselected sample. A little loss of data (19%) occurred due to reward given for ratings to all participants and external data monitoring. We analyzed data of 160 participants whose follow-up data (12 months) were available. Missing data were imputed with expectation-maximization imputation models.
Measures and Latent Variable Construction
We grouped indicators to five latent constructs and tested the measurement adequacy empirically (Klingberg et al., 2006; Nuechterlein et al., 2008; Kim et al., 2012; Khan et al., 2013). As indicators of a latent construct may differ in the degree to which they represent the latent construct, we examined factor loadings as a measure of the strength of association between the indicator and the construct.
Negative symptoms were measured by the Positive and Negative Symptom Scale (PANSS) and the Scale for the Assessment of Negative Symptoms (SANS). The corresponding factor loadings to the negative symptoms factors in our analyses can be considered as high (0.86–0.96), respectively.
Paranoia was measured by the “delusions” item from the PANSS (item P1) and the “vsuspiciousness/persecution” item from the PANSS (item P6). The factor loadings ranged from 0.51 to 0.84.
Two domains of neurocognition, verbal recall and processing speed, were selected as particularly relevant. The Trail Making Test (TMT) consists of two parts, one (part A) measures mainly processing speed. Verbal memory was measured by the Verbaler Lern und Merkfähigkeitstest Test (VLMT). The two tests represent two different domains of neurocognitive functioning, therefore lower factor loadings were expected. For sake of content validity of the factor we decided to keep verbal memory in the construct. The factor loadings of the tests ranged from 0.41 to 0.81, indicating that verbal memory is not as well represented in the neurocognitive functioning construct as processing speed.
Self-concepts were assessed with the Frankfurt Self-Concept Scales (FSKN; Deusinger, 1986). This inventory comprises 10 one-dimensional scales with specific self-concepts concerning relevant aspects of the self. The internal consistency of the scales was highly satisfactory (α = 0.93–0.97; n = 1794). The questionnaire has been used in psychosis research frequently (Lincoln et al., 2010, 2011; Wittorf et al., 2010). We used six subscales for our analysis, three to measure positive self-concept, and three to measure interpersonal self-concept.
The self-concepts “general achievement,” “solving daily problems,” and “self-esteem” were used to measure positive self-concept. The factor loadings of these subscales ranged from 0.88 to 0.93. Interpersonal self-concept was measured with three subscales from the FSKN: “valued by others,” “ability to make contact with other people “and” emotions and relations to others.” The factor loadings of these subscales ranged from 0.59 to 0.86.
Statistical Analysis
First we checked if the two psychotherapeutic interventions to which patients were allocated in the RCT have any significant differential treatment effect on the variables of interest. Analysis of covariance (ANCOVA) was conducted with t1 as the dependent and t0 and treatment group as independent variables for each symptom and self-concept. We used structural equation modeling (SEM) techniques to test the main hypotheses of longitudinal associations. SEM is a confirmative technique allowing the construction of latent variables by observed indicators and testing the relations between the latent constructs.
We examined the vulnerability model and the scar model for different symptoms and self-concepts comparing estimates of strength of association and fit indexes. In a preparatory investigation of assumptions of SEM both skewness and kurtosis of the modeled indicators were within acceptable limits (Kline, 2011). A total of six longitudinal models were defined using data from baseline (t0) and 12-months follow-up (t1) with combinations of the two areas of self-concepts (positive self-concept and interpersonal self-concept) and three symptom domains (paranoia, negative symptoms, and neurocognition). We allowed autocorrelations between indicators over time. When Heywood cases (negative error variances) occurred, problematic autocorrelations have been fixed at 0. For each self-concept-symptom pair, an unrestricted model including all paths and thus allowing for both scar and vulnerability effects was estimated. Subsequently, partly restricted models omitting one path each representing the vulnerability or the scar model were fit, respectively. Finally, a fully restricted model excluding both scar and vulnerability effects was estimated.
All analyses were performed with AMOS and SPSS (Version 21.0. Armonk, NY: IBM Corporation).
Results
The ANCOVAs for differential effects of the interventions resulted in no significant (P < 0.05) difference between the two groups for any reported variable. Therefore the treatment group was not considered in further analyses. Anyway, we report in the appendix on models incorporating the group factor to rule out influence of treatment.
The mean scores and SD for all variables are summarized in Table 1. The sample comprised only a few first-episode patients, and the majority was male. Level of occupation and of general functioning indicates that the sample was moderately to severely impaired. The sample is characterized by rather weak positive symptoms and moderate to severe negative symptoms. The mean results in the VLMT are about one SD lower than the results in an age-matched normative sample (M = 52.27, SD = 7.84; Lux et al., 1999). The time needed to complete the TMT A is more than one SD above the mean in the age-matched normative sample (M = 28.54, SD = 10.09; Tombaugh, 2004).
Table 1.
Demographic and clinical characteristics of the sample.
| t0 (Baseline) |
t1 (12 months) | ||||||
|---|---|---|---|---|---|---|---|
| Frequency | Percent | ||||||
| Female | 66 | 41 | |||||
| High school | 84 | 52 | |||||
| Occupation | 44 | 28 | |||||
| Married/with partner | 65 | 41 | |||||
| Adverse child events | 31 | 19 | |||||
| First episode | 11 | 7 | |||||
| Mean | SD | Mean | SD | ||||
| Age (years) | 36.90 | 9.83 | |||||
| Age at first psychiatric symptom (years) | 23.77 | 8.74 | |||||
| GAF (score) | 59.58 | 8.91 | 63.34 | 11.47 | |||
| Verbal IQ | 108.72 | 16.72 | |||||
| PANSS | |||||||
| PANSS P01 (item score) | 1.89 | 1.00 | 2.06 | 1.23 | |||
| PANSS P06 (item score) | 2.00 | 0.91 | 1.94 | 1.07 | |||
| PANSS MNS (mean item score) | 3.02 | 0.80 | 2.58 | 0.90 | |||
| SANS (mean score) | 2.01 | 0.65 | 1.69 | 0.78 | |||
| TMT A (section) | 38.68 | 15.71 | 33.59 | 14.11 | |||
| VLMT learning (sum words) | 45.16 | 10.66 | 46.69 | 11.79 | |||
| FSKN | |||||||
| General achievement (FSGA) | 3.51 | 0.90 | 3.70 | 0.90 | |||
| Solving daily problems (FSSP) | 3.65 | 0.81 | 3.78 | 0.82 | |||
| Self-esteem (FSSE) | 3.68 | 1.05 | 3.95 | 0.99 | |||
| Valued by others (FSVO) | 3.69 | 0.99 | 3.87 | 1.03 | |||
| Ability to make contact (FSAC) | 3.73 | 0.84 | 3.91 | 0.78 | |||
| Emotions and relationships (FSEO) | 3.80 | 0.82 | 3.75 | 0.78 | |||
N = 160; Occupation, Fulltime occupation or education; GAF, Global Assessment of Functioning, PANSS P01, delusions; P06, suspiciousness/persecution; MNS, modified negative symptom scale; SANS, Scale for the Assessment of Negative Symptoms; TMT A, Trail Making Test Trail A; VLMT, Verbaler Lern und Merkfähigkeitstest; FSKN, Frankfurt Self-Concept Scales.
