Abstract
Background
Informal caregiving can be deleterious to mental health, but research results are inconsistent and may reflect an interaction between caregiving and vulnerability to stress.
Methods
We examined psychological distress among 1,228 female caregiving and non-caregiving twins. By examining monozygotic and dizygotic twin pairs discordant for caregiving, we assessed the extent to which distress is directly related to caregiving or confounded by common genes and environmental exposures.
Results
Caregiving was associated with distress as measured by mental health functioning, anxiety, perceived stress, and depression. The overall association between caregiving and distress was confounded by common genes and environment for mental health functioning, anxiety, and depression. Common environment also confounded the association of caregiving and perceived stress.
Conclusions
Vulnerability to distress is a factor in predicting caregivers' psychosocial functioning. Additional research is needed to explicate the mechanisms by which common genes and environment increase the risk of distress among informal caregivers.
Keywords: Twins, Caregiving, Psychological distress
Background
The current debate in the US on healthcare costs and service delivery often overlooks the essential role played by informal caregivers and the potential costs that they incur. Informal caregivers are typically family or friends of people who have difficulties with independent living because of physical, cognitive, or emotional impairments. Caregiving duties are extremely diverse and can include important maintenance tasks, such as bathing and transportation, as well as higher-level activities, such as managing finances and medications [1]. Without this help, care recipients would often need to live in institutionalized settings. According to one estimate, the US government relies on more than 65 million informal care-givers, who provide $375 billion worth of unpaid services each year to adult relatives and friends living in the community [2]. Only 5 years earlier, the number of caregivers was estimated to be 44 million, and the value of their services was approximately $306 billion annually [3]. Given the aging of the American population, these staggering figures can only be expected to keep rising.
Clearly, caregivers are a great economic benefit to the US, but many caregivers report feeling burdened by relentless and inescapable duties, family problems, and secondary consequences such as lost work and strained finances [4–6]. Indeed, many investigators have reported that caregivers have higher levels of perceived stress, anxiety, and depressed mood than non-caregivers. This is true for caregivers of people with dementias [7], psychiatric illnesses [8], cancer [9, 10], coronary events [11], AIDS [5], and autism [12]. Caregivers also report higher levels of depressive symptoms and mental health problems when they place family members in nursing homes [13].
However, not all studies find that caregiving is associated with greater distress. In addition to studies that report no difference in distress between caregivers and non-caregivers, some find that caregiving provides benefits to caregivers, and many report a mix of benefits and stressors [1]. Some of the variability in outcomes may be influenced by the characteristics of caregiving situations and the amount of care provided. For example, the mental health consequences of caregiving are believed to increase substantially in women who spend more than 36 h per week caring for a spouse [14].
Even though caregivers often report distress, the degree to which their distress is caused by caregiver exposures remains unclear. Since the first formal research [15], the vast majority of caregiver studies have been observational, but many have included comparison groups (e.g., non-caregivers). Despite the lack of data supporting direct causation between caregiving and distress, a causal role for caregiving has been asserted without controversy for more than a half a century, with prominent researchers continuing to posit that “caregiving causes psychological distress” [16]. The distinction between caregiver status as a correlate or a cause of distress is not just an academic question. It is relevant to policy makers, healthcare providers, caregivers, and care recipients. We know that psychological distress is associated with caregivers' risk for health problems and disabilities [17], and that reductions in depressed mood or improvements in self-rated health decrease the likelihood that caregivers will prematurely place their care recipients in nursing homes [18]. It is, therefore, important to understand what is driving these associations.
Using the diathesis-stress model as a theoretical framework [19], some studies have hypothesized that personal vulnerabilities increase the risk of distress in certain caregivers and interact with the demands of the caregiving environment to exacerbate distress [20]. For example, one study found that among persons with a history of depression, caregivers had a much higher rate of current depression (73 %) than noncaregivers (30 %). However, among persons with no history of depression, caregivers did not have a higher rate of current depression (5 %) than non-caregivers (3 %) [21]. Unfortunately, despite its utility as a guiding framework, adequate testing of the diathesis-stress model requires study designs that go beyond observational data.
Twin research represents an important method for testing hypotheses about causal connections between phenotypes (e.g., traits, exposures, and outcomes), especially in situations where experimental designs are impractical or impossible. Twins who are discordant for a given exposure provide a natural experimental setup for testing the counterfactual framework of causal inference [22–24]. In this approach, the potential effect of an exposure is measured as the difference between outcomes for individuals who are exposed to a particular risk factor and outcomes for those who are not. While it is impossible to observe an individual who is simultaneously exposed and not exposed, phenotype-discordant twin pairs provide a compelling means to evaluate the direct effects of an exposure on an outcome or, alternatively, to assess the possibility of confounding between phenotypes based on common developmental history and shared genetics. Briefly, assuming that two phenotypes—such as caregiving and distress—are related to each other in a standard research sample at the individual level, the observed association is potentially confounded by developmental history (e.g., the effects of growing up in a home with high levels of psychological distress) and by genetic background, either of which might predispose people to assume a caregiving role in later life and to experience psychological distress. Twin studies can disentangle these sources of confounding.
Given the advantages of twin analyses, we examined psychological distress among 1,228 female caregiving and noncaregiving twins from the University of Washington Twin Registry (UWTR) [25, 26]. By examining both monozygotic (MZ) and dizygotic (DZ) twin pairs discordant for caregiver status, we assessed the extent to which psychological distress is directly related to caregiving behavior versus common genes and environmental exposures. Our sample differs from most previous study samples by including caregivers for people with several kinds of illnesses with varying forms of chronicity. It also includes caregivers who have a broad spectrum of relationships with their care recipients (e.g., child, parent, spouse, or friend). We hypothesized that caregivers in our sample would report more psychological distress than non-caregivers. Given the extensive literature on the importance of family history and genetics in current mood and distress [27–29], as well as our previous work on vulnerable caregivers, we expected that the relationship between caregiving and distress would be partially confounded by common environment and shared genetics.
