Abstract
Background
The medial patellofemoral ligament is the primary soft-tissue restraint to lateral patella translation. Medial patellofemoral ligament reconstruction has become a viable surgical option to provide patellar stability in patients with recurrent instability. The primary goal of this study was to determine the effect of medial patellofemoral ligament reconstruction on the lateral force-displacement behavior of the patella using finite element analyses.
Methods
A finite element model of the knee was created using cadaveric image data. Experimental testing was performed to validate the computational model. After validation, the model was modified to study the effect of various medial patellofemoral ligament reconstruction insertion sites, allowing comparison of patellofemoral contact force and pressure.
Results
For the intact anatomic model, the lateral restraining force was 80.0 N with a corresponding patellar contact area of 54.97 mm2. For the anatomic reconstructed medial patellofemoral ligament model, the lateral restraining force increased to 148.9 N with a contact area of 71.78 mm2. This compared favorably to the corresponding experimental study. The force required to laterally displace the patella increased when the femoral insertion site was moved anteriorly or distally. The lateral restraining force decreased when the femoral insertion site moved proximally and the patellar insertion site moved either proximal or distal by 5 mm.
Conclusion
The line of action was altered with insertion site position, which in turn changed the amount of force it took to displace the patella laterally. Considering the model constraints, an anterior femoral attachment may over constrain the patella and increase cartilage wear due to increase contact area and restraining force.
Clinical Relevance
A malpositioned femoral tunnel in MPFL reconstruction could increase restraining forces and PF contact pressure, thus it is suggested to use intra-operative fluoroscopy to confirm correct tunnel placement.
Introduction
Patellar stability is maintained by the bony architecture, soft tissue restraints, and dynamic action of the quadriceps throughout knee motion. The medial patellofemoral ligament (MPFL) is the primary soft tissue restraint to lateral translation of the patella1-3, acting as a check-rein to lateral translation during the first 30° of knee flexion prior to the patella engaging the trochlear groove4,5. Following acute lateral patellar dislocation, the MPFL is the most consistently injured ligamentous structure6-8. Nonoperative management of acute lateral patellar dislocation frequently results in recurrent instability, potentially requiring future surgical intervention9,10. Proximal soft tissue procedures, such as MPFL reconstruction or repair, are indicated in patients with normal bony alignment and a deficient MPFL4,7,11. Due to poor outcomes following MPFL repair12-14, MPFL reconstruction, which aims to restore the form and function of the native MPFL, has become the procedure of choice for this patient population.
Although MPFL reconstruction is a popular technique, relatively few studies have investigated the behavior of the patellofemoral joint after MPFL reconstruction. While MPFL reconstruction aims to restore the native properties of the ligament, experimental studies have shown that variations in insertion sites may over constrain the patella and lead to premature osteoarthritis due to increased medial patellofemoral contact pressures or result in recurrent instability due to graft failure5,15.
Therefore, the primary goal of this study was to determine the effect of MPFL reconstruction on the lateral force-displacement behavior of the patella using finite element analyses. Additionally, our objective was to study the affect MPFL reconstruction insertion site has on patellofemoral contact force, area and pressure.
Methods
A single finite element (FE) model of the knee was created to gain a better understanding of MPFL reconstruction. The model was validated with corresponding experimental data. After model validation, the FE model was modified to study what effect MPFL reconstruction insertion site has on patellofemoral biomechanics.
Finite Element Model
A magnetic resonance (MR) image of a cadaveric knee joint was obtained and used to define the bone and soft tissue anatomy. The bones (tibia, femur, and patella) and soft tissues (cartilage, patellar tendon (FT), and quadriceps tendon (QT)) were manually segmented using BRAINS2 software16,17. Surfaces were generated from the traced regions of interest using Gaussian image based smoothing, similar to the techniques described by DeVries et al18.
