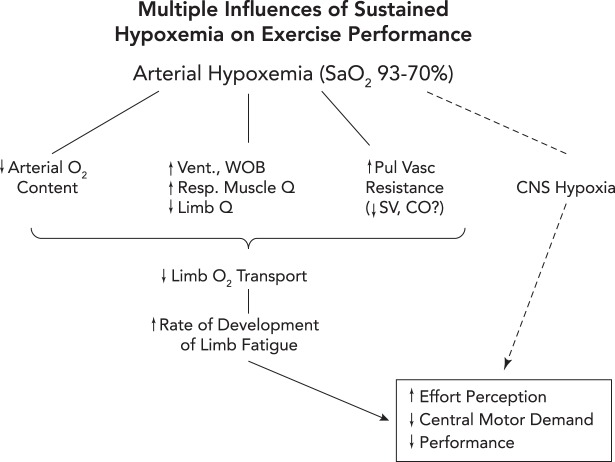
FIGURE 4.
Three potential routes to exacerbation of exercise-induced central and peripheral (locomotor muscle) fatigue and reduction in exercise performance in hypoxia
1: reduced O2 transport to locomotor muscles via a) exercise-induced arterial hypoxemia (a); reductions in locomotor muscle blood flow secondary to an augmented sympathetic vasoconstriction of locomotor muscle vasculature elicited by high levels of respiratory muscle work and fatigue (b) (29); and/or stroke volume and cardiac output may be compromised via high left ventricular afterload induced by positive intrathoracic pressure on expiration in the face of airway expiratory flow limitation (70) (see also FIGURE 2A) or by increased pulmonary vascular resistance causing interventricular septal deviation toward the left ventricle, thereby altering left ventricular geometry and delaying filling (c) (56, 79). 2: CNS hypoxia, especially at extreme levels of arterial O2 desaturation (<75% SaO2), will inhibit central motor command (likely linked to reduced neurotransmitter turnover) and limit performance even in the face of limited amounts of peripheral muscle fatigue (6). 3: peripheral and central fatigue are causally linked via feedback inhibition of central motor output through group III–IV muscle afferents. When these afferents were partially blocked during a cycling time trial, the cyclist “chose” a much higher power output (vs. placebo control) in the initial half of the trial, leading to excessive muscle metabolite accumulation, reduced power output, and excessive locomotor muscle fatigue at end-exercise (5).