Methods
Participants
The UWTR is a community-based sample of twins recruited from applicants for driver licenses through the Washington State Department of Licensing. Full details of the construction and characteristics of the UWTR are described elsewhere [25]. In brief, driver license numbers in Washington State are created by combining characters from each applicant's name and birth date. To avoid issuing duplicate numbers to twins, who are likely to share both the same surname and the same birth date, the Department of Licensing asks all new applicants if they are members of a twin pair. Because state agencies in Washington are permitted by law to share data, the Department of Licensing regularly sends the UWTR lists of all recent applicants who self-identify as twins. Once UWTR staff receives each list, they invite all twin applicants who are at least 18 years old to join the registry. These index twins may in turn invite their co-twins to enroll, even if they live out of state. All twins complete an initial enrollment survey that includes self-reported assessments of physical and mental health and basic demographic information. Zygosity is then assessed by UWTR staff by using standardized questions about childhood similarity that have been shown to reliably classify zygosity with an accuracy of 95–98 %, compared with zygosity assessment by biological indicators [30].
Data Collection
From 2006 to 2008, a follow-up health survey was mailed to all members of the UWTR, achieving a 59 % overall response rate (n =3,072 individuals). The survey collected self-reported data on demographic indices, height, and weight, as well as physical and mental health behaviors and outcomes. For the present study, all same-sex twin pairs who completed the health survey between 2006 and 2008 and had a known zygosity were eligible for inclusion. Because the resulting sample contained only 39 male caregivers in all, and only 8 DZ male/male pairs discordant for caregiving, we focused exclusively on female twins for our analyses. Our final analytic dataset included 1,228 individual female twins (408 MZ and 206 DZ pairs), of whom 188 were caregivers.
Participants and Caregiving
Demographic information included age, sex, marital status (married or cohabitating vs. single), education (less than high school, high school graduate, or more than high school), and income. We used four questions to assess issues relevant to caregiving. These included (1) the caregiver's relationship to the care recipient, (2) the type of illness of the care recipient, (3) the duration of caregiving, and (4) the degree of distress associated with caregiving (0 = “not at all,” 1 = “a little,” 2 = “somewhat,” and 3 = “very much so”).
Psychosocial Outcomes
Psychological responses to events and experiences include appraisals of their salience, level of threat, controllability, and amenability to coping. Such appraisals influence the degree to which an experience is perceived as stressful or upsetting. We used the 10-item perceived stress scale (PSS; [31]) to assess subjective reactions to demands from stressful experiences. The PSS yields scores from 0 to 40 and has good reliability in our sample (Cronbach's alpha=0.89) and elsewhere [32].
An individual's psychological response to stressors may also include anxiety and depression [33–35]. We used the mental component survey score (MCS) of the Short Form-8 [36], a widely used health status measure, to assess mental health functioning. MCS scores are standardized with a mean of 50 for the general population; higher values reflect better mental health functioning. The Brief Symptom Inventory-A (BSI-A; 6-item anxiety subscale) [37] was used to assess anxiety symptoms. Scores range from 0 to 24. The BSI-A has demonstrated validity and reliability [38]. Cronbach's alpha was 0.85 in our sample. Finally, the Patient Health Questionnaire-2 (PHQ-2; [39]) assessed depressive symptoms. Scores range from 0 to 6, with a score of 3 or higher as the cutoff for classification of depression [39]. The PHQ-2 has good reliability and validity as a screener for clinical depression [40]. Cronbach's alpha was 0.82 in our sample.
Statistical Analysis
We first calculated means and standard deviations for continuous variables and percentages for categorical variables, and then stratified variables by caregiver status and zygosity. We used generalized estimating equations (GEE), with robust standard errors to account for correlations within twin pairs, to evaluate differences between caregivers and noncaregivers. For caregivers, we also calculated correlation coefficients (Spearman's rho) for self-reported distress attributed to caregiving with each of the psychological distress variables. To investigate the individual-level (i.e., overall phenotypic) association between caregiver status and psychological distress, all individual twins were included in models that assessed the cross-sectional relationships between caregiver status and the four psychological distress indicators (0–3). We again fit GEE regression models to account for the lack of independence within twin pairs, and then adjusted for age, which was the only demographic characteristic significantly associated with caregiving between pairs and with psychological distress within pairs. Nevertheless, age was not associated with PHQ-2 depression in these models. We then used linear and logistic regression models as indicated to evaluate continuous and binary or categorical variables, respectively. Although these analyses accounted for the correlations within twin pairs on the variables of interest, the results represent the overall phenotypic effect of caregiver status on psychological distress.
We also estimated the within-twin pair association between caregiving and distress among twins discordant for caregiving. The cross-sectional analysis of individual twins, above, does not directly assess the extent to which differences in psychological distress are predicted by differences in caregiver status within twin pairs. Within-twin pair effects were estimated by calculating the difference between twins within a pair on caregiving status and on each psychological distress variable. Only twin pairs discordant for caregiver status were included in these analyses because concordant pairs would not be informative for our research question. Values for within-twin pair differences were then used in subsequent linear and logistic regression models.
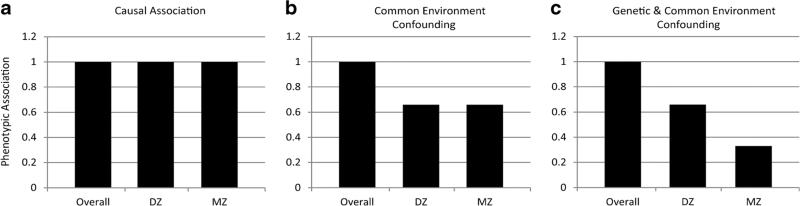
Within-twin pair analyses account for potential confounding factors based on shared genetics and family environment in the overall phenotypic association. Before conducting the regression analyses, we stratified by zygosity to examine the within-twin pair effects in separate regression models for MZ and DZ pairs. If within-twin pair associations for MZ and DZ pairs are equally attenuated in comparison with the overall effect, we can conclude that common environmental exposures contribute to these associations. If within-pair associations for MZ pairs are more attenuated in comparison with the overall effect as well as with the DZ effect, we can conclude that genetic factors also contribute to these associations. Alternately, a within-pair association that remains robust compared to the overall effect provides evidence that familial factors do not play a primary role in the association between caregiver status and mental health. Figure 1, adapted from McGue et al. and Bergen et al. [23, 41], presents this model graphically. Data were analyzed by using IBM SPSS Statistics v.18 (Somers, NY).