Negative symptoms were the first domain to be tested with regard to the vulnerability and the scar model. The fit of all models is good. The restricted model, omitting the paths representing the vulnerability and the scar model, does not significantly impact the model fit. The goodness of fit statistics are summarized in Table 2. Negative symptoms were fairly stable over time as indicated by a standardized coefficient of 0.66. Whereas the correlation between negative symptoms and positive self-concept was -0.32 at t0, it increased marginally to -0.44 at t1. The test of models with negative symptoms and interpersonal self-concepts result in similar results as shown in Table 2. Incorporating treatment group in the model (see Supplementary Figure S1), did not change these results. In summary, for negative symptoms our data did not support either the scar or the vulnerability model.
Table 2.
Goodness-of-fit indices of the tested models and model comparisons.
| Chi-sq | Chi-sq/df | CFI | TLI | RMSEA | BIC | AIC | Coefficient (SE; P) | |
|---|---|---|---|---|---|---|---|---|
| Threshold for good models | n.a. | ≤2 | ≥0.950 | ≥0.950 | ≤0.050 | l.v.p. | l.v.p. | P < 0.05 |
| Negative Symptoms | ||||||||
| Positive self-concept | ||||||||
| Unrestricted model (df = 26) | 22.05; P = 0.63 | 0.882 | 1.000 | 1.004 | 0.000 | 174.31 | 82.05 | |
| Scar model (df = 27) | 22.18; P = 0.68 | 0.853 | 1.000 | 1.005 | 0.000 | 169.36 | 80.18 | -0.10 (0.07; 0.128) |
| Vulnerability model (df = 27) | 24.35; P = 0.56 | 0.937 | 1.000 | 1.002 | 0.000 | 171.53 | 82.35 | 0.02 (0.08; 0.719) |
| Restricted model (df = 28) | 24.39; P = 0.61 | 0.903 | 1.000 | 1.003 | 0.000 | 166.50 | 80.39 | |
| Interpersonal self-concept | ||||||||
| Unrestricted model (df = 26) | 25.78; P = 0.42 | 1.031 | 0.999 | 0.999 | 0.014 | 178.03 | 85.78 | |
| Scar model (df = 27) | 27.17; P = 0.40 | 1.045 | 0.999 | 0.998 | 0.017 | 174.35 | 85.17 | -0.08 (0.08; 0.232) |
| Vulnerability model (df = 27) | 25.78; P = 0.48 | 0.992 | 1.000 | 1.000 | 0.000 | 172.96 | 83.78 | 0.01 (0.08; 0.943) |
| Restricted model (df = 28) | 27.18; P = 0.45 | 1.007 | 1.000 | 1.000 | 0.006 | 169.28 | 83.18 | |
| Neurocognition | ||||||||
| Positive self-concept | ||||||||
| Unrestricted model (df = 26) | 27.54; P = 0.28 | 1.145 | 0.997 | 0.995 | 0.030 | 184.87 | 89.54 | |
| Scar model (df = 27) | 27.90; P = 0.31 | 1.116 | 0.998 | 0.996 | 0.027 | 180.16 | 87.90 | 0.26 (0.02; 0.008) |
| Vulnerability model (df = 27) | 38.00; P = 0.05 | 1.520 | 0.989 | 0.981 | 0.057 | 190.25 | 97.99 | -0.05 (0.63; 0.563) |
| Restricted model (df = 28) | 38.14; P = 0.06 | 1.467 | 0.990 | 0.983 | 0.054 | 185.32 | 96.14 | |
| Interpersonal self-concept | ||||||||
| Unrestricted model (df = 26) | 25.63; P = 0.37 | 1.125 | 0.998 | 0.996 | 0.020 | 183.91 | 87.63 | |
| Scar model (df = 27) | 26.43; P = 0.39 | 1.096 | 0.998 | 0.997 | 0.019 | 179.61 | 86.43 | 0.25 (0.02; 0.02) |
| Vulnerability model (df = 27) | 31.54; P = 0.17 | 1.218 | 0.992 | 0.985 | 0.040 | 184.72 | 91.54 | -0.07 (0.80; 0.39) |
| Restricted model (df = 28) | 32.27; P = 0.19 | 1.195 | 0.992 | 0.987 | 0.038 | 180.31 | 90.24 | |
| Paranoia | ||||||||
| Positive self-concept | ||||||||
| Unrestricted model (df = 26) | 28.57; P = 0.24 | 1.191 | 0.996 | 0.992 | 0.035 | 185.90 | 90.57 | |
| Scar model (df = 27) | 31.21; P = 0.18 | 1.248 | 0.994 | 0.990 | 0.040 | 183.46 | 91.20 | 0.03 (0.07; 0.714) |
| Vulnerability model (df = 27) | 28.70; P = 0.28 | 1.148 | 0.997 | 0.994 | 0.030 | 180.95 | 88.70 | -0.18 (0.15; 0.097) |
| Restricted model (df = 28) | 31.30; P = 0.22 | 1.204 | 0.995 | 0.992 | 0.036 | 178.48 | 89.30 | |
| Interpersonal self-concept | ||||||||
| Unrestricted model (df = 26) | 29.41; P = 0.21 | 1.225 | 0.992 | 0.985 | 0.038 | 186.74 | 91.41 | |
| Scar model (df = 27) | 34.02; P = 0.11 | 1.361 | 0.987 | 0.976 | 0.048 | 186.28 | 94.02 | 0.01 (0.08; 0.904) |
| Vulnerability model (df = 27) | 29.42; P = 0.25 | 1.117 | 0.994 | 0.988 | 0.033 | 181.68 | 89.42 | -0.25 (0.14; 0.029) |
| Restricted model (df = 28) | 34.03; P = 0.13 | 1.309 | 0.988 | 0.980 | 0.044 | 181.21 | 92.03 |
Chi-sq, discrepancy chi-squared statistic; df, degrees of freedom; Chi-sq/df, normed chi-squared statistic; Coefficient, the standardized estimates in the unrestricted model; SE, Standard error of the coefficient; P, significance level of the coefficient; CFI, Comparative Fit Index; TLI, Tucker-Lewis Index; RMSEA, Root Mean Squared Error of Approximation; BIC, Bayes Information Criterion; l.v.p., lower values preferred (only for model comparisons).
