Abstract
A natural disaster leading to accumulation of environmental contaminants may have substantial effects on the male reproductive system. Our aim was to compare and assess semen parameters in a normospermic population residing in the Southern Louisiana, USA area pre- and post-Hurricane Katrina. We retrospectively evaluated semen analyses data (n = 3452) of 1855 patients who attended the Tulane University Andrology/Fertility Clinic between 1999 and 2013. The study inclusion criteria were men whose semen analyses showed ≥ 1.5 ml volume; ≥15 million ml-1 sperm concentration; ≥39 million total sperm count; ≥40% motility; >30% morphology, with an abstinence interval of 2–7 days. After the inclusion criteria applied to the population, 367 normospermic patients were included in the study. Descriptive statistics and group-based analyses were performed to interpret the differences between the pre-Katrina (Group 1, 1999–2005) and the post-Katrina (Group 2, 2006–2013) populations. There were significant differences in motility, morphology, number of white blood cell, immature germ cell count, pH and presence of sperm agglutination, but surprisingly there were no significant differences in sperm count between the two populations. This long-term comparative analysis further documents that a major natural disaster with its accompanied environmental issues can influence certain semen parameters (e.g., motility and morphology) and, by extension, fertility potential of the population of such areas.
Keywords: environment, Hurricane Katrina, New Orleans area, normospermic infertile population, retrospective semen analysis
INTRODUCTION
Hurricane Katrina hit the Gulf Coast area of the United States on August 29, 2005 causing massive flooding in New Orleans and the Gulf region.1 Floodwater, mainly from nearby Lake Pontchartrain, carried substantial amounts of mud, heavy metals and other pollutants to the habitant land, air and water. Detrimental effects of toxic pollutants from similar disasters on human health are well documented.2,3,4 Studies have shown that lead (Pb) and arsenic (As) were discovered in relatively high concentrations in many of the soil/sediment samples collected from various locations 1–2 years post-Katrina.5 These heavy metals, especially Pb – and to some extent iron and copper – influence the male reproductive system with altered spermatogenesis, either directly affecting the testes or indirectly through the hypothalamic-pituitary-gonadal (HPG) axis.6,7,8 This alters sperm concentrations without affecting motility and semen volume.8 On the other hand, low dose, chronic Pb exposure results in a dose-dependent suppression of serum testosterone and spermatogenesis, and alters gonadotropin-releasing hormone system and HPG axis.9,10 In humans, low Pb environmental exposure affects semen quality and sperm chromatin condensation as reported in the northern Mexican population.11 Mental health disorders associated with anxiety, depression and stress often accompany natural disasters and affect reproduction and overall health.12,13 Similarly, high-rates of posttraumatic stress disorder with anxiety and depression were reported in the post-Katrina population.14 Fertile men who undergo two stressful life events often show abnormal sperm concentration, motility, and morphology.12 Psychological factors in male partners of infertile couples lead to poor semen quality, abnormal sperm morphology, and may lead to early miscarriage.15 Sperm morphological defects in four European cities were associated with lifestyle stress, longer daily working hours, and medical issues related to occupational exposure.16 There are very few previous studies that described the effects of large-scale disasters (e.g. civil war and earthquake) on male reproductive health as assessed through changes in semen parameters.17,18 The exact mechanism(s), whether mental or pathophysiological, and how any natural disaster is associated with reproductive health of certain population is not well understood. In order to assess such an association, we did retrospective analyses of semen parameters of men attending the Tulane University Hospital Andrology Clinic in New Orleans, Louisiana between 1999 and 2013, i.e. the period immediately before and after Hurricane Katrina disaster.
MATERIALS AND METHODS
Study population
A total of 1855 patients, with 3452 semen evaluations (S/E) were screened and out of that, 367 normospermic men (average age 34.8 years) were included in this study. Two different groups were stratified according to the date of semen analyses, as pre-Katrina (Group 1, between 1999 and 2005) and post-Katrina (Group 2, between 2006 and 2013) (Figure 1). Any patient diagnosed with azoospermia, oligozoospermia, low semen volume, poor motility and morphology, and inadequate ejaculatory abstinence period were excluded.
Figure 1.