Fig. 1.
Interpreting patterns of overall and within-pair associations for causation and confounding in monozygotic (MZ) and dizygotic (DZ) twins. a In causal association, the magnitude of the phenotypic association within pairs is the same overall and for both MZ and DZ pairs. b With common environment confounding, the magnitude of the phenotypic association within pairs is attenuated but not eliminated in MZ and DZ twins compared to the overall association. c With both genetic and common environment confounding, the magnitude of the phenotypic association is attenuated in MZ pairs compared to DZ pairs
For the analyses involving overall phenotypic associations, the total number of caregivers was 188, of whom 68 belonged to 68 caregiving-discordant MZ pairs, 54 belonged to 54 caregiving-discordant DZ pairs, 54 belonged to 27 caregiving-concordant MZ pairs, and 12 belonged to 6 caregiving-concordant DZ pairs. For within-pair analyses, we used only the caregiving-discordant pairs.
Results
Participants and Caregiving
Table 1 presents the sociodemographic profiles of caregivers and non-caregivers, both for all twin pairs and for caregiving-discordant pairs stratified by zygosity. Similarly, Table 2 presents the caregiving characteristics of the caregivers in all pairs and in the discordant pairs stratified by zygosity. In all pairs, caregivers were older and more likely to be married or cohabitating than non-caregivers. Because of the large overall sample, group differences in education were statistically significant but still quite modest. We found no significant associations in the analyses of discordant pairs.
Table 1.
Characteristics of caregivers and non-caregivers in the sample
| Sociodemographic characteristics | All twin pairs (n =614 pairs) |
Caregiving-discordant MZ pairs (n =68 pairs) |
Caregiving-discordant DZ pairs (n =54 pairs) |
|||
|---|---|---|---|---|---|---|
| Caregivers (n = 188) | Non-caregivers (n = 1040) | Caregivers | Non-caregivers | Caregivers | Non-caregivers | |
| Age, mean years (SD) | 43.4 (16.0) | 34.6 (14.3)* | 39.1 (16.0) | 45.1 (16.2) | ||
| Monozygotic, % | 64.9 | 66.7 | 100 | 0 | ||
| Married or living with a partner, % | 59.6 | 49.6** | 55.9 | 49.3 | 55.6 | 57.4 |
| Education, % | ||||||
| Less than high school graduate | 3.7 | 1.6 | 2.9 | 1.5 | 0.0 | 1.9 |
| High school graduate | 12.8 | 8.6 | 13.2 | 10.3 | 16.7 | 14.8 |
| More than high school | 83.5 | 89.8** | 83.8 | 88.2 | 83.3 | 83.3 |
| Annual household income, % | ||||||
| <$20,000 | 17.5 | 22.4 | 19.7 | 21.9 | 15.4 | 14.0 |
| $20,000-$39,999 | 23.0 | 18.7 | 25.8 | 15.6 | 23.1 | 26.0 |
| $40,000-$59,999 | 20.2 | 17.5 | 15.2 | 20.3 | 23.1 | 28.0 |
| $60,000-$79,999 | 12.6 | 13.5 | 13.6 | 18.8 | 9.6 | 14.0 |
| >$80,000 | 27.9 | 26.8 | 25.8 | 23.4 | 28.8 | 18.0 |
p <0.01 between caregivers and non-caregivers
p <0.05 between caregivers and non-caregivers
Table 2.
Characteristics of caregivers in the sample
| Caregiver characteristics |
All twins (n = 188 pairs) |
MZ discordant (n =68 pairs) |
DZ discordant (n =54 pairs) |
|---|---|---|---|
| Years spent caregiving, % | |||
| Less than 1 year | 59.0 | 67.2 | 57.7 |
| 1–2 years | 17.0 | 9.4 | 19.2 |
| Longer than 2 years | 24.0 | 23.4 | 23.1 |
| Relationship to the caregiver, % | |||
| Child | 20.3 | 16.7 | 16.7 |
| Spouse | 8.1 | 4.5 | 13.0 |
| Parent | 17.3 | 15.2 | 9.3 |
| Other relative | 29.9 | 39.4 | 29.6 |
| Friend | 24.4 | 24.2 | 31.5 |
| Type of illness, % | |||
| Acute illness or accident | 36.7 | 34.8 | 43.4 |
| Chronic illness or disability | 30.9 | 31.8 | 37.7 |
| Other | 32.4 | 33.3 | 18.9 |
| Distressed by caregiving, % | |||
| Not at all | 35.8 | 36.8 | 31.5 |
| A little/somewhat | 51.8 | 52.9 | 53.7 |
| Very much so | 12.4 | 10.3 | 14.8 |
Most caregivers reported caring for a friend or relative other than a child, spouse, or parent, with the duration of caregiving less than 1 year. Illnesses among care recipients were almost equally split between acute illnesses or accidents, chronic illnesses, and other types of illness. Approximately 36 % of caregivers reported no distress from caregiving, and distress ratings were significantly correlated with scores for MCS (r =−0.20, p =0.004), PSS (r =0.20, p =0.005), and BSI-A (r =0.15, p =0.018), but not PHQ-2 (r =0.00, p =0.96).
Psychosocial Outcomes
Table 3 shows the estimated marginal means and standard deviations for all twin pairs and for caregiving-discordant pairs stratified by zygosity on the four major outcomes, adjusted for age. As expected, caregivers were significantly more distressed than non-caregivers across all four psychological distress outcomes in the overall sample, but not in the caregiving-discordant pairs. In within-pair models, only BSIA in caregiving-discordant DZ pairs remained significant.
Table 3.