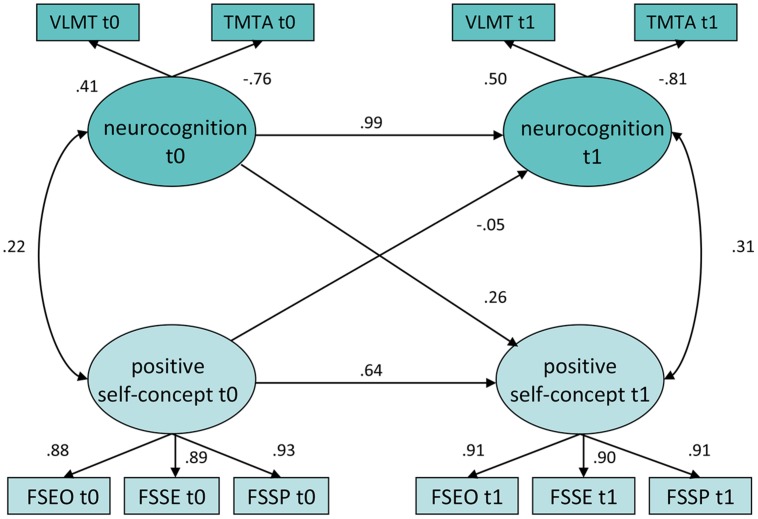
With regard to neurocognition, the scar model was identified as the best model both for positive and interpersonal self-concepts. These results are presented in Table 2 and Figure 2. Neurocognition is highly stable over time indicated by a high auto-regression coefficient. The standardized coefficient from neurocognition at baseline to positive self-concept at follow-up representing the scar model is 0.26 with p = 0.008. In nested model comparison for positive self-concept, the difference between the restricted model and the scar model is significant, indicating a substantially increased model fit for the scar model than for the restricted model (df = 1; ΔX2 = 10.24; p = 0.001). For interpersonal self-concepts the same pattern is depicted; the scar path coefficient (0.25; p > 0.019) and the difference to the restricted model are both significant (df = 1; ΔX2 = 5.80; p = 0.016). When treatment group is added to the model (see Supplementary Figure S2), the relationship between neurocognition at t0 and positive self-concept in t1 remains significant (p = 0.008). In summary, for neurocognition the data supported the scar hypothesis.
FIGURE 2.
Unrestricted longitudinal model of Positive Self-concept and Neurocognition. Rectangles indicate observed indicator variables. Ovals indicate unobserved latent variables. Figures on single-headed arrows indicate standardized regression weights; figures on double-headed arrows correlations. Error variables are omitted. TMT A, Trail Making Test Trail A; (VLMT) Verbaler Lern und Merkfähigkeitstest; Frankfurt Self-Concept Scales: (FSGA, general achievement; FSSP, solving daily problems; FSSE, self-esteem). The overall model fit was χ2 27.538, df = 24, P < 0.280; CFI = 0.997, TLI = 0.995, RMSEA = 0.030 (0.000 – 0.074).
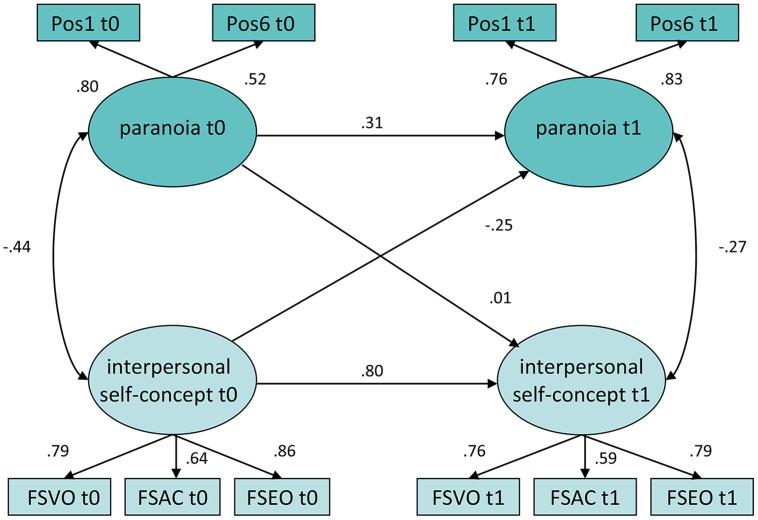
For paranoia, the vulnerability model showed better fitting indices. The unrestricted model for interpersonal self-concepts is presented in Figure 3. Whereas the concurrent correlation between paranoia and self-concepts is -0.44 at baseline, it decreases to -0.27 12 months later. The stability of paranoia is smaller than for negative symptoms or neurocognition with a standardized coefficient of 0.31. The standardized coefficient from interpersonal self-concept at baseline to paranoia at follow-up representing the vulnerability model is -0.25 with p < 0.029. Moreover the chi-square statistics of the vulnerability model fits significantly superior than the restricted model (df = 1; ΔX2 = 4.60; p = 0.032). Although the results were fairly comparable for the models with positive self-concept, the coefficient representing the vulnerability model did not reach the threshold for strict statistical significance (p < 0.097). As well, the chi-square statistics between the vulnerability model and the restricted model did not differ significantly, indicating no significant incremental fit for the vulnerability model with positive self-concepts.(df = 1; X2 = 2.17; p = 0.141). When treatment group is added to the model (see Supplementary Figure S3), the relationship between paranoid delusions at t0 and interpersonal self-concept in t1 remains significant (p = 0.031). In summary, for paranoia the data supported the vulnerability model, particularly with regard to interpersonal self-concept.