A finite element model was created using IA-FEMesh19 (Figure 1). IA-FEMesh allows meshes to be created based on anatomical surfaces generated from medical image segmentation. The bones were modeled using three-dimensional rigid elements since bone is significantly stiffer than the soft tissues, which were the structures of interest, not the bone. The model did not include the fibula, similar to previous computational models of patellofemoral biomechanics20-23. The cartilage, FT, and QT were modeled using 8-noded hexahedral elements. The MPFL and the medial patellotibial ligament (MPTL) were also modeled using hexahedral elements. Since the ligaments, specifically the attachment sites, were difficult to define on MR images due to their thin anatomy, they were modeled based on the insertion sites and dimensions (i.e. width, thickness) previously reported in anatomic studies12,24-26. The meniscus was not included since the study focused on the patellofemoral interaction at a static flexed knee position.
Figure 1. (A) The finite element mesh of the knee, including the quadrilateral tendon, patellar tendon, cartilage, medial patellofemoral ligament and the medial patellotibio ligament. (B) the von Mises stress after 10 mm lateral patellar displacement for the intact MPFL model.
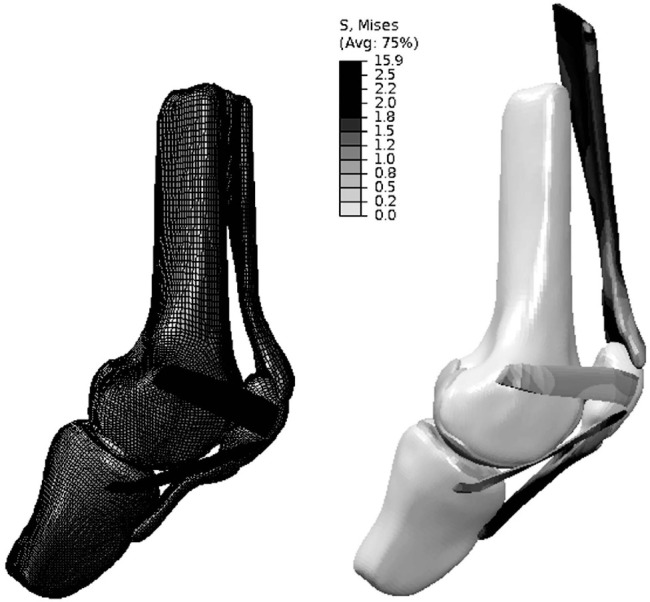
The viscoelastic nature of the cartilage was simplified to linear elastic material properties (E=12 MPa, v=0.45)22,23,27. The tendon and ligaments were modeled as hyperelastic with the material properties adapted from stress-strain and force-displacement curves reported in literature28-30. The reconstructed MPFL assumed material properties characteristic of the tibialis tendon31. The anatomic reconstruction insertion site and dimensions were considered to be the same as the intact model, which was based on anatomical data reported in literature12,24-26.
To ensure model accuracy, a convergence study was conducted on the MPFL, since this was the primary tissue of interest. Meshes were created for the isolated MPFL, with varying mesh densities ranging from two elements to 4160 elements. A 100 N force was applied along the long axis of the MPFL, and stresses were monitored at three locations. Based on convergence, a mesh density of 520 elements was chosen to model the MPFL. A similar mesh element size was used throughout the entire knee model.
For both the intact and reconstructed models, the knee was positioned at 30° of flexion, with the femur fixed in all directions and the tibia free to translate and rotate about the z-axis, allowing anterior-posterior translation and varus-valgus rotation. The patella was free to rotate and displace in all directions. The quadriceps was physiologically loaded to 178 N, along the three main muscle groups32-34. With the quadriceps loaded, the tibia and femur were fixed in all directions and the patella was displaced laterally 10 mm. The resultant patellar restraining force, contact pressure, and contact area were compared for the intact and reconstructed MPFL. Analyses were completed using Abaqus/Standard (Version 6.12-1; Dassault Systèmes Simulia, Providence, RI).
Model Validation/Experimental Study
To validate the computational models, corresponding experimental testing was conducted35. Four fresh-frozen knees were obtained from two cadavers (95 year old male; 57 year old female). Prior to testing, magnetic resonance images were obtained to ensure continuity of the MPFL in all specimens. All soft tissues were dissected with the exception of the distal quadriceps extensor mechanism, MPFL, and capsular tissue surrounding the knee. The distal quadriceps was separated into three muscle groups (vastus medialis (VM), vastus lateralis (VL), and rectus femoris and vastus intermedius (RF+VI)). Cloth strips were attached to each muscle group to allow loading through the extensor mechanism. The femur and tibia were fixed in a polymer resin, allowing for attachment to the custom testing fixture.