Estimated marginal mean differences for mental health outcomes for female twins by caregiver statusa
| Psychological distress/perceived stress | All twin pairs (n =614 pairs) |
Caregiving-discordant MZ pairs (n =64 pairs) |
Caregiving-discordant DZ pairs (n =58 pairs) |
|||
|---|---|---|---|---|---|---|
| Caregivers (n =188) | Non-caregivers (n =1040) | Caregivers (n =64) | Non-caregivers (n =64) | Caregivers (n =58) | Non-caregivers (n =58) | |
| MCS, M (SE) | 46.7 (0.8) | 49.0 (0.3)b | 47.6 (1.1) | 48.5 (1.2) | 47.7 (1.2) | 49.3 (1.2) |
| BSI-A, M (SE) | 4.1 (0.4) | 2.7 (0.1)b | 3.9 (0.5) | 3.0 (0.4) | 3.5 (0.5) | 2.2 (0.3)b |
| PSS, M (SE) | 15.4 (0.6) | 13.9 (0.2)b | 14.5 (0.9) | 14.1 (0.9) | 14.5 (0.9) | 14.0 (0.9) |
| PHQ-2 Depression, %c | 14.0 | 8.9b | 13.2 | 11.8 | 9.3 | 7.4 |
BSI-A Brief Symptom Inventory-A, DZ dizygotic, MCS SF-8 mental component summary, MZ monozygotic, PHQ-2 Patient Health Questionnaire-2, and PSS perceived stress scale
Analyses are adjusted for age, which was a significant covariate in all models except PHQ-2
Indicates that caregivers and non-caregivers significantly differed on psychological distress at p <0.05
Percentages are provided for participants who scored 3 or higher on the PHQ-2
The left half of Table 4 presents the linear and logistic regressions used to test caregiver status as a predictor of differences in the four outcome variables among twin pairs. The right half contains the within-pair results for the DZ and MZ pairs. To interpret these results, we used Fig. 1 as our theoretical framework and Fig. 2a–d as the framework's empirical realization (see [23, 41]). The likelihood of direct causal effects is reduced to the extent that the within-pair associations are smaller than the overall associations.
Table 4.
Overall and within-twin pair associations of caregiver status with psychological distress and perceived stressa
| Outcome | Overall GEE females n =614 twin pairsb |
Within-twin pair females n =68 caregiving-discordant MZ pairs n = 54 caregiving-discordant DZ pairs |
|||||
|---|---|---|---|---|---|---|---|
| B or OR | 95 % CI | p | Zygosity | B or OR | 95 % CI | p | |
| MCS | –2.35 | (–4.0, –0.7) | 0.006 | MZ | –1.05 | (–3.8, 1.7) | 0.47 |
| DZ | –1.56 | (–5.1, 2.0) | 0.39 | ||||
| BSI-A | 1.43 | (0.7, 2.1) | 0.001 | MZ | 0.92 | (–0.1, 1.9) | 0.08 |
| DZ | 1.25 | (0.0, 2.5) | 0.05 | ||||
| PSS | 1.47 | (0.3, 2.6) | 0.01 | MZ | 0.35 | (–1.6, 2.3) | 0.73 |
| DZ | 0.36 | (–2.0, 2.8) | 0.77 | ||||
| PHQ-2 | 1.66c | (1.0, 2.8) | 0.05 | MZ | 1.153 | (0.4, 3.5) | 0.80 |
| DZ | 1.433 | (0.2, 11.8) | 0.74 | ||||
BSI-A Brief Symptom Inventory-A, DZ dizygotic, GEE generalized estimating equations, MCS SF-8 mental component summary, MZ monozygotic, OR odds ratio, PHQ-2 Patient Health Questionnaire-2, PSS perceived stress scale
All analyses are adjusted for age
Of these 614 twin pairs, 68 are caregiving-discordant MZ pairs, 54 are caregiving-discordant DZ pairs, 27 are caregiving-concordant MZ pairs, and 6 are caregiving-concordant DZ pairs
Analyses are binary and odds ratios are reported
Fig. 2.
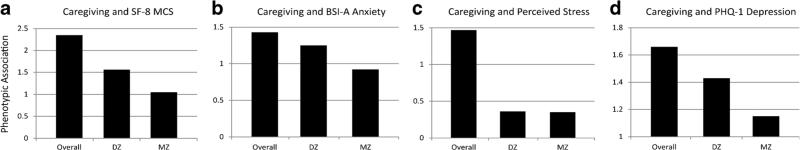
Patterns of overall and within-pair associations for caregiving and psychological distress. a For caregiving and the mental component survey score of the Short Form-8 (SF-8 MCS), the magnitude of the phenotypic association decreases with increasingly rigorous control of familial factors. This suggests that common environmental factors and genetics both contribute to the association. b For caregiving and anxiety scores on the Brief Symptom Inventory-A (BSI-A), the magnitude of the phenotypic association decreases with increasingly rigorous control of familial factors. This suggests that common environmental factors and genetics both contribute to the association. c For caregiving and perceived stress, the magnitude of the phenotypic association decreases equally for both dizygotic (DZ) and monozygotic (MZ) pairs. This suggests that common environmental factors contribute to the association. d For caregiving and depression scores on the Patient Health Questionnaire-2 (PHQ-2), the magnitude of the phenotypic association decreases with increasingly rigorous control of familial factors. This suggests that common environmental factors and genetics both contribute to the association
In the GEE cross-sectional analyses (Table 4), caregivers reported poorer mental health functioning than did noncaregivers. However, the smaller regression coefficients within DZ pairs and the additional attenuation within MZ pairs (Fig. 2a) suggests that this overall effect was confounded by both common environmental and genetic factors, and that the effect was not completely direct or causal.
Caregivers also reported higher anxiety than noncaregivers, but familial confounding, especially genetics, appears to play a role in this association (Fig. 2b). The within-pair difference regression coefficient for the DZ twins was only slightly smaller than the individual-level coefficient, but the MZ coefficient was further attenuated. Even with some familial confounding, a direct causal effect is more plausible for anxiety than for our other measures of psychological distress.
