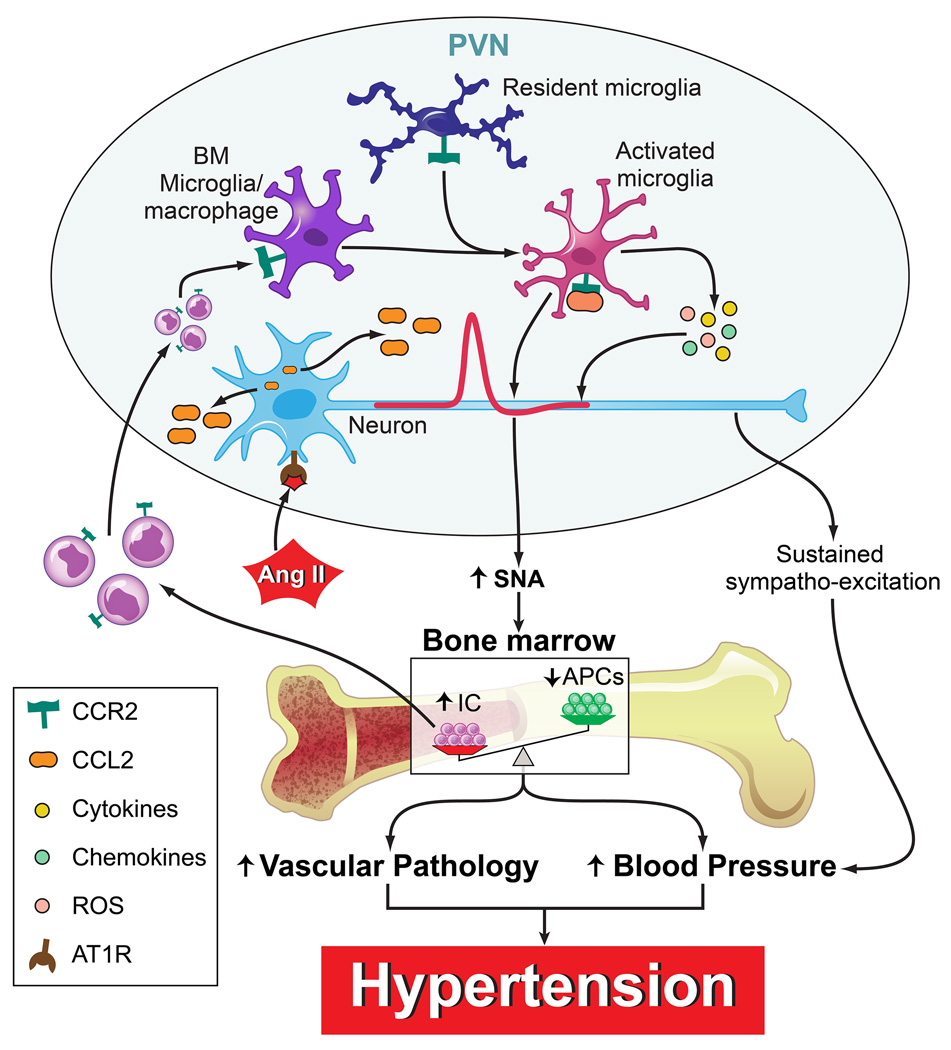
Figure 8. Proposed hypothesis for the extravasation of bone marrow cells to the hypothalamic paraventricular nucleus (PVN) and the involvement of neuroinflammation in hypertension (HTN).
Pro-hypertensive signals such as angiotensin II (Ang II) activate PVN preautonomic neurons to increase in sympathetic nerve activity (SNA) and cause release of C-C chemokine ligand 2 (CCL2). The increased SNA impacts the bone marrow (BM) resulting in an increase in inflammatory cells (IC) and decrease in angiogenic progenitor cells (APCs). This imbalance is associated with vascular pathology and increase in blood pressure. Additionally, some of these inflammatory progenitors migrate to the PVN as a result of an increased neuronal release of CCL2 where they differentiate into BM-derived microglia/macrophages. Both resting microglia and BM-derived microglia/macrophages are activated to release an array of cytokines, chemokines, and reactive oxygen species (ROS) which will further increase preautonomic neuronal activity. This leads to a state of sustained sympatho-excitation which will result in a perpetuation of high blood pressure and ultimately established hypertension.