The knee specimen was fixed at 30° of flexion using a custom fixture, with the femur and tibia firmly held in all directions. Next, the components of the quadriceps were loaded with a total of 178 N, accounting for physiological loading directions and cross-sectional areas32-34. The patella was connected to a loading rod using a ball joint, allowing for patella rotation about the anterior-posterior and proximal-distal axes. Figure 3 shows the testing setup. Using a biaxial servo-hydraulic materials testing machine, the patella was cyclically displaced 10 mm laterally from its neutral position at 100 mm/minute33,36. The force to displace the patella 10 mm laterally (restraining force) was recorded, with the fourth cycle used for analyses.
Figure 3. Experimental setup with the knee mounted in the Bionix II material testing machine with the quadriceps loaded using a custom pulley system through the cloth loops.

After intact MPFL testing, the MPFL was sectioned and an MPFL reconstruction performed using a split anterior tibialis allograft. For additional information on the MPFL reconstruction procedure, refer to the study by Duchman et al35.
The FE model was validated using the results from the experimental study by comparing the patellar restraining force for both the intact MPFL and MPFL reconstruction at anatomical insertion. The stiffness was also compared. The stiffness of the MPFL in response to lateral patella displacement for both the intact and reconstructed MPFL was calculated for the first 1.5 mm of displacement (S1) and from 1.5 mm to 10 mm of displacement (S2). Stiffness was defined as the slope of the linear regression that was fit to each region of the load-displacement curve.
Reconstructed MPFL - Insertion Sites
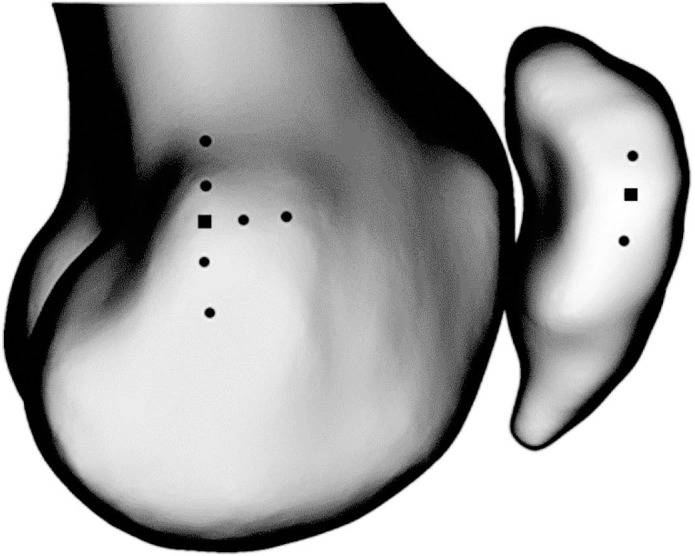
The validated model was used to study multiple MPFL reconstruction insertion sites. Specifically, the insertion sites were repositioned in increments of 5 mm from the anatomic position on both the femur and patella37. For the validated model, the femoral and patellar insertions assumed the anatomic position. Thereafter, the femoral insertion was modeled at 5 mm and 10 mm anterior, proximal, and distal to the anatomic position (Figure 2), with the patellar insertion remaining at anatomic position. Additionally, the patellar insertion site was positioned 5 mm proximal and distal to the anatomic site, with the femoral insertion site remaining in anatomic position, thus creating nine unique insertion scenarios (Figure 2). Note, the initial tension (0 N) in the graft remained the same for the different insertion sites.
Figure 2. The attachement sites for the reconstructed medial patel-lofemoral ligament. The black squares represent the anatomical attachement site. The black dots show locations 5mm and 10mm anterior, proximal, and distal to the anatomical attachement sites.
Results
For the intact FE model, the lateral restraining force was 80.0 N with a corresponding patellar contact area of 54.97 mm2. For the reconstructed MPFL FE model, the lateral restraining force increased to 148.9 N with a contact area of 71.78 mm2. The biomechanical data for the finite element model is summarized in Table 1. The model predicted restraining forces were greater than the forces measured during the experimental study, where the average lateral restraining force was 69.0 (5.9) N for the intact MPFL, increasing to 110.2 (17.5) N for the reconstructed MPFL. The ratios between intact and reconstructed MPFL restraining forces were similar, however.