In addition, caregivers reported higher perceived stress than non-caregivers, but the within-twin pair associations suggest that almost all of this effect was confounded by common environmental factors (Fig. 2c). Given the near equivalence between within-twin pair results for both DZ and MZ pairs, we see little evidence for genetic confounding. Perceived stress in the context of caregiving appears to be strongly determined by common family environment rather than by a direct causal mechanism.
Table 4 shows an increase in the odds of depression for caregivers versus non-caregivers. However, the within-twin pair odds ratios for MZ and DZ pairs are small, suggesting that this overall effect is significantly confounded by the combination of common environmental and genetic factors (Fig. 2d) and is not primarily causal.
Discussion
This is the first study to investigate the relationship between caregiving and psychological distress while controlling for important familial factors, including common environment and shared genetics. At the individual level, we replicated the typical finding that caregiving is modestly but significantly associated with psychological distress as measured by overall mental health functioning, anxiety, perceived stress, and depression. However, the overall phenotypic association between caregiving and distress is confounded by both common environment and shared genetics in the case of mental health functioning, anxiety, and depression. Common environment also confounds the association of caregiving and perceived stress.
These results are consistent with prior findings that vulnerability is a major factor in the prediction of psychosocial and physiological functioning in caregivers of people with dementia [20, 42]. Based on the diathesis-stress model, such research suggested that distress is a function both of exposure to stressors and of vulnerable phenotypes that increase the risk of distress. Within the field of diathesis-stress research, these vulnerable phenotypes may be a function of genetics, developmental history (i.e., common environment), age, gender, disposition, and race [19, 33, 43, 44]. In the present study, it appears that both genetics and common environment are relevant to understanding the connection between caregiving and distress.
Within the broader literature on environmental contributions to health and disease, several potential candidates might explain how common environmental exposures contribute to psychological distress as well as the likelihood of becoming a caregiver. First and foremost, socioeconomic status is a predictor of both physical and mental health, since lower income is associated with greater morbidity and mortality [45, 46] as well as higher risk for psychiatric diagnoses [47, 48]. Moreover, lower-income individuals may lack access to health insurance [49] or other necessities, such as child care and transportation [50], leaving informal caregiving as the only healthcare option in many situations. As Conger and colleagues have shown, children reared under conditions of economic hardship, marital distress, or disrupted parenting are at higher risk for mental health problems such as depression [51, 52]. Mental health problems, in turn, may hinder educational and employment opportunities [53], such that informal caregiving becomes the only viable option for some people who are vulnerable to psychological distress. Exposure to any combination of these physical and mental health risk factors could explain how caregiving and psychological distress are linked by a mechanism of common environmental exposures.
Formulating a genetic link between caregiving and psychological distress is a little more difficult than identifying a common environmental link, but a likely candidate emerges from literature showing that exposure to certain life events is partially heritable and linked with psychological distress (see, e.g., [29] for a summary). For example, Kendler et al. [28, 54] have shown that, among women, stressful life events predict the genetic risk for onset of major depressive disorder, and that people at risk for depression are more likely to experience stressful life events, including interpersonal and economic strain. Of particular relevance to the present study, Saudino et al. [55] found that the genetic variance of controllable, desirable, and undesirable life events was significant and entirely explained by personality dimensions, including neuroticism, extraversion, and openness to experience. Their finding is particularly important because those personality dimensions are partially determined by genetics and have shared genetic variance with a number of measures of psychological functioning, including depression and anxiety [28, 55, 56]. Thus, certain heritable personality traits may explain the shared genetic association between caregiving and psychological distress.
More research is clearly needed to explicate the mechanisms by which common environmental exposures and shared genetics increase the risk of psychological distress among informal caregivers. However, such research should complement, not replace, research and policy decisions that support informal caregivers and reduce the burdens that they experience. Although our results show that the association between caregiving and distress is partially confounded by common environment and shared genetics, a portion of the relationship still appears to be direct, especially for anxiety. Reducing health disparities and increasing access to healthcare and preventive services would likely pay dividends, not only for adults who are caregivers now but also for young people growing up in households of low socioeconomic status and other stressful environments. Providing access to care and reducing morbidity over the lifespan could provide benefits for individual health as well as for the quality of life of millions of people who might otherwise need to care for sick family members and friends.
Limitations
The primary limitation of the present study is that our care-giver sample was more heterogeneous than those in most caregiver studies in terms of the care recipients' illnesses, the relationship of caregivers with care recipients (55.4 % were caring for a friend or relative other than a child, spouse, or parent), and the duration of caregiving (50 % provided care for less than 1 year). Nevertheless, this heterogeneity may also be advantageous, since most previous caregiver research has focused on homogenous samples of caregivers and care recipients. Our sample may, thus, be more externally valid across all types of caregivers than those in other studies.
An exception to this statement, as well as a secondary limitation of our study, is the fact that our sample was entirely female and, therefore, may not generalize to male caregivers.
To take full advantage of our sample, we would need to compare larger subgroups in terms of their relationships with distress and the influence of genotype and family background. Thus, a third limitation of our study is that, despite the large size of our full sample (n = 188 caregivers) and our sample of caregiving-discordant twin pairs (n = 122 caregivers), we would still need a larger sample to test additional mechanisms of genetic and environmental mediation, above and beyond the modest associations that we detected between caregiving and distress.
Finally, we note that we derived our data from a large survey on general health issues and did not use a standard questionnaire on caregiving burden. Future research would benefit from using a standard caregiving questionnaire to provide more direct comparisons with other published studies.
Recommendations, Advances, and Conclusions
The US faces two major challenges involving health care and the resources required to pay for it. First, we are experiencing an increasing prevalence of people living with chronic diseases. Second, in a period of recession and slow economic recovery, funds are insufficient to provide long-term care for everyone who is chronically ill. These conditions have catapulted informal caregivers into important positions. Although the careful allocation of healthcare funds has already included triage to the most vulnerable care recipients, little research has focused on identifying the most vulnerable care-givers. Informal caregivers are a first line of defense against the need for institutionalization in the face of scarce public funds. Policy makers are well advised to help caregivers remain independent and maintain the highest possible quality of life, both for themselves and for their care recipients.