FIGURE 3.
Unrestricted longitudinal model of interpersonal self-concept and paranoia. Rectangles indicate observed indicator variables. Ovals indicate unobserved latent variables. Figures on single-headed arrows indicate standardized regression weights; figures on double-headed arrows correlations. Error variables are omitted. Pos1, PANNS P01 delusions; Pos06, PANSS P6 suspiciousness/persecution; Frankfurt Self-Concept Scales: (FSVO, valued by others; FSAC, ability to make contact with other people, FSEO, emotions and relations to others). The overall model fit was χ2 = 29.41, df = 24, P = 0.21; CFI = 0.992, TLI = 0.985, RMSEA = 0.038 (0.000 – 0.078).
Discussion
Cognitive models on negative symptoms, positive symptoms, and neurocognition can inform treatment development as they shed light on the development and maintenance of symptoms (Garety et al., 2001, 2007; Freeman et al., 2002; Rector et al., 2005; Kesting and Lincoln, 2013). In order to obtain a robust evidence base, these models need to be tested by different methodologies including epidemiological studies (Krabbendam et al., 2002; Fowler et al., 2006), experimental data with healthy controls, or clinical samples (Kesting et al., 2013), as well as longitudinal data from clinical samples like the study presented in this article.
Negative Symptoms
Cognitive models of negative symptoms (Rector et al., 2005) as well as the psychotherapeutic rationale (Staring et al., 2013) rely on defeatist beliefs and negative self-concepts. Most studies use measures of defeatist attitudes and expectancies such as measured by the dysfunctional attitude scale (Beck et al., 2013). In our study, negative symptoms were associated concurrently with self-concepts as predicted by the cognitive model of negative symptoms. Contrary to our expectation, self-concept at pre-treatment did not predict negative symptoms after 12 months. The construct of negative symptoms has been stable, thus there was change in individuals and in the mean, but relative low change in the individual residuals. However, the longitudinal analysis did not support an influence, like found in first-episode patients (Palmier-Claus et al., 2011a). As in our study the time between t0 and t1 was 12 months, multiple causation might have influenced negative symptoms as well as self-concepts during this period. The variance in our sample is limited due to the inclusion criteria; this might have limited the covariances as well. For further research a shorter duration of measurement intervals is supposed to test.
Neurocognition
As hypothesized, neurocognitive functioning at baseline predicted positive self-concept after 12 months. Yet, self-concepts are not in the focus of interest in research on neurocognition in people with psychosis. In the general population there is strong evidence that people can estimate their cognitive abilities well (Freund and Kasten, 2012). Our findings support the scar model. Possibly service-users perceive the loss of memory function and processing speed during the course of the disorder and integrate them in a negative self-concept. In concurrent analyses of people with schizophrenia, defeatist beliefs operated as a mediator between neurocognitive impairments and negative symptoms (Grant and Beck, 2009). These results demonstrate the importance of functional illness-concepts. In a cross-sectional model of visual perception, social cognition, and social functioning the same mediating effect of negative beliefs about the self was found (Green et al., 2012). It is plausible that more negative self-concepts may lead to negative symptoms due to the perception of neurocognitive deficits and maladaptive illness-concepts.
Paranoid Delusions
In our study, evidence was found for a prediction of paranoia after 12 months by interpersonal self-concept at pre-treatment. Other researchers yielded empirical support for the vulnerability model in paranoid delusions was as well (Fowler et al., 2012; Kesting and Lincoln, 2013). For example, in daily life reports of fluctuations in self-esteem predicted the development of paranoia (Thewissen et al., 2008). Some cross-sectional studies found positive correlations between self-concepts and positive symptoms (Barrowclough et al., 2003) or paranoid delusions (Smith et al., 2006). In the data presented above the stability of paranoid delusions was weak, primarily indicating that most people involved in this trial had only modest paranoid delusions at entry but some of them relapsed in the course of the study. The scales “negative self” and “negative others” of the Brief Core Schema Scale (BCSS; Fowler et al., 2006) have shown positive correlations with paranoid delusions (Freeman et al., 2013; Garety et al., 2013). There is a slight difference between the “negative others” scale in the BCSS and the interpersonal self-concepts measured in the FSKN. Whereas the BCSS assesses appraised threat from others, the items used in our study are formulated as self-concepts, i.e., how the person is thinking about itself in social relationships. The three scales which has been used to measure interpersonal self-concepts reflect the feelings of being valued by others, trustworthy for others and competent in making contacts. In the BCSS one item is for instance: “Other people are supportive,” whereas in the FSKN a corresponding inverted item is “With many of my friends, I’m afraid that when I need them they won’t be there for me.” In our study, the more global positive self-concepts did not support the vulnerability model; the path from positive self-concept at baseline to paranoia at follow-up did not reach statistical significance. The long interval of 12 months, the limited variance in paranoia and the sample size may have caused these non-significant findings. Lincoln et al. (2010) found although that paranoia was not associated with self-esteem but with interpersonal self-concepts. In our study, interpersonal self-concepts predicted paranoia too, hence when psychological models of paranoia are studied, interpersonal self-concepts in addition to more general positive, or negative self-concepts should be considered. Bentall et al. (2001) have hypothesized that people with tendencies to paranoid delusions avoid negative beliefs about the self, by attributing threatening events to other persons. Interpersonal self-concepts could reflect not only the self though how we see ourselves in social context and how we see other people in relation to us. Our findings support the model of persecutory delusions of Garety et al. (2001) and Freeman et al. (2002) who proposed that certain beliefs about the self and others are important factors in the development of persecutory delusions.