Table 1.
The biomechanical data for lateral patella displacement of 10 mm determined by the finite element model
| Force at the Patella (N) | Contact Force (N) | Maximum Contact Pressure (MPa) | Total Contact Pressure (MPa) | Contact Area (mm2) | |
|---|---|---|---|---|---|
| Anatomical Intact | 80.0 | 178.4 | 7.76 | 82.72 | 54.97 |
| Anatomical Reconstructed | 148.9 | 226.9 | 5.00 | 89.21 | 71.78 |
| Femur Anterior 5mm | 163.1 | 232.4 | 4.76 | 88.71 | 86.68 |
| Femur Anterior 10mm | 177.0 | 236.6 | 4.58 | 87.84 | 95.22 |
| Femur Distal 5mm | 159.4 | 230.0 | 4.96 | 89.09 | 83.84 |
| Femur Distal 10mm | 154.5 | 222.1 | 4.38 | 83.51 | 89.06 |
| Femur Proximal 5mm | 125.1 | 215.4 | 6.40 | 88.55 | 67.24 |
| Femur Proximal 10mm | 114.1 | 211.7 | 6.39 | 89.61 | 60.08 |
| Patella Distal 5mm | 135.6 | 220.5 | 6.81 | 92.26 | 68.09 |
| Patella Proximal 5mm | 132.6 | 217.3 | 4.76 | 86.08 | 69.80 |
In the intact FE model, S1 was 17.39 N/mm and S2 decreased to 6.15 N/mm. Comparatively, the experimental average S1 was 24.5 (5.0) N/mm; S2 decreased to 5.0 (1.6) N/mm. The stiffness for the reconstructed MPFL model was higher than the intact model. S1 was 18.97 N/ mm and S2 decreased to 14.12 N/mm. Experimentally, the average S1 for the MPFL reconstruction was 23.1 (4.2) N/mm; S2 average stiffness was 11.2 (1.8) N/mm.
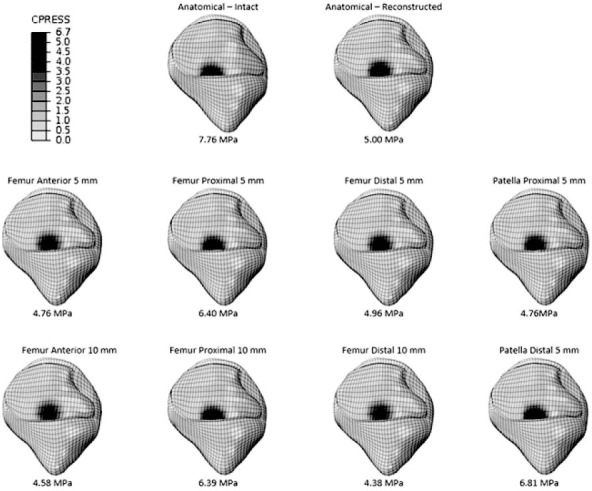
Comparing the different reconstruction insertion site models to the anatomic MPFL insertion model, the lateral restraining force increased when the femoral insertion site was moved anteriorly or distally. The force decreased when the femoral insertion site moved proximally. Additionally, the lateral restraining force decreased when the patellar insertion site moved either proximally or distally by 5 mm relative to the anatomic insertion. Table 1 summarizes the biomechanical results for patellar lateral displacement of 10 mm, comparing the various insertion site models. Figure 4 shows the contact pattern and the corresponding contact pressure for each model. Similar to the lateral restraining force, the contact force increased for femoral insertion sites that were anterior, but decreased for femoral insertion sites proximal to the anatomical insertion. Additionally, the contact force decreased with the patella insertion site moving either proximal or distal by 5 mm.
Figure 4. The contact pressure (MPa) of the patella after 10 mm of lateral displacement The peak contact pressure is provided below for each MPFL insertion model.