Despite 50 years of formal caregiver research, we still need to find optimal ways to identify caregivers at the highest risk for psychological distress. Caregiver distress is associated with and predictive of risky health behaviors, physiological dysregulation, and cognitive problems, as well as long-term illness, disability, and mortality [20, 57–62]. The present findings suggest that exposure to caregiving may influence distress (especially anxiety), but personal vulnerabilities such as family history and genetics play major roles in caregiver distress. Although we [42] hypothesized the importance of these factors in caregiver distress more than 20 years ago, the type of data needed to test this hypothesis was simply not available then. The present study design enabled us to examine the relative importance of caregiver status, genotype, and family history.
Our findings extend a large and important caregiver literature by demonstrating, for the first time, the linkages between caregiver status, family history, and genetic predisposition to psychological distress. These results have substantial implications for interventions that focus on all caregivers, and not simply on vulnerable caregivers. Nevertheless, interventions targeting caregivers who are at genetic or familial risk for psychological distress, as well as for more serious mental health problems, may be more efficacious and yield greater social and economic benefits than interventions targeting all caregivers.
Acknowledgments
This research was supported by the National Institutes of Health grants RC2 HL103416 (D. Buchwald) and R01 AR051524 (N. Afari) and AG023629 (P. Vitaliano). We wish to thank the twins for taking part in the University of Washington Twin Registry and for their time and enthusiasm for this project.
Footnotes
Conflict of Interest The authors have no conflict of interest to disclose.
Contributor Information
Peter P. Vitaliano, Department of Psychiatry and Behavioral Sciences, University of Washington, PO Box 356560, Seattle, WA 98195, USA
Eric Strachan, Department of Psychiatry and Behavioral Sciences, University of Washington, PO Box 356560, Seattle, WA 98195, USA The University of Washington Twin Registry, Seattle, WA, USA.
Elizabeth Dansie, Department of Anesthesiology and Pain Medicine, University of Washington, Seattle, WA, USA
Jack Goldberg, Department of Epidemiology, University of Washington, Seattle, WA, USA The University of Washington Twin Registry, Seattle, WA, USA.
Dedra Buchwald, Department of Epidemiology, University of Washington, Seattle, WA, USA Department of Medicine, University of Washington, Seattle, WA, USA; The University of Washington Twin Registry, Seattle, WA, USA; Center for Clinical and Epidemiological Research, University of Washington, 1100 Olive Way, Suite 1200, Seattle, WA 98101, USA.
References
- 1.National Alliance for Caregiving, AARP . Caregiving in the US. Washington, DC: 2009. [Google Scholar]
- 2.Rosalynn Carter Institute for Caregiving . Averting the caregiving crisis: Why we must act now. Americus, GA: 2010. pp. 5–12. [Google Scholar]
- 3.National Alliance for Caregiving, AARP . Caregiving in the US. Washington, DC: 2004. [Google Scholar]
- 4.Marks NF, Lambert JD, Choi H. Transitions to caregiving, gender, and psychological well-being: A prospective US national study. J Marriage Fam. 2002;64:657–667. [Google Scholar]
- 5.Pearlin LI, Semple S, Turner H. Stress of AIDS caregiving: A preliminary overview of the issues. Death Stud. 1988;12:5–6. doi: 10.1080/07481188808252266. [DOI] [PubMed] [Google Scholar]
- 6.Shahly V, Chatterji S, Gruber M, et al. Cross-national differences in the prevalence and correlates of burden among older family care-givers in the World Health Organization World Mental Health (WMH) Surveys. Psychol Med. 2012;9:1–15. doi: 10.1017/S0033291712001468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pinquart M, Sorensen S. Differences between caregivers and noncaregivers in psychological health and physical health: A meta-analysis. Psychol Aging. 2003;18:250–267. doi: 10.1037/0882-7974.18.2.250. [DOI] [PubMed] [Google Scholar]
- 8.Dyck DG, Short R, Vitaliano PP. Predictors of burden and infectious illness in schizophrenia caregivers. Psychosom Med. 1999;61:411–419. doi: 10.1097/00006842-199907000-00001. [DOI] [PubMed] [Google Scholar]
- 9.Lutgendorf SK, De Geest K, Bender D, et al. Social influences on clinical outcomes of patients with ovarian cancer. J Clin Oncol. 2012;30:2885–2890. doi: 10.1200/JCO.2011.39.4411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mosher CE, Danoff-Burg S. Psychosocial impact of parental cancer in adulthood: A conceptual and empirical review. Clin Psychol Rev. 2005;25:365–382. doi: 10.1016/j.cpr.2004.12.003. [DOI] [PubMed] [Google Scholar]
- 11.Molloy GJ, Johnston DW, Witham MD. Family caregiving and congestive heart failure. Review and analysis. Eur J Heart Fail. 2005;7:592–603. doi: 10.1016/j.ejheart.2004.07.008. [DOI] [PubMed] [Google Scholar]
- 12.Schieve LA, Blumberg SJ, Rice C, Visser SN, Boyle C. The relationship between autism and parenting stress. Pediatrics. 2007;119:114–121. doi: 10.1542/peds.2006-2089Q. [DOI] [PubMed] [Google Scholar]
- 13.Whitlatch CJ, Feinberg LF, Stevens EJ. Predictors of institutionalization for persons with Alzheimer's disease and the impact on family caregivers. J Ment Health Aging. 1999;5:275–288. [Google Scholar]