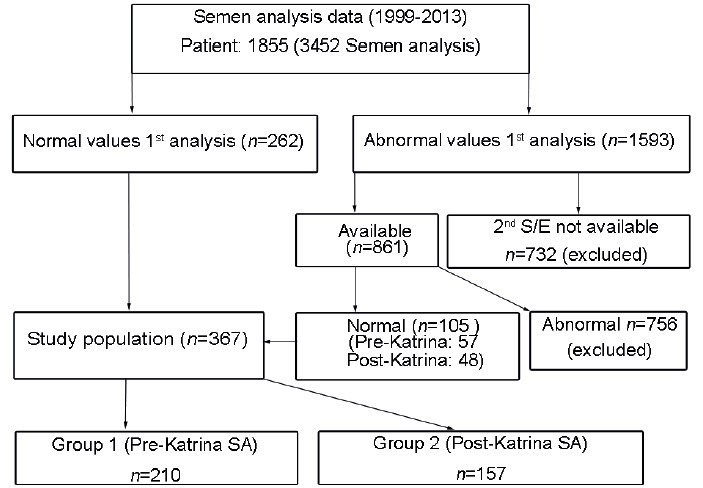
Patient stratification as pre- and post-Katrina groups.
Semen analyses
All semen analyses were performed using World Health Organization (WHO) 1992 guidelines19 and by a certified laboratory director (SCS) in a CLIA-certified Andrology Laboratory. All semen samples were collected in a private clinic room by masturbating in a sterile, plastic wide-mouth container, following 2–7 days of ejaculatory abstinence. A written consent was obtained from patients at the time of collection in order to use any data anonymously. Also, written and spoken instructions were provided to patients regarding proper semen collection including loss of sample or the improper duration of sexual abstinence. The collected sample was placed in an incubator (at 37°C) for 15–20 min to allow for liquefaction. Each sample was evaluated within one hour of collection using a calibrated phase-contrast microscope with × 20-phase objective and an eyepiece reticle with grid. A standardized disposable counting chamber (Leja Inc., Sweden) was used for all microscopic evaluations. The same observer read the sperm morphology after staining dried fixed smears by Diff-Quik methodology.19
Data evaluation
For this study, only normospermic values based on the most recent WHO criteria (i.e. semen volumes ≥ 1.5 ml, sperm count per milliliter ≥ 15 × 106, total sperm count ≥ 39 × 106, total motility ≥ 40% and abstinence interval between 2 and 7 days), were selected.20 For sperm morphology, nonstrict criteria were used based upon 1992 WHO manual.19 If any patient had an abnormal semen parameter as per these criteria, records were checked for a second semen analysis, and if that met the normal criteria, it was then included in the study.
Statistical evaluation
The two groups were compared using the Mann–Whitney and Chi-square tests because of the abnormal distribution of semen parameters. Regression analyses were performed for the motility index and normal head morphology. Post-Katrina group, age, race, and time of sexual abstinence were used as covariates. Spearman's correlation test was used to describe the correlation between the number of immature germ cells and white blood cells in a sample. Statistical software, SPSS version 21 (IBM Corp., Armonk, NY, USA) was used to calculate P values and P < 0.05 was established as significant.
RESULTS
A total of 367 patients (210 pre-Katrina and 157 post-Katrina) were categorized as normal as per the WHO criteria listed previously. Mean age was 34.8 years (35 years for Group 1 and 34.6 years for Group 2). Tables 1 and 2 document the detailed information of semen parameters; descriptive statistics and statistical differences of groups for the entire population. Some differences were observed between the two groups based on abstinence duration, pH, and agglutination. There were significant differences between groups according to motility and motility index. Average motility index values were 167 ± 51 and 141 ± 40 for pre- and post-Katrina groups, respectively (P = 0.001) (Table 1). In morphological parameters, a number of significant differences were observed between the two groups; specifically the normal head, mid-piece, and tail morphology of sperm (Table 2). Likewise, statistical differences were observed in number of white blood cells and immature germ cells between the two groups. Table 3 shows the summary of key S/E parameters. There was a strong correlation between numbers of white blood cells and immature germ cells count (Spearman's correlation coefficient: 0.935; P < 0.001). Interestingly, some decreasing trend was observed in pre-Katrina S/E values. Furthermore, the post-Katrina group's race (nonwhite) had an effect on motility index and normal head morphology. The motility index model identifies only 7.2% of variances (R2 = 0.072). On the other hand, the model explains 56% of the variances for head morphological change (R2 = 0.56). For normal mid-piece morphology, the post-Katrina group had a significant effect on variances as shown in Table 4. None of the covariates had an impact on differences of sperm motility and normal tail shape. Table 4 shows regression analysis results without the potential confounders for parameters (motility index and head/mid-piece morphology) that showed significant change between pre- and post-Katrina population.