Discussion
Previous authors5,6,38 have highlighted the importance of anatomic graft position during MPFL reconstruction, but there have been relatively few studies that describe patellofemoral contact force and area after reconstruction. This finite element study provides insight into the changes in patellofemoral biomechanics due to medial patellofemoral ligament reconstruction, including the effect of reconstruction insertion site.
The finite element model was compared to the experimental study by Duchman et al.35 The model predicted similar, although slightly larger, forces to displace the patella 10 mm laterally for both the intact and reconstructed MPFL. The difference between experimental forces and the model predicted forces could be due to the large variability in patellofemoral anatomy. Also, the models had similar stiffness predictions with a greater initial stiffness (0–1.5 mm range) than S2 (1.5–10 mm range). This was true both experimentally and theoretically. Since the experimental and finite element model results were comparable for both force and stiffness and followed a general trend, the anatomical model was considered validated.
For additional validation, the model was compared to experimental studies focusing on patellofemoral contact area. Although there is no direct comparison due to different loading conditions and varying techniques to define contact area, the contact pattern for the current study was similar to previous studies. The femoral contact pattern at 30° was comparable to the study by Yamada et al.39; like the current study, the contact was primarily isolated to the proximal portion of the femoral trochlear cartilage. Additionally, the patellar contact pattern was similar to that reported in the experimental study by Lee et al.40 The contact pattern was centered on the patella itself. For the current study, the contact occurred on the distal edge of the cartilaginous portion of the patella, but central overall on the patella (Figure 5).
Figure 5. The contact pressure and area for the patellofemoral contact at 30° flexion with the quadriceps loaded to 178N.

Using this validated anatomical model, the effects of MPFL reconstruction insertion sites were studied, comparing the alternate insertion sites to the anatomically reconstructed MPFL. For this model, the initial graft tension did not vary with insertion site; the graft was not pre-tensioned and had the same material properties. It was determined that the insertion site does have an effect on the biomechanics of the patellofemoral joint. Anterior placement on the femur resulted in the greatest increase in patellar restraining force (a difference of 28.1 N at 10 mm anteriorly) compared to the anatomical MPFL reconstruction. This also resulted in a 32.7% increase in contact area with little decrease in contact pressure, both peak pressure (8.4%) and total pressure (1.5%). The larger contact area with minimal change in pressure may result in increased cartilage wear, suggesting that clinicians should avoid anterior graft positioning during reconstruction.
On the other hand, when the femoral insertion site was shifted proximally, the patellar force decreased by 34.8 N. The proximal insertion also had a lower patella contact force and contact area, which resulted in forces and contact area that are between the anatomically intact and reconstructed MPFL. The decrease in contact area and lateral restraining force may be due to the line of action of the reconstructed MPFL ligament based on the insertion site. The different ligament line of action may make it easier to laterally displace within the trochlear groove. Since the goal of MPFL reconstruction is to provide additional stability, proximal insertion may provide inadequate stability
There are limitations to this study. First, the model is based on a single specimen; with high variability in trochlear groove depth and patella anatomy, it may be beneficial to extend this study to several models to account for anatomical differences. Also, for this model the MPFL and medial patellotibial ligament were modeled based on anatomic data reported in literature and were not specimen specific. Although defining these ligaments from medical images would be ideal, it is a challenge due to the thin anatomy and complex nature of the attachment site. With advances in medical imaging, future models may be able to define all soft tissues on a specimen-/subject- specific basis, as opposed to average anatomical data. Additionally, this model did not incorporate the meniscus since static loading options were considered. To study various loading conditions and angles of flexion, the meniscus should be added to the model. Also, the model boundary conditions do not capture in vivo scenarios; however, do mimic in vitro loading conditions. The model boundary constraints should be considered when applying these predicted trends to clinical situations. This study was restricted to one angle of flexion and graft tension. Future work should look at different flexion angles and different graft tensions. Additionally, the model will be used to look at different combinations of MPFL reconstruction insertion sites, where both the patellar and femoral insertion are not anatomic.
Although the model has limitations and constraints, it affords insight into overall patellar biomechanics, comparing intact MPFL to MPFL reconstruction. Additionally, the study addresses the effects of MPFL reconstruction insertion sites. Corresponding with experimental studies, MPFL reconstruction increases the patella lateral restraining force. Considering the constraint condition and model restrictions, the study predicts that placement anterior to the femoral anatomical insertion could increase the contact force and area, whereas an insertion proximal to the anatomical position may reduce the contact force and area.