- 14.Miller B, Cafasso L. Gender differences in caregiving: Fact or artifact? Gerontologist. 1992;32:498–507. doi: 10.1093/geront/32.4.498. [DOI] [PubMed] [Google Scholar]
- 15.Grad J, Sainsbury P. Mental illness and the family. Lancet. 1963;1:544–547. doi: 10.1016/s0140-6736(63)91339-4. [DOI] [PubMed] [Google Scholar]
- 16.Schulz R, Sherwood PR. Physical and mental health effects of family caregiving. Am J Nurs. 2008;108:23–27. doi: 10.1097/01.NAJ.0000336406.45248.4c. quiz 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Vitaliano P, Echeverria D, Shelkey M, Zhang JP, Scanlan J. A cognitive psychophysiological model to predict functional decline in chronically stressed older adults. J Clin Psychol Med S. 2007;14:177–190. [Google Scholar]
- 18.Mittelman MS. A family intervention to delay nursing home placement of patients with Alzheimer's disease. A randomized controlled trial. J Am Med Assoc. 1996;276:1725–1731. [PubMed] [Google Scholar]
- 19.Zubin J, Spring B. Vulnerability—a new view of schizophrenia. J Abnorm Psychol. 1977;86:103–126. doi: 10.1037//0021-843x.86.2.103. [DOI] [PubMed] [Google Scholar]
- 20.Vitaliano PP, Zhang J, Scanlan JM. Is caregiving hazardous to one's physical health? A meta-analysis. Psychol Bull. 2003;129:946–972. doi: 10.1037/0033-2909.129.6.946. [DOI] [PubMed] [Google Scholar]
- 21.Russo J, Vitaliano PP, Brewer DD, Katon W, Becker J. Psychiatric disorders in spouse caregivers of care recipients with Alzheimer's disease and matched controls: A diathesis-stress model of psychopathology. J Abnorm Psychol. 1995;104:197–204. doi: 10.1037//0021-843x.104.1.197. [DOI] [PubMed] [Google Scholar]
- 22.Little RJ, Rubin DB. Causal effects in clinical and epidemiological studies via potential outcomes: Concepts and analytical approaches. Annu Rev Publ Health. 2000;21:121–145. doi: 10.1146/annurev.publhealth.21.1.121. [DOI] [PubMed] [Google Scholar]
- 23.McGue M, Osler M, Christensen K. Causal inference and observational research: The utility of twins. Perspect Psychol Sci. 2010;5:546–556. doi: 10.1177/1745691610383511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rubin DB. For objective causal inference, design trumps analysis. Ann Appl Stat. 2008;2:808–840. [Google Scholar]
- 25.Afari N, Noonan C, Goldberg J, et al. University of Washington Twin Registry: Construction and characteristics of a community-based twin registry. Twin Res Hum Genet. 2006;9:1023–1029. doi: 10.1375/183242706779462543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Strachan E, Hunt C, Afari N, et al. The University of Washington Twin Registry: Poised for the next generation of twin research. Twin Res Hum Genet. 2012:1–8. doi: 10.1017/thg.2012.124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kendler KS, Prescott CA. A population-based twin study of lifetime major depression in men and women. Arch Gen Psychiat. 1999;56:39–44. doi: 10.1001/archpsyc.56.1.39. [DOI] [PubMed] [Google Scholar]
- 28.Kendler KS, Kessler RC, Walters EE, et al. Stressful life events, genetic liability, and onset of an episode of major depression in women. Am J Psychiat. 1995;152:833–842. doi: 10.1176/ajp.152.6.833. [DOI] [PubMed] [Google Scholar]
- 29.Federenko IS, Schlotz W, Kirschbaum C, Bartels M, Hellhammer DH, Wust S. The heritability of perceived stress. Psychol Med. 2006;36:375–385. doi: 10.1017/S0033291705006616. [DOI] [PubMed] [Google Scholar]
- 30.Reed T, Plassman BL, Tanner CM, Dick DM, Rinehart SA, Nichols WC. Verification of self-report of zygosity determined via DNA testing in a subset of the NAS-NRC Twin Registry 40 years later. Twin Res Hum Genet. 2005;8:362–367. doi: 10.1375/1832427054936763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Heal Soc Behav. 1983;24:385–396. [PubMed] [Google Scholar]
- 32.Mitchell AM, Crane PA, Kim Y. Perceived stress in survivors of suicide: Psychometric properties of the perceived stress scale. Res Nurs Health. 2008;31:576–585. doi: 10.1002/nur.20284. [DOI] [PubMed] [Google Scholar]
- 33.Lazarus RS, Folkman S. Stress, Appraisal, and Coping. Springer Publishing Company; New York: 1984. [Google Scholar]
- 34.Leventhal H, Brown D, Shacham S, Engquist G. Effects of preparatory information about sensations, threat of pain, and attention on cold pressor distress. J Pers Soc Psychol. 1979;37:688–714. doi: 10.1037//0022-3514.37.5.688. [DOI] [PubMed] [Google Scholar]
- 35.Selye H. The Stress of Life. McGraw-Hill; New York: 1956. [Google Scholar]
- 36.Ware J, Kosinski M, Dewey J, Gandek B. A Manual for Users of the SF-8 Health Survey. Quality Metrics Inc.; Lincoln, RI: 2001. [Google Scholar]
- 37.Derogatis LR, Melisaratos N. The brief symptom inventory: An introductory report. Psychol Med. 1983;13:595–605. [PubMed] [Google Scholar]
- 38.De Jong MM, An K, McKinley S, Garvin BJ, Hall LA, Moser DK. Using a 0–10 scale for assessment of anxiety in patients with acute myocardial infarction. Dimens Crit Care Nurs. 2005;24:139–146. doi: 10.1097/00003465-200505000-00008. [DOI] [PubMed] [Google Scholar]
- 39.Kroenke K, Spitzer RL, Williams JB. The Patient Health Questionnaire-2: Validity of a two-item depression screener. Med Care. 2003;41:1284–1292. doi: 10.1097/01.MLR.0000093487.78664.3C. [DOI] [PubMed] [Google Scholar]