Table 1.
Entire population group-based statistics
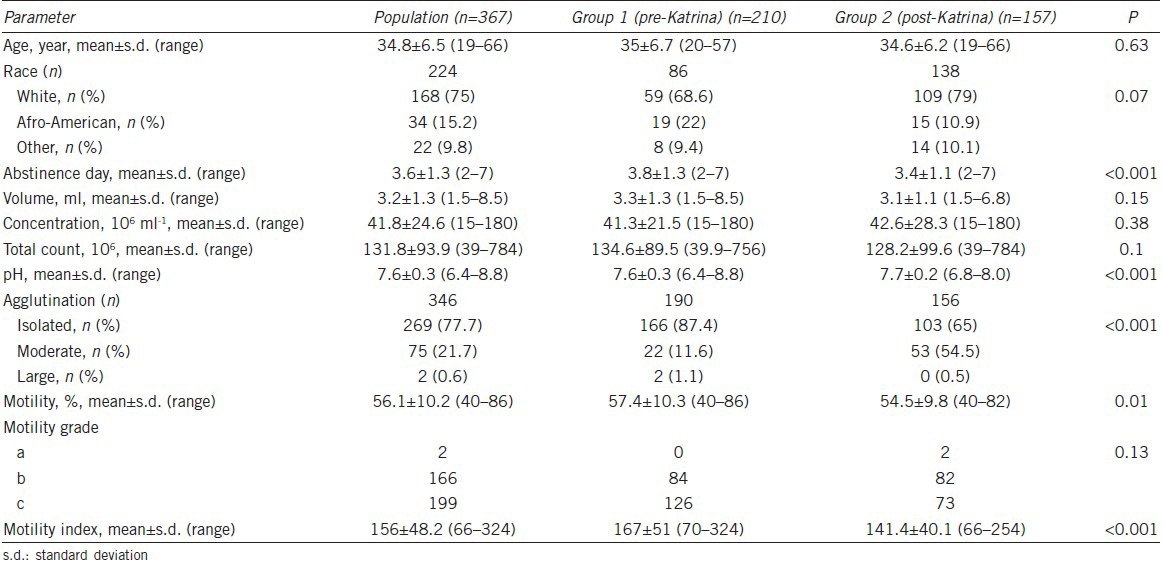
Table 2.
Morphological assessment of entire population and group-based statistics
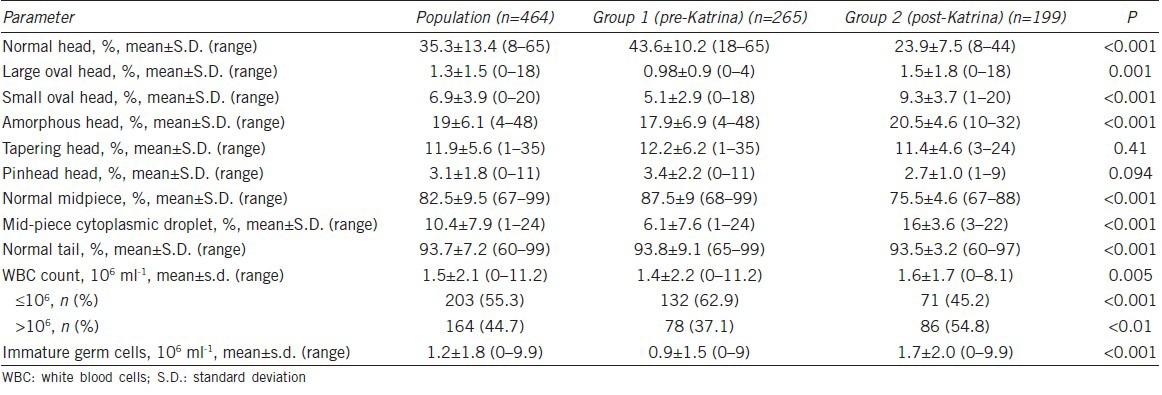
Table 3.