Clinical Implications
There may be some clinical implications for our findings, assuming that cognitive behavioral therapy for psychosis is an effective treatment, one mechanism of change could be the improvement of self-concepts. Interpersonal self-concepts could be influenced by the quality of the therapeutic alliance in psychotherapy, which is indeed a common effect in the treatment of schizophrenia (Frank and Gunderson, 1990) as well as in every therapeutic intervention (Martin et al., 2000). We can speculate that in many therapeutic settings interpersonal self-concepts are influenced as the therapeutic relationship might be a positive model in terms of trustworthiness, reliability, and acceptance. The possible change in the interpersonal self-concept due to the therapy could be one explanation for the reduction in positive symptoms in supportive therapies (Penn et al., 2004) and for symptom changes during therapy even when they are not directly addressed. When neurocognitive deficits are seen in people with schizophrenia, interventions aiming at compensating deficits and modifying dysfunctional attitudes and self-concepts could be helpful in reducing negative performance expectancies and negative symptoms. When neurocognitive deficits are present, minimizing the deficits is crucial and partly possible (Wykes et al., 2011). The awareness of cognitive impairments is negatively correlated with self-esteem (Cella et al., 2014), therefore when neurocognition does not remit, service-users should be helped in accepting and destigmatizing limits caused by symptoms. For this purpose psychological interventions could be helpful, like combinations of cognitive therapy, and cognitive remediation (Greenwood et al., 2005; Wykes et al., 2011). For this purpose cognitive intervention could focus more on interpersonal self-concepts and narrative enhancements (Yanos et al., 2011) to protect people with schizophrenia from relapse to paranoid delusions.
Strengths and Limitations
A main strength of our study is that patients have been investigated and followed-up over a period of 12 months. From the 198 patients interviewed at baseline we had almost complete data from 160 participants 12 months later, indicating a low risk of bias due to informative censoring. Whereas other studies showed effects for some hours (Thewissen et al., 2008) up to 9 months (Fowler et al., 2012), in our analysis the interval was 12 months. The relatively small coefficients have to be interpreted in this context.
There are some limitations in the study. First, the study is part of randomized controlled trial with systematic therapy regime. We tried to rule out influences from treatment statistically; anyway a sample without explicit psychotherapy would be more adequate to test the hypotheses. Second, the tested models had to be simple, because the sample size of 160 participants limits more complex structural equation models (e.g., a single model including all tested constructs and associations simultaneously). Furthermore, our sample consists of patients with predominantly negative symptoms and relatively weak positive symptoms, and thus might limit the possibility of generalization. On the other hand a strength of the study is to include a relative large sample of people with distinct inclusion criteria and a relative homogenous phenotype. Neurocognition as measured in this study consisted only of verbal memory and processing speed, other important domains like executive functions or verbal fluency were not included. We had other measures in the dataset available, but we could not reach appropriate model fits when including measures of attention and problem solving. Nevertheless we included two good established markers for neurocognition in our analysis. The Hopkins Verbal Learning Test (a similar verbal learning test as we used) and the TMT are included in the MATRICS-Battery, both are correlated with functioning and have the highest ratings for practicability by experts (Nuechterlein et al., 2008).
Conclusion
We found some evidence for the importance of self-concepts in the course of symptoms in people with schizophrenia. We could find evidence for the scar model in neurocognition: global positive self-concepts as well as interpersonal self-concepts seem to be endangered when neurocognitive impairments occur. This study provides further evidence for a vulnerability model of paranoia: the presence of a negative interpersonal self-concept is a risk factor for paranoid delusions. This result is consistent with theories proposing a relationship between negative social experiences, mood, self-concepts, and paranoia (Garety et al., 2001; Freeman, 2007; Kesting and Lincoln, 2013).
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
This work was supported by the German Research Foundation (Deutsche Forschungsgemeinschaft, grants Kl 1179/2-1 and Kl 1179/3-1). We acknowledge support by Deutsche Forschungsgemeinschaft and Open Access Publishing Fund of University of Tübingen. We thank Johannes Harbort, Michael Ruch, Hanna Smoltczyk, and Maia Weickert for their contribution in the assessments.
Supplementary Material
The Supplementary Material for this article can be found online at: http://journal.frontiersin.org/article/10.3389/fpsyg.2015.00917
References
- Barrowclough C., Tarrier N., Humphreys L., Ward J., Gregg L., Andrews B. (2003). Self-esteem in schizophrenia: relationships between self-evaluation, family attitudes, and symptomatology. J. Abnorm. Psychol. 112 92–99. 10.1037/0021-843X.112.1.92 [DOI] [PubMed] [Google Scholar]
- Beck A. T., Grant P. M., Huh G. A., Perivoliotis D., Chang N. A. (2013). Dysfunctional attitudes and expectancies in deficit syndrome schizophrenia. Schizophr. Bull. 39 43–51. 10.1093/schbul/sbr040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bentall R. P., Corcoran R., Howard R., Blackwood N., Kinderman P. (2001). Persecutory delusions: a review and theoretical integration. Clin. Psychol. Rev. 21 1143–1192. 10.1016/S0272-7358(01)00106-4 [DOI] [PubMed] [Google Scholar]