- 40.Daig I, Herschbach P, Lehmann A, Knoll N, Decker O. Gender and age differences in domain-specific life satisfaction and the impact of depressive and anxiety symptoms: A general population survey from Germany. Qual Life Res. 2009;18:669–678. doi: 10.1007/s11136-009-9481-3. [DOI] [PubMed] [Google Scholar]
- 41.Bergen SE, Kendler KS, Gardner CO, Aggen SH. Socioeconomic status and social support following illicit drug use: Causal pathways or common liability? Twin Res Hum Genet. 2008;11:266–274. doi: 10.1375/twin.11.3.266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Vitaliano PP, Russo J, Young HM, Teri L, Maiuro RD. Predictors of burden in spouse caregivers of individuals with Alzheimer's disease. Psychol Aging. 1991;6:392–402. doi: 10.1037//0882-7974.6.3.392. [DOI] [PubMed] [Google Scholar]
- 43.Monroe SM, Simmons AD. Diathesis-stress theories in the context of life stress research: Implications for the depressive disorders. Psychological Bulletin. 1991;110:406–425. doi: 10.1037/0033-2909.110.3.406. [DOI] [PubMed] [Google Scholar]
- 44.Robins LN. Sturdy childhood predictors of adult antisocial behavior: Replications from longitudinal studies. Psychol Med. 1978;8:611–622. doi: 10.1017/s0033291700018821. [DOI] [PubMed] [Google Scholar]
- 45.Adler NE, Coriell M. Socioeconomic status and health: Do we know what explains the association? Adv J Mind Body Health. 1995;11:6–9. [Google Scholar]
- 46.Adler N, Boyce T, Chesney M, et al. Socioeconomic status and health. The challenge of the gradient. Am Psychol. 1994;49:15–24. doi: 10.1037//0003-066x.49.1.15. [DOI] [PubMed] [Google Scholar]
- 47.Regier DA. The linkage of health care reform and health services research. Am J Psychiat. 1993;150:1613–1615. doi: 10.1176/ajp.150.11.1613. [DOI] [PubMed] [Google Scholar]
- 48.Bourdon K, Rae D, Narrow W, Manderschild R, Regier D. National prevalence and treatment of mental and addictive disorders. In: Mandershild R, Sonnenschein M, editors. Mental Health, United States. Vol. 1994. Center for Mental Health Services; Washington, DC: 1994. pp. 22–51. [Google Scholar]
- 49.McGinnis JM, Williams-Russo P, Knickman JR. The case for more active policy attention to health promotion. Health Affair. 2002;21:78–93. doi: 10.1377/hlthaff.21.2.78. [DOI] [PubMed] [Google Scholar]
- 50.McGrath E. Women and Depression: Risk Factors and Treatment Issues: Final Report of the American Psychological Association's National Task Force on Women and Depression. American Psychological Association; Washington, DC: 1990. American Psychological Association National Task Force on Women and Depression. [Google Scholar]
- 51.Conger RD, Wallace LE, Sun Y, Simons RL, McLoyd VC, Brody GH. Economic pressure in African-American families: A replication and extension of the family stress model. Dev Psychol. 2002;38:179–193. [PubMed] [Google Scholar]
- 52.Conger RD, Conger KJ, Martin MJ. Socioeconomic status, family processes, and individual development. J Marriage Fam. 2010;72:685–704. doi: 10.1111/j.1741-3737.2010.00725.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Murray CJ, Lopez AD. Global mortality, disability, and the contribution of risk factors: Global Burden of Disease Study. Lancet. 1997;349:1436–1442. doi: 10.1016/S0140-6736(96)07495-8. [DOI] [PubMed] [Google Scholar]
- 54.Kendler KS, Karkowski-Shuman L. Stressful life events and genetic liability to major depression: Genetic control of exposure to the environment? Psychol Med. 1997;27:539–547. doi: 10.1017/s0033291797004716. [DOI] [PubMed] [Google Scholar]
- 55.Saudino KJ, Pedersen NL, Lichtenstein P, McClearn GE, Plomin R. Can personality explain genetic influences on life events? J Pers Soc Psychol. 1997;72:196–206. doi: 10.1037//0022-3514.72.1.196. [DOI] [PubMed] [Google Scholar]
- 56.Hansell NK, Wright MJ, Medland SE, et al. Genetic comorbidity between neuroticism, anxiety/depression, and somatic distress in a population sample of adolescent and young adult twins. Psychol Med. 2012;42:1249–1260. doi: 10.1017/S0033291711002431. [DOI] [PubMed] [Google Scholar]
- 57.Schulz R, Beach SR. Caregiving as a risk factor for mortality—The caregiver health effects study. J Amer Med Assoc. 1999;282:2215–2219. doi: 10.1001/jama.282.23.2215. [DOI] [PubMed] [Google Scholar]
- 58.Vitaliano PP, Scanlan JM, Zhang J, Savage MV, Hirsch IB, Siegler IC. A path model of chronic stress, the metabolic syndrome, and coronary heart disease. Psychosom Med. 2002;64:418–435. doi: 10.1097/00006842-200205000-00006. [DOI] [PubMed] [Google Scholar]
- 59.Vitaliano PP, Zhang J, Young HM, Caswell LW, Scanlan JM, Echeverria D. Depressed mood mediates decline in cognitive processing speed in caregivers. Gerontologist. 2009;49:12–22. doi: 10.1093/geront/gnp004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Vitaliano PP, Persson R, Kiyak A, Saini H, Echeverria D. Caregiving and gingival symptom reports: Psychophysiologic mediators. Psychosom Med. 2005;67:930–938. doi: 10.1097/01.psy.0000188485.65153.7b. [DOI] [PubMed] [Google Scholar]
- 61.Kiecolt-Glaser JK, Glaser R, Gravenstein S, Malarkey WB, Sheridan J. Chronic stress alters the immune response to influenza virus vaccine in older adults. Proc Natl Acad Sci U S A. 1996;93:3043–3047. doi: 10.1073/pnas.93.7.3043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Kiecolt-Glaser JK, Marucha PT, Malarkey WB, Mercado AM, Glaser R. Slowing of wound healing by psychological stress. Lancet. 1995;346:1194–1196. doi: 10.1016/s0140-6736(95)92899-5. [DOI] [PubMed] [Google Scholar]