Summary of key S/E parameters
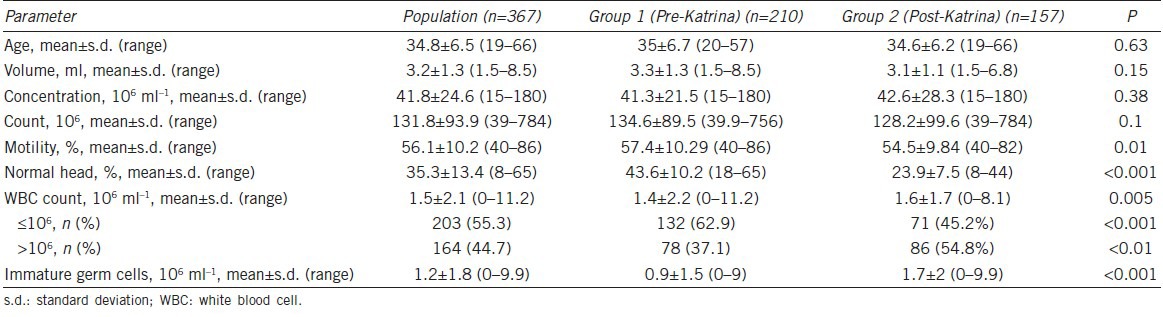
Table 4.
Regression analysis results without the potential confounders for parameters (motility index and head/piece morphology that showed significant change between pre- and post-Karina populations)
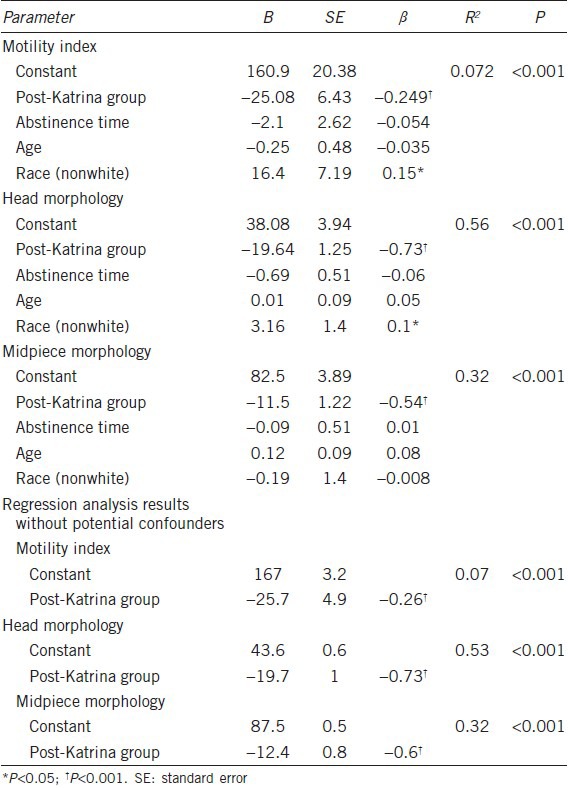
Figure 2a shows the changes in motility index in the pre- and post-Katrina populations and reveals a decreasing trend at a P < 0.001 significance. Figure 2b shows the changes in morphology of sperm head between two groups over time.
Figure 2.
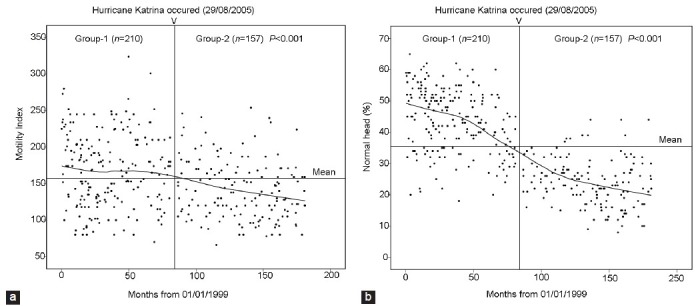
Changes in motility index between two groups over the time (a); and changes in normal head morphology between two groups over the time (b).