Acknowledgments
The authors would like to thank Dr. Mark McCarthy and Justin Kuiper for their assistance with the experimental setup and testing.
References
- 1.Melegari TM, Parks BG, Matthews LS. Patellofemoral contact area and pressure after medial patellofemoral ligament reconstruction. AmJSports Med. 2008;36:747–52. doi: 10.1177/0363546508314410. [DOI] [PubMed] [Google Scholar]
- 2.Desio SM, Burks RT, Bachus KN. Soft tissue restraints to lateral patellar translation in the human knee. AmJSports Med. 1998;26:59–65. doi: 10.1177/03635465980260012701. [DOI] [PubMed] [Google Scholar]
- 3.Schöttle PB, Fucentese SF, Romero J. Clinical and radiological outcome of medial patellofemoral ligament reconstruction with a semitendinosus autograft for patella instability. Knee Surgery Sports Traumatology, Arthroscopy. 2005;13:516–21. doi: 10.1007/s00167-005-0659-0. [DOI] [PubMed] [Google Scholar]
- 4.Bicos J, Fulkerson JP, Amis A. Current Concepts Review: The Medial Patellofemoral Ligament. AmJSports Med. 2007;35:484–92. doi: 10.1177/0363546507299237. [DOI] [PubMed] [Google Scholar]
- 5.Bollier M, Fulkerson J, Cosgarea A, Tanaka M. Technical Failure of Medial Patellofemoral Ligament Reconstruction. Arthroscopy: The Journal of Arthroscopic & Related Surgery. 2011;27:1153–9. doi: 10.1016/j.arthro.2011.02.014. [DOI] [PubMed] [Google Scholar]
- 6.Amis AA, Firer P, Mountney J, Senavongse W, Thomas NP. Anatomy and biomechanics of the medial patellofemoral ligament. The Knee. 2003;10:215–20. doi: 10.1016/s0968-0160(03)00006-1. [DOI] [PubMed] [Google Scholar]
- 7.Farr J, Schepsis AA. Reconstruction of the medial patellofemoral ligament for recurrent patellar instability. JKnee Surg. 2006;19:307–16. doi: 10.1055/s-0030-1248123. [DOI] [PubMed] [Google Scholar]
- 8.Servien E, Fritsch B, Lustig S, et al. In vivo positioning analysis of medial patellofemoral ligament reconstruction. AmJSports Med. 2011;39:134–9. doi: 10.1177/0363546510381362. [DOI] [PubMed] [Google Scholar]
- 9.Fithian DC, Paxton EW, Stone ML, et al. Epidemiology and natural history of acute patellar dislocation. AmJSports Med. 2004;32:1114–21. doi: 10.1177/0363546503260788. [DOI] [PubMed] [Google Scholar]
- 10.Hawkins RJ, Bell RH, Anisette G. Acute patellar dislocations. AmJSports Med. 1986;14:117–20. doi: 10.1177/036354658601400204. [DOI] [PubMed] [Google Scholar]
- 11.Colvin AC, West RV. Current Concepts Review: Patellar Instability. JBone Joint SurgAm. 2008;90:2751–62. doi: 10.2106/JBJS.H.00211. [DOI] [PubMed] [Google Scholar]
- 12.LaPrade RF, Engebretsen AH, Ly TV, Johansen S, Wentorf FA, Engebretsen L. The anatomy of the medial part of the knee. The Journal of Bone and Joint Surgery (American) 2007;89:2000. doi: 10.2106/JBJS.F.01176. [DOI] [PubMed] [Google Scholar]
- 13.Mountney J, Senavongse W, Amis AA, Thomas NP. Tensile strength of the medial patellofemoral ligament before and after repair or reconstruction. Journal of Bone and Joint Surgery-British Volume. 2005;87:36. [PubMed] [Google Scholar]
- 14.Schottle PB, Schmeling A, Rosenstiel N, Weiler A. Radiographic landmarks for femoral tunnel placement in medial patellofemoral ligament reconstruction. AmJSports Med. 2007;35:801. doi: 10.1177/0363546506296415. [DOI] [PubMed] [Google Scholar]