- Bentall R. P., Kinderman P., Kaney S. (1994). The self, attributional processes and abnormal beliefs: towards a model of persecutory delusions. Behav. Res. Ther. 32 331–341. 10.1016/0005-7967(94)90131-7 [DOI] [PubMed] [Google Scholar]
- Bora E., Murray R. M. (2014). Meta-analysis of cognitive deficits in ultra-high risk to psychosis and first-episode psychosis: do the cognitive deficits progress over, or after, the onset of psychosis? Schizophr. Bull. 40 744–755. 10.1093/schbul/sbt085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bortolon C., Capdevielle D., Boulenger J. P., Gely-Nargeot M. C., Raffard S. (2013). Early maladaptive schemas predict positive symptomatology in schizophrenia: a cross-sectional study. Psychiatry Res. 209 361–366. 10.1016/j.psychres.2013.03.018 [DOI] [PubMed] [Google Scholar]
- Bowie C. R., Depp C., Mcgrath J. A., Wolyniec P., Mausbach B. T., Thornquist M. H., et al. (2010). Prediction of real-world functional disability in chronic mental disorders: a comparison of schizophrenia and bipolar disorder. Am. J. Psychiatry 167 1116–1124. 10.1176/appi.ajp.2010.09101406 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cavelti M., Beck E. M., Kvrgic S., Kossowsky J., Vauth R. (2012a). The role of subjective illness beliefs and attitude toward recovery within the relationship of insight and depressive symptoms among people with schizophrenia spectrum disorders. J. Clin. Psychol. 68 462–476. 10.1002/jclp.20872 [DOI] [PubMed] [Google Scholar]
- Cavelti M., Kvrgic S., Beck E. M., Rusch N., Vauth R. (2012b). Self-stigma and its relationship with insight, demoralization, and clinical outcome among people with schizophrenia spectrum disorders. Compr. Psychiatry 53 468–479. 10.1016/j.comppsych.2011.08.001 [DOI] [PubMed] [Google Scholar]
- Cella M., Swan S., Medin E., Reeder C., Wykes T. (2014). Metacognitive awareness of cognitive problems in schizophrenia: exploring the role of symptoms and self-esteem. Psychol. Med. 44 469–476. 10.1017/S0033291713001189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deusinger I. M. (1986). Die Frankfurter Selbstkonzeptskalen (FSKN). Göttingen: Hogrefe. [Google Scholar]
- Erickson M. A., Lysaker P. H. (2012). Self-esteem and insight as predictors of symptom change in schizophrenia: a longitudinal study. Clin. Schizophr. Relat. Psychoses 6 69–75. 10.3371/CSRP.6.2.4 [DOI] [PubMed] [Google Scholar]
- Fowler D., Freeman D., Smith B., Kuipers E., Bebbington P., Bashforth H., et al. (2006). The brief core schema scales (BCSS): psychometric properties and associations with paranoia and grandiosity in non-clinical and psychosis samples. Psychol. Med. 36 749–759. 10.1017/S0033291706007355 [DOI] [PubMed] [Google Scholar]
- Fowler D., Hodgekins J., Garety P., Freeman D., Kuipers E., Dunn G., et al. (2012). Negative cognition, depressed mood, and paranoia: a longitudinal pathway analysis using structural equation modeling. Schizophr. Bull. 38 1063–1073. 10.1093/schbul/sbr019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frank A. F., Gunderson J. G. (1990). The role of the therapeutic alliance in the treatment of schizophrenia - relationship to course and outcome. Arch. Gen. Psychiatry 47 228–236. 10.1001/archpsyc.1990.01810150028006 [DOI] [PubMed] [Google Scholar]
- Freeman D. (2007). Suspicious minds: the psychology of persecutory delusions. Clin. Psychol. Rev. 27 425–457. 10.1016/j.cpr.2006.10.004 [DOI] [PubMed] [Google Scholar]
- Freeman D., Dunn G., Fowler D., Bebbington P., Kuipers E., Emsley R., et al. (2013). Current paranoid thinking in patients with delusions: the presence of cognitive-affective biases. Schizophr. Bull. 39 1281–1287. 10.1093/schbul/sbs145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freeman D., Garety P. A., Kuipers E., Fowler D., Bebbington P. E. (2002). A cognitive model of persecutory delusions. Br. J. Clin. Psychol. 41 331–347. 10.1348/014466502760387461 [DOI] [PubMed] [Google Scholar]
- Freund P. A., Kasten N. (2012). How smart do you think you are? A meta-analysis on the validity of self-estimates of cognitive ability. Psychol. Bull. 138 296–321. 10.1037/a0026556 [DOI] [PubMed] [Google Scholar]
- Garety P. A., Bebbington P., Fowler D., Freeman D., Kuipers E. (2007). Implications for neurobiological research of cognitive models of psychosis: a theoretical paper. Psychol. Med. 37 1377–1391. 10.1017/S003329170700013X [DOI] [PubMed] [Google Scholar]
- Garety P. A., Gittins M., Jolley S., Bebbington P., Dunn G., Kuipers E., et al. (2013). Differences in cognitive and emotional processes between persecutory and grandiose delusions. Schizophr. Bull. 39 629–639. 10.1093/schbul/sbs059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garety P. A., Kuipers E., Fowler D., Freeman D., Bebbington P. E. (2001). A cognitive model of the positive symptoms of psychosis. Psychol. Med. 31 189–195. 10.1017/S0033291701003312 [DOI] [PubMed] [Google Scholar]
- Gaudiano B. A., Herbert J. D. (2006). Acute treatment of inpatients with psychotic symptoms using acceptance and commitment therapy: pilot results. Behav. Res. Ther. 44 415–437. 10.1016/j.brat.2005.02.007 [DOI] [PubMed] [Google Scholar]
- Grant P. M., Beck A. T. (2009). Defeatist beliefs as a mediator of cognitive impairment, negative symptoms, and functioning in schizophrenia. Schizophr. Bull. 35 798–806. 10.1093/schbul/sbn008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green M. F., Hellemann G., Horan W. P., Lee J., Wynn J. K. (2012). From perception to functional outcome in schizophrenia modeling the role of ability and motivation. Arch. Gen. Psychiatry 69 1216–1224. 10.1001/archgenpsychiatry.2012.652 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green M. F., Kern R. S., Braff D. L., Mintz J. (2000). Neurocognitive deficits and functional outcome in schizophrenia: are we measuring the “right stuff”? Schizophr. Bull. 26 119–136. 10.1093/oxfordjournals.schbul.a033430 [DOI] [PubMed] [Google Scholar]