DISCUSSION
In 2005, Hurricane Katrina had a major impact on the residents of the US Gulf coast, resulting in major loss of life and property, as well as changes to the environment and population demography. It is recognized that toxic elements in the environment exert detrimental effects on semen parameters causing reduced reproductive potential.21 Adams et al. measured several organic and inorganic constituents in post-Katrina soil and noted that As, Pb and benzene concentrations were above acceptable levels.22 Mielke et al.23 showed that higher Pb levels in the soil reflect higher blood levels of habitants in the polluted area. Although the soil surface in many areas of greater New Orleans showed higher Pb levels post-Katrina,6,7,22 with a potential of affecting the reproductive system of both men and women, we did not observe major changes in semen volume, sperm concentration or total sperm count of the normospermic men attending our Andrology Clinic. It is interesting to note that the pre- and post-Katrina demography of these men has changed (Table 1), but it is not clear how many of the patients were the same or how long they inhabited such polluted areas. A longitudinal evaluation of their semen parameters and independent measures of Pb and As levels may show differences after a number of years.
The effect of disasters on semen parameters is a complex issue because many variables come into play that may affect semen parameters. In 1996, Fukuda et al. showed decreased sperm motility in men who lost their homes as a result of the Kobe earthquake in 1995.18 However, there was no difference in sperm concentrations before and after the earthquake. Also, their study consisted of only 27 patients without morphological assessment and evaluated only the short-term effects of the earthquake (i.e. the semen analyses were performed only 5 months before and after this event). In contrast, our retrospective study includes 367 normospermic patients comparing S/E from 210 pre-Katrina and 157 post-Katrina men. Different factors alongside hurricane Katrina may play a role in the alteration of motility index and sperm head morphology as observed by us.
Another retrospective study by Abu-Musa et al. evaluated the effect of the Lebanese civil war on semen parameters.17 These authors reported significantly lower sperm concentration during the wartime period, but no differences in semen volume and sperm motility were observed. However, these analyses were based on only one semen sample and they did not evaluate a second semen sample if the first semen sample was abnormal, which is contrary to WHO guidelines. Our study excluded participants if the second evaluation was also abnormal, thus ensuring that only normospremic men are included.
In our study, we did not find any significant differences in sperm concentration or total sperm count between the pre- and post-Katrina populations. Interestingly, some differences were observed in sperm motility, morphology, white blood cell counts and immature germ cells between pre- and post-Katrina groups. An important aspect from our data was the altered sperm morphology, which may be the most important factor in male fertility. Our study shows decreased normal sperm morphology in the semen of post-Katrina compared to pre-Katrina men (Figure 2b, Tables 2 and 3). Since morphological evaluations, using WHO nonstrict criteria of 30% normal forms (WHO 1999) were performed by the same expert (SCS), this change cannot be attributed to technical variability or other issues. Thus, it is important to determine whether these changes in morphology are a direct effect of pollutants and/or the stressful environment, and if these changes in morphology caused a lower fertility rate. Sperm morphology, when measured using strict criteria, may provide further defining information in both fertile and infertile men.24 This retrospective study was based upon WHO criteria and compared only normospermic men between the pre- and post-Katrina periods.9 The fertility aspect of the post-Katrina population has not been evaluated, but there appears to be an increased rate of infertile men being referred to our Andrology Clinic.
This study evaluated only those patients with normal semen volume, sperm concentration and 2–7 days of abstinence.19 This data selection method allows us to evaluate the trends without the skewing from azoo- or oligo-spermic patients.
Regression analysis showed that sexual abstinence duration has no effect on semen volume, sperm concentration and motility. However, there was a difference between groups in sperm head, mid-piece and tail morphology. Regression analysis of this data suggests that Hurricane Katrina adversely affected sperm head and mid-piece morphology in 56% and 32% of patients, respectively. We have also presented regression analysis results without potential confounders as a part of Table 4.