- 15.Elias JJ, Cosgarea AJ. Technical errors during medial patellofemoral ligament reconstruction could overload medial patellofemoral cartilage. AmJSports Med. 2006;34:1478–85. doi: 10.1177/0363546506287486. [DOI] [PubMed] [Google Scholar]
- 16.Andreasen NC, Cohen G, Harris G, et al. Image processing for the study of brain structure and function: problems and programs. The Journal of Neuropsychiatry and Clinical Neurosciences. 1992;4:125–33. doi: 10.1176/jnp.4.2.125. [DOI] [PubMed] [Google Scholar]
- 17.Magnotta VA, Harris G, Andreasen NC, O'Learya DS, Yuhb WTC, Heckela D. Structural MR image processing using the BRAINS2 toolbox. Computerized Medical Imaging and Graphics. 2002;26:251–64. doi: 10.1016/s0895-6111(02)00011-3. [DOI] [PubMed] [Google Scholar]
- 18.DeVries NA, Gassman EE, Kallemeyn NA, Shivanna KH, Magnotta VA, Grosland NM. Validation of phalanx bone three-dimensional surface segmentation from computed tomography images using laser scanning. Skeletal Radiology. 2008;37:35. doi: 10.1007/s00256-007-0386-3. [DOI] [PubMed] [Google Scholar]
- 19.Grosland NM, Shivanna KH, Magnotta VA, et al. IA-FEMesh: An open-source, interactive, mul-tiblock approach to anatomic finite element model development. Computer Methods and Programs in Biomedicine. 2009;94:96. doi: 10.1016/j.cmpb.2008.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Besier TF, Gold GE, Delp SL, Fredericson M, Beaupré GS. The influence of femoral internal and external rotation on cartilage stresses within the patellofemoral joint. Journal of Orthopaedic Research. 2008;26:1627–35. doi: 10.1002/jor.20663. [DOI] [PubMed] [Google Scholar]
- 21.Besier TF, Draper C, Pal S, et al. Imaging and musculoskeletal modeling to investigate the mechanical etiology of patellofemoral pain. In: Sanchis-Alfonso V, editor. Anterior Knee Pain and Patellar Instability. Springer-Verlag; 2011. pp. 269–84. [Google Scholar]
- 22.Fitzpatrick CK, Baldwin MA, Rullkoetter PJ. Computationally Efficient Finite Element Evaluation of Natural Patellofemoral Mechanics. Journal of Biomechanical Engineering. 2010;132:121013–1. doi: 10.1115/1.4002854. - -8. [DOI] [PubMed] [Google Scholar]
- 23.Shirazi-Adl A, Mesfar W. Effect of tibial tubercle elevation on biomechanics of the entire knee joint under muscle loads. Clinical Biomechanics. 2007;22:344–51. doi: 10.1016/j.clinbiomech.2006.11.003. [DOI] [PubMed] [Google Scholar]
- 24.Baldwin JL. The anatomy of the medial patellofemoral ligament. AmJSports Med. 2009;37:2355–61. doi: 10.1177/0363546509339909. [DOI] [PubMed] [Google Scholar]
- 25.Panagiotopoulos E, Strzelczyk P, Herrmann M, Scuderi G. Cadaveric study on static medial patellar stabilizers: the dynamizing role of the vastus medialis obliquus on medial patellofemoral ligament. Knee Surgery Sports Traumatology, Arthroscopy. 2006;14:7. doi: 10.1007/s00167-005-0631-z. [DOI] [PubMed] [Google Scholar]
- 26.Philippot R, Chouteau J, Wegrzyn J, Testa R, Fessy MH, Moyen B. Medial patellofemoral ligament anatomy: implications for its surgical reconstruction. Knee Surgery Sports Traumatology, Arthroscopy. 2009;17:475. doi: 10.1007/s00167-009-0722-3. [DOI] [PubMed] [Google Scholar]
- 27.Mesfar W, Shirazi-Adl A. Biomechanics of changes in ACL and PCL material properties or prestrains in flexion under muscle force-implications in ligament reconstruction. Computer methods in biomechanics and biomedical engineering. 2006;9:201–9. doi: 10.1080/10255840600795959. [DOI] [PubMed] [Google Scholar]