- Greenwood K. E., Landau S., Wykes T. (2005). Negative symptoms and specific cognitive impairments as combined targets for improved functional outcome within cognitive remediation therapy. Schizophr. Bull. 31 910–921. 10.1093/schbul/sbi035 [DOI] [PubMed] [Google Scholar]
- Harvey P. D., Keefe R. S. E. (2001). Studies of cognitive change in patients with schizophrenia following novel antipsychotic treatment. Am. J. Psychiatry 158 176–184. 10.1176/appi.ajp.158.2.176 [DOI] [PubMed] [Google Scholar]
- Hesse K., Kriston L., Mehl S., Wittorf A., Wiedemann W., Wolwer W., et al. (2015). The vicious cycle of family atmosphere, interpersonal self-concepts, and paranoia in schizophrenia-a longitudinal study. Schizophr. Bull. 10.1093/schbul/sbv055 [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kesting M. L., Bredenpohl M., Klenke J., Westermann S., Lincoln T. M. (2013). The impact of social stress on self-esteem and paranoid ideation. J. Behav. Ther. Exp. Psychiatry 44 122–128. 10.1016/j.jbtep.2012.07.010 [DOI] [PubMed] [Google Scholar]
- Kesting M. L., Lincoln T. M. (2013). The relevance of self-esteem and self-schemas to persecutory delusions: a systematic review. Compr. Psychiatry 54 766–789. 10.1016/j.comppsych.2013.03.002 [DOI] [PubMed] [Google Scholar]
- Khan A., Lindenmayer J. P., Opler M., Yavorsky C., Rothman B., Lucic L. (2013). A new integrated negative symptom structure of the positive and negative syndrome scale (PANSS) in schizophrenia using item response analysis. Schizophr. Res. 150 185–196. 10.1016/j.schres.2013.07.007 [DOI] [PubMed] [Google Scholar]
- Kim J. H., Kim S. Y., Lee J., Oh K. J., Kim Y. B., Cho Z. H. (2012). Evaluation of the factor structure of symptoms in patients with schizophrenia. Psychiatry Res. 197 285–289. 10.1016/j.psychres.2011.10.006 [DOI] [PubMed] [Google Scholar]
- Klein D. N., Kotov R., Bufferd S. J. (2011). Personality and depression: explanatory models and review of the evidence. Annu. Rev. Clin. Psychol. 7 269–295. 10.1146/annurev-clinpsy-032210-104540 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kline R. B. (2011). Principles and Practice of Structural Equation Modeling. New York, NY: Guilford. [Google Scholar]
- Klingberg S., Wittorf A., Herrlich J., Wiedemann G., Meisner C., Buchkremer G., et al. (2009). Cognitive behavioural treatment of negative symptoms in schizophrenia patients: study design of the TONES study, feasibility and safety of treatment. Eur. Arch. Psychiatry Clin. Neurosci. 259 149–154. 10.1007/s00406-009-0047-8 [DOI] [PubMed] [Google Scholar]
- Klingberg S., Wittorf A., Wiedemann G. (2006). Disorganization and cognitive impairment in schizophrenia: independent symptom dimensions? Euro. Arch. Psychiatry Clin. Neurosci. 256 532–540. 10.1007/s00406-006-0704-0 [DOI] [PubMed] [Google Scholar]
- Klingberg S., Wolwer W., Engel C., Wittorf A., Herrlich J., Meisner C., et al. (2011). Negative symptoms of schizophrenia as primary target of cognitive behavioral therapy: results of the randomized clinical TONES study. Schizophr. Bull. 37 98–110. 10.1093/schbul/sbr073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krabbendam L., Janssen I., Bak M., Bijl R. V., De Graaf R., Van Os J. (2002). Neuroticism and low self-esteem as risk factors for psychosis. Soc. Psychiatry Psychiatr. Epidemiol. 37 1–6. 10.1007/s127-002-8207-y [DOI] [PubMed] [Google Scholar]
- Lewinsohn P. M., Steinmetz J. L., Larson D. W., Franklin J. (1981). Depression-related cognitions: antecedent or consequence? J. Abnorm. Psychol. 90 213–219. 10.1037/0021-843X.90.3.213 [DOI] [PubMed] [Google Scholar]
- Lincoln T. M., Mehl S., Kesting M. L., Rief W. (2011). Negative symptoms and social cognition: identifying targets for psychological interventions. Schizophr. Bull. 37(Suppl. 2), S23–S32. 10.1093/schbul/sbr066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lincoln T. M., Mehl S., Ziegler M., Kesting M. L., Exner C., Rief W. (2010). Is fear of others linked to an uncertain sense of self? The relevance of self-worth, interpersonal self-concepts, and dysfunctional beliefs to paranoia. Behav. Ther. 41 187–197. 10.1016/j.beth.2009.02.004 [DOI] [PubMed] [Google Scholar]
- Lux S., Helmstaedter C., Elger C. E. (1999). Normative study on the “Verbaler Lern- und Merkfahigkeitstest” (VLMT). Diagnostica 45 205–211. 10.1026//0012-1924.45.4.205 [DOI] [Google Scholar]
- Lysaker P. H., Roe D., Yanos P. T. (2007). Toward understanding the insight paradox: internalized stigma moderates the association between insight and social functioning, hope, and self-esteem among people with schizophrenia spectrum disorders. Schizophr. Bull. 33 192–199. 10.1093/schbul/sbl016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin D. J., Garske J. P., Davis M. K. (2000). Relation of the therapeutic alliance with outcome and other variables: a meta-analytic review. J. Consult. Clin. Psychol. 68 438–450. 10.1037/0022-006X.68.3.438 [DOI] [PubMed] [Google Scholar]
- Moritz S., Andreou C., Schneider B. C., Wittekind C. E., Menon M., Balzan R. P., et al. (2014). Sowing the seeds of doubt: a narrative review on metacognitive training in schizophrenia. Clin. Psychol. Rev. 34 358–366. 10.1016/j.cpr.2014.04.004 [DOI] [PubMed] [Google Scholar]
- Nuechterlein K. H., Green M. F., Kern R. S., Baade L. E., Barch D. M., Cohen J. D., et al. (2008). The MATRICS consensus cognitive battery, part 1: test selection, reliability, and validity. Am. J. Psychiatry 165 203–213. 10.1176/appi.ajp.2007.07010042 [DOI] [PubMed] [Google Scholar]