Another interesting observation was the numerical difference in the amount of immature germ cells in the two groups (Table 2). Usually, white blood cells and immature germ cells are collectively known as “round cells” in semen. Excessive numbers of white blood cells in semen may imply genitourinary inflammation (GUI) (e.g., prostatitis). Such changes may not play a direct role in causing reproductive decline, but may play a role in depressed immune system causing more GUI. However, increased number of immature germ cell in post-Katrina population may suggest poor recovery of spermatogenesis after testicular damage.19
In summary, the results from 367 age-matched normospermic men suggest a significant decline in sperm morphology and motility in the post-Katrina population. It will be interesting to further evaluate the fertility changes of this population. We should note that this retrospective study did not compare clinical information such as a testicular size, hormonal profiles, etc. These results were observed in a population over a longer duration than previously reported and employed technical standardization and minimal variation of measurement. Further studies are needed to explain the effect of disasters on the male reproductive system and similarly on female reproductive changes.
AUTHOR CONTRIBUTIONS
CB extracted data, participated in the design of the study, performed statistical analysis and drafted the manuscript. WJH participated in the design of the study, helped to draft of the manuscript. SCS performed semen analysis, planned the concept, participated in the design of the study, helped in statistical analysis and in finalizing the manuscript. All authors read and approved the final manuscript.
COMPETING INTERESTS
All authors declare no competing interests.
REFERENCES
- 1.Knabb RD, Rhome JR, Brown DP. Tropical Cyclone Report: Hurricane Katrina. National Oceanic and Atmospheric Administration, National Weather Service, National Hurricane Center; August - 23–30. 2005 [Google Scholar]
- 2.Englande AJ., Jr Katrina and the Thai Tsunami – Water quality and public health aspects mitigation and research needs. Int J Environ Res Public Health. 2008;5:384–93. doi: 10.3390/ijerph5050384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kessler RC, Galea S, Jones RT, Parker HA Hurricane Katrina Community Advisory Group. Mental illness and suicidality after Hurricane Katrina. Bull World Health Organ. 2006;84:930–9. doi: 10.2471/blt.06.033019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rao CY, Riggs MA, Chew GL, Muilenberg ML, Thorne PS, et al. Characterization of airborne molds, endotoxins, and glucans in homes in New Orleans after Hurricanes Katrina and Rita. Appl Environ Microbiol. 2007;73:1630–4. doi: 10.1128/AEM.01973-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shi H, Witt EC 3 r rd, Shu S, Su T, Wang J, et al. Toxic trace element assessment for soils/sediments deposited during Hurricanes Katrina and Rita from southern Louisiana, USA: a sequential extraction analysis. Environ Toxicol Chem. 2010;29:1419–28. doi: 10.1002/etc.218. [DOI] [PubMed] [Google Scholar]
- 6.Abel MT, Suedel B, Presley SM, Rainwater TR, Austin GP, et al. Spatial distribution of lead concentrations in urban surface soils of New Orleans, Louisiana USA. Environ Geochem Health. 2010;32:379–89. doi: 10.1007/s10653-009-9282-1. [DOI] [PubMed] [Google Scholar]
- 7.Chou J, Elbers D, Clement G, Bursavich B, Tian T, et al. In situ monitoring (field screening) and assessment of lead and arsenic contaminants in the greater New Orleans area using a portable X-ray fluorescence analyser. J Environ Monit. 2010;12:1722–9. doi: 10.1039/c0em00012d. [DOI] [PubMed] [Google Scholar]