- 28.Atkinson P, Atkinson T, Huang C, Doane R. A comparison of the mechanical and dimensional properties of the human medial and lateral patellofemoral ligaments. Orthopaedic Research Society 2000. March 12–15 2000 Orlando, Florida. [Google Scholar]
- 29.Mesfar W, Shirazi-Adl A. Biomechanics of the knee joint in flexion under various quadriceps forces. The knee. 2005;12:424–34. doi: 10.1016/j.knee.2005.03.004. [DOI] [PubMed] [Google Scholar]
- 30.Stäubli HU, Schatzmann L, Brunner P, Rincón L, Nolte LP. Mechanical tensile properties of the quadriceps tendon and patellar ligament in young adults. AmJSports Med. 1999;27:27–34. doi: 10.1177/03635465990270011301. [DOI] [PubMed] [Google Scholar]
- 31.Donahue TLH, Howell SM, Hull ML, Gregersen C. A biomechanical evaluation of anterior and posterior tibialis tendons as suitable single-loop anterior cruciate ligament grafts. Arthroscopy-New York. 2002;18:589–97. doi: 10.1053/jars.2002.32617. [DOI] [PubMed] [Google Scholar]
- 32.Amis AA, Senavongse W, Bull AMJ. Patellofemoral kinematics during knee flexion-extension: An in vitro study. Journal of orthopaedic research. 2006;24:2201–11. doi: 10.1002/jor.20268. [DOI] [PubMed] [Google Scholar]
- 33.Farahmand F, Tahmasbi MN, Amis AA. Lateral force-displacement behaviour of the human patella and its variation with knee flexion-a biomechanical study in vitro. Journal of Biomechanics. 1998;31:1147–52. doi: 10.1016/s0021-9290(98)00125-0. [DOI] [PubMed] [Google Scholar]
- 34.Senavongse W, Amis AA. The effects of articular, retinacular, or muscular deficiencies on patellofemoral joint stability: a biomechanical study in vitro. Journal of Bone and Joint Surgery-British Volume. 2005;87:577–82. doi: 10.1302/0301-620X.87B4.14768. [DOI] [PubMed] [Google Scholar]
- 35.Duchman KR, DeVries NA, McCarthy MA, Kuiper JJ, Grosland NM, Bollier ML. Biomechanical Evaluation of Medial Patellofemoral Ligament Reconstruction. Iowa Orthopaedic Journal. 2013;33:64–9. [PMC free article] [PubMed] [Google Scholar]
- 36.Senavongse W, Farahmand F, Jones J, Andersen H, Bull AMJ, Amis AA. Quantitative measurement of patellofemoral joint stability: force-displacement behavior of the human patella in vitro. Journal of orthopaedic research. 2003;21:780. doi: 10.1016/S0736-0266(03)00061-5. [DOI] [PubMed] [Google Scholar]
- 37.Smirk C, Morris H. The anatomy and reconstruction of the medial patellofemoral ligament. The Knee. 2003;10:221–7. doi: 10.1016/s0968-0160(03)00038-3. [DOI] [PubMed] [Google Scholar]
- 38.Beck P, Brown NAT, Greis PE, Burks RT. Patellofemoral contact pressures and lateral patellar translation after medial patellofemoral ligament reconstruction. AmJSports Med. 2007;35:1557–63. doi: 10.1177/0363546507300872. [DOI] [PubMed] [Google Scholar]
- 39.Yamada Y, Toritsuka Y, Horibe S, Sugamoto K, Yoshikawa H, Shino K. In vivo movement analysis of the patella using a three-dimensional computer model. Journal of Bone and Joint Surgery-British Volume. 2007;89:752. doi: 10.1302/0301-620X.89B6.18515. [DOI] [PubMed] [Google Scholar]
- 40.Lee TQ, Morris G, Csintalan RP. The influence of tibial and femoral rotation on patellofemoral contact area and pressure. JOrthopSports PhysTher. 2003;33:686. doi: 10.2519/jospt.2003.33.11.686. [DOI] [PubMed] [Google Scholar]