- Palmier-Claus J., Dunn G., Drake R., Lewis S. (2011a). The negative and positive self: a longitudinal study examining self-esteem, paranoia and negative symptoms in individuals with first-episode psychosis. Early Interv. Psychiatry 5 150–155. 10.1111/j.1751-7893.2010.00250.x [DOI] [PubMed] [Google Scholar]
- Palmier-Claus J. E., Dunn G., Morrison A. P., Lewis S. W. (2011b). The role of metacognitive beliefs in stress sensitisation, self-esteem variability, and the generation of paranoia. Cogn. Neuropsychiatry 16 530–546. 10.1080/13546805.2011.561583 [DOI] [PubMed] [Google Scholar]
- Penn D. L., Mueser K. T., Tarrier N., Gloege A., Cather C., Serrano D., et al. (2004). Supportive therapy for schizophrenia: possible mechanisms and implications for adjunctive psychosocial treatments. Schizophr. Bull. 30 101–112. 10.1093/oxfordjournals.schbul.a007055 [DOI] [PubMed] [Google Scholar]
- Rector N. A., Beck A. T., Stolar N. (2005). The negative symptoms of schizophrenia: a cognitive perspective. Can. J. Psychiatry 50 247–257. [DOI] [PubMed] [Google Scholar]
- Reichenberg A., Harvey P. D., Bowie C. R., Mojtabai R., Rabinowitz J., Heaton R. K., et al. (2009). Neuropsychological function and dysfunction in schizophrenia and psychotic affective disorders. Schizophr. Bull. 35 1022–1029. 10.1093/schbul/sbn044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanchez P., Pena J., Bengoetxea E., Ojeda N., Elizagarate E., Ezcurra J., et al. (2014). Improvements in negative symptoms and functional outcome after a new generation cognitive remediation program: a randomized controlled trial. Schizophr. Bull. 40 707–715. 10.1093/schbul/sbt057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith B., Fowler D. G., Freeman D., Bebbington P., Bashforth H., Garety P., et al. (2006). Emotion and psychosis: links between depression, self-esteem, negative schematic beliefs and delusions and hallucinations. Schizophr. Res. 86 181–188. 10.1016/j.schres.2006.06.018 [DOI] [PubMed] [Google Scholar]
- Sowislo J. F., Orth U. (2013). Does low self-esteem predict depression and anxiety? A meta-analysis of longitudinal studies. Psychol. Bull. 139 213–240. 10.1037/a0028931 [DOI] [PubMed] [Google Scholar]
- Staring A. B. P., Ter Huurne M. B., van der Gaag M. (2013). Cognitive behavioral therapy for negative symptoms (CBT-n) in psychotic disorders: a pilot study. J. Behav. Ther. Exp. Psychiatry 44 300–306. 10.1016/j.jbtep.2013.01.004 [DOI] [PubMed] [Google Scholar]
- Staring A. B. P., van der Gaag M., Van Den Berge M., Duivenvoorden H. J., Mulder C. L. (2009). Stigma moderates the associations of insight with depressed mood, low self-esteem, and low quality of life in patients with schizophrenia spectrum disorders. Schizophr. Res. 115 363–369. 10.1016/j.schres.2009.06.015 [DOI] [PubMed] [Google Scholar]
- Tai S., Turkington D. (2009). The evolution of cognitive behavior therapy for schizophrenia: current practice and recent developments. Schizophr. Bull. 35 865–873. 10.1093/schbul/sbp080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thewissen V., Bentall R. P., Lecomte T., Van Os J., Myin-Germeys I. (2008). Fluctuations in self-esteem and paranoia in the context of daily life. J. Abnorm. Psychol. 117 143–153. 10.1037/0021-843X.117.1.143 [DOI] [PubMed] [Google Scholar]
- Thewissen V., Bentall R. P., Oorschot M., A Campo J., Van Lierop T., Van Os J., et al. (2011). Emotions, self-esteem, and paranoid episodes: an experience sampling study. Br. J. Clin. Psychol. 50 178–195. 10.1348/014466510X508677 [DOI] [PubMed] [Google Scholar]
- Tombaugh T. N. (2004). Trail making test A and B: normative data stratified by age and education. Arch. Clin. Neuropsychol. 19 203–214. 10.1016/S0887-6177(03)00039-8 [DOI] [PubMed] [Google Scholar]
- Vracotas N., Iyer S. N., Joober R., Malla A. (2012). The role of self-esteem for outcome in first-episode psychosis. Int. J. Soc. Psychiatry 58 41–46. 10.1177/0020764010382698 [DOI] [PubMed] [Google Scholar]
- Weinberg D., Shahar G., Noyman G., Davidson L., Mcglashan T. H., Fennig S. (2012). Role of the self in schizophrenia: a multidimensional examination of short-term outcomes. Psychiatry 75 285–297. 10.1521/psyc.2012.75.3.285 [DOI] [PubMed] [Google Scholar]
- Wittorf A., Klingberg S., Wiedemann G. (2004). Secondary verbal memory: a potential endophenotype of schizophrenia. J. Psychiatry Res. 38 601–612. 10.1016/j.jpsychires.2004.03.005 [DOI] [PubMed] [Google Scholar]
- Wittorf A., Wiedemann G., Buchkremer G., Klingberg S. (2010). Quality and correlates of specific self-esteem at the beginning stabilisation phase of schizophrenia. Psychiatry Res. 179 130–138. 10.1016/j.psychres.2009.03.024 [DOI] [PubMed] [Google Scholar]
- Wykes T., Huddy V., Cellard C., Mcgurk S. R., Czobor P. (2011). A meta-analysis of cognitive remediation for schizophrenia: methodology and effect sizes. Am. J. Psychiatry 168 472–485. 10.1176/appi.ajp.2010.10060855 [DOI] [PubMed] [Google Scholar]
- Yanos P. T., Moos R. H. (2007). Determinants of functioning and well-being among individuals with schizophrenia: an integrated model. Clin. Psychol. Rev. 27 58–77. 10.1016/j.cpr.2005.12.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yanos P. T., Roe D., Lysaker P. H. (2011). Narrative enhancement and cognitive therapy: a new group-based treatment for internalized stigma among persons with severe mental illness. Int. J. Group Psychother. 61 577–595. 10.1521/ijgp.2011.61.4.576 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yesufu-Udechuku A., Harrison B., Mayo-Wilson E., Young N., Woodhams P., Shiers D., et al. (2015). Interventions to improve the experience of caring for people with severe mental illness: systematic review and meta-analysis. Br. J. Psychiatry 206 268–274. 10.1192/bjp.bp.114.147561 [DOI] [PubMed] [Google Scholar]
- Zubin J., Spring B. (1977). Vulnerability - a new view of schizophrenia. J. Abnorm. Psychol. 86 103–126. 10.1037/0021-843X.86.2.103 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.