- 8.Xu W, Bao H, Liu F, Liu L, Zhu YG, et al. Environmental exposure to arsenic may reduce human semen quality: associations derived from a Chinese cross-sectional study. Environ Health. 2012;11:46. doi: 10.1186/1476-069X-11-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sokol RZ. The effect of duration of exposure on the expression of lead toxicity on the male reproductive axis. J Androl. 1990;11:521–6. [PubMed] [Google Scholar]
- 10.Sokol RZ, Wang S, Wan YJ, Stanczyk FZ, Gentzschein E, et al. Long-term, low-dose lead exposure alters the gonadotropin-releasing hormone system in the male rat. Environ Health Perspect. 2002;110:871–4. doi: 10.1289/ehp.02110871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hernández-Ochoa I, García-Vargas G, López-Carrillo L, Rubio-Andrade M, Morán-Martínez J, et al. Low lead environmental exposure alters semen quality and sperm chromatin condensation in northern Mexico. Reprod Toxicol. 2005;20:221–8. doi: 10.1016/j.reprotox.2005.01.007. [DOI] [PubMed] [Google Scholar]
- 12.Gollenberg AL, Liu F, Brazil C, Drobnis EZ, Guzick D, et al. Semen quality in fertile men in relation to psychosocial stress. Fertil Steril. 2010;93:1104–11. doi: 10.1016/j.fertnstert.2008.12.018. [DOI] [PubMed] [Google Scholar]
- 13.Canino G, Bravo M, Rubiostipec M, Woodbury M. The impact of disaster on mental-health-prospective and retrospective analyses. Int J Ment Health. 1990;19:51–69. [Google Scholar]
- 14.Galea S, Brewin CR, Gruber M, Jones RT, King DW, et al. Exposure to hurricane-related stressors and mental illness after Hurricane Katrina. Arch Gen Psychiatry. 2007;64:1427–34. doi: 10.1001/archpsyc.64.12.1427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zorn B, Auger J, Velikonja V, Kolbezen M, Meden-Vrtovec H. Psychological factors in male partners of infertile couples: relationship with semen quality and early miscarriage. Int J Androl. 2008;31:557–64. doi: 10.1111/j.1365-2605.2007.00806.x. [DOI] [PubMed] [Google Scholar]
- 16.Auger J, Eustache F, Andersen AG, Irvine DS, Jørgensen N, et al. Sperm morphological defects related to environment, lifestyle and medical history of 1001 male partners of pregnant women from four European cities. Hum Reprod. 2001;16:2710–7. doi: 10.1093/humrep/16.12.2710. [DOI] [PubMed] [Google Scholar]
- 17.Abu-Musa AA, Nassar AH, Hannoun AB, Usta IM. Effect of the Lebanese civil war on sperm parameters. Fertil Steril. 2007;88:1579–82. doi: 10.1016/j.fertnstert.2007.01.067. [DOI] [PubMed] [Google Scholar]
- 18.Fukuda M, Fukuda K, Shimizu T, Yomura W, Shimizu S. Kobe earthquake and reduced sperm motility. Hum Reprod. 1996;11:1244–6. doi: 10.1093/oxfordjournals.humrep.a019365. [DOI] [PubMed] [Google Scholar]
- 19.3rd ed. Geneva: World Health Organization; 1992. World Health Organization. WHO Laboratory Manual for the Examination and Processing of Human Semen. [Google Scholar]
- 20.5th ed. Geneva: World Health Organization; 2010. World Health Organization. WHO Laboratory Manual for the Examination and Processing of Human Semen. [Google Scholar]
- 21.Jurewicz J, Hanke W, Radwan M, Bonde JP. Environmental factors and semen quality. Int J Occup Med Environ Health. 2009;22:305–29. doi: 10.2478/v10001-009-0036-1. [DOI] [PubMed] [Google Scholar]
- 22.Adams C, Witt EC, Wang J, Shaver DK, Summers D, et al. Chemical quality of depositional sediments and associated soils in New Orleans and the Louisiana Peninsula following Hurricane Katrina. Environ Sci Technol. 2007;41:3437–43. doi: 10.1021/es0620991. [DOI] [PubMed] [Google Scholar]
- 23.Mielke HW, Gonzales CR, Mielke PW., Jr The continuing impact of lead dust on children's blood lead: comparison of public and private properties in New Orleans. Environ Res. 2011;111:1164–72. doi: 10.1016/j.envres.2011.06.010. [DOI] [PubMed] [Google Scholar]
- 24.Guzick DS, Overstreet JW, Factor-Litvak P, Brazil CK, Nakajima ST, et al. Sperm morphology, motility, and concentration in fertile and infertile men. N Engl J Med. 2001;345:1388–93. doi: 10.1056/NEJMoa003005. [DOI] [PubMed] [Google Scholar]


