Abstract
Background and Objectives
Pre- and/or intra-operative use of diuretics, angiotensin-converting enzyme inhibitors (ACE-I) or angiotensin II receptor blockers (ARB) constitutes a potentially modifiable risk factor for postoperative acute kidney injury (AKI). It has been studied whether use of these drugs predicts AKI after cardiac surgery. The objective of this study was to examine whether administration of these agents was independently associated with AKI after non-cardiac surgery.
Design, Setting, Participants, and Measurements
This was a retrospective observational study. Inclusion criteria were adult patients (age ≥ 18) who underwent non-cardiac surgery under general anesthesia from 2007 to 2009 at Kyoto Katsura Hospital. Exclusion criteria were urological surgery, missing creatinine values, and preoperative dialysis. The exposures of interest were pre- and/or intra-operative use of diuretics or ACE-I/ARB. Outcome variables were postoperative AKI as defined by the AKI Network (increase in creatinine ≥ 0.3 mg/dL or 150% within 48 hours, or urine output < 0.5 ml/kg/hour for > 6 hours). Multivariable logistic regression analyses were conducted and adjusted for potential confounders. Propensity scores (PS) for receiving diuretics or ACE-I/ARB therapy were estimated and PS adjustment, PS matching, and inverse probability weighting were performed.
Results
There were 137 AKI cases (5.0%) among 2,725 subjects. After statistical adjustment for patient and surgical characteristics, odds (95% CI) of postoperative AKI were 2.07 (1.10-3.89) (p = 0.02) and 0.89 (0.56-1.42) (p = 0.63) in users of diuretics and ACE-I/ARB, respectively, compared with non-users. PS adjustment, PS matching, and inverse probability weighting yielded similar results. The effect size of diuretics was significantly greater in the patients with lower propensity for diuretic use (p for interaction < 0.1).
Conclusions
Prescription of diuretics, but not ACE-I/ARB, was independently associated with postoperative AKI after non-cardiac surgery, especially in patients with low propensity for diuretic use. It might be reasonable to withhold preoperative diuretics in these patients.
Introduction
Postoperative acute kidney injury (AKI) is a serious complication of surgical procedures that is associated not only with short-term increases in mortality [1–3] but also with long-term complications such as development of chronic kidney disease [4]. Predictors of postoperative AKI have been extensively studied in cardiac surgery [5–22], and to a lesser extent in non-cardiac surgery [23–30].
As reported in previous studies, these predictors include age, female sex, types of surgery (valvular surgery versus coronary artery bypass grafting in cardiac surgery and intra-thoracic or intra-abdominal surgery versus others in non-cardiac surgery), emergency surgery, preoperative renal dysfunction, body mass index (BMI), smoking, diabetes mellitus (DM), the use of insulin, hypertension, chronic obstructive pulmonary disease (COPD), atrial fibrillation, peripheral arterial disease (PAD), cerebrovascular disease (CVA), coronary artery disease (CAD), preoperative hematocrit, coagulopathy, thrombocytopenia, the use of vasopressors, left ventricular dysfunction, pre- and/or intra-operative use of iodinated contrast, diuretics, angiotensin converting enzyme inhibitors (ACE-I) and angiotensin receptor blockers (ARB) [5–30]. Among these predictors of AKI, pre- and/or intra-operative use of diuretics, ACE-I or ARB is possibly modifiable. There are several studies that examined the association of ACE-I or ARB with AKI after cardiac surgery with conflicting results [17–19, 22], while a meta-analysis showed that the use of ACE-I/ARB was significantly associated with increased odds of postoperative AKI and mortality [21]. The studies that examined the association between preoperative use of ACE-I/ARB and postoperative AKI in non-cardiac surgery were of small sample size [26, 28]. To our knowledge, no studies have investigated whether use of diuretics is associated with postoperative AKI in non-cardiac surgery. We hypothesized that pre- and/or intra-operative use of diuretics or ACE-I/ARB is independently associated with AKI after non-cardiac surgery, and tested this hypothesis in a single-center, retrospective cohort study.
Materials and Methods
Study Design, Settings and Patients
This was a single center, retrospective cohort study. Inclusion criteria were adult patients (age ≥ 18) who underwent non-cardiac surgery under general anesthesia from 2007–2009 at Kyoto Katsura Hospital. Patients were excluded if they had undergone urological surgery (because changes in creatinine due to nephrectomy or ureteral manipulation are likely to be caused by different mechanisms from those underlying other postoperative AKI), were missing creatinine values within 1 week preoperatively or 48 hours postoperatively, or had undergone dialysis preoperatively. The exposures of interest were pre- and/or intra-operative use of diuretics, ACE-I and/or ARB. Intra-operative use of diuretics was included as it is a common practice in Japan to administer diuretics intra-operatively to maintain urine output. If urine output increases in response to diuretic administration, and serum creatinine does not increase postoperatively, the patient is not diagnosed with postoperative AKI. Thus, intra-operative use of diuretics is not a result of AKI but considered to be a risk factor for postoperative AKI. The outcome variable was postoperative AKI as defined by the AKI Network (increase in creatinine ≥ 0.3 mg/dL or 150% within 48 hours, or urine output < 0.5 ml/kg/hour for > 6 hours) within 2 days postoperatively [31]. The data was collected from review of medical charts.
Definitions
Pre- and/or intra-operative use of diuretics and ACE-I/ARB was defined as the use of these agents from the preoperative period through the end of surgery, as confirmed by medication lists in medical charts. Operations were divided into 4 categories: intra-thoracic surgery, intra-abdominal surgery, surgery with large fluid shift and others. Surgery with large fluid shift included total hysterectomy and replacement of major joints such as hips and knees. Estimated glomerular filtration rate (eGFR) was calculated using the equation developed for Japanese populations by the Japanese Society of Nephrology [32], based on the preoperative creatinine value closest to the time of surgery. The use of vasopressors (norepinephrine, epinephrine, phenylephrine, dopamine and ephedrine) was defined as intra-operative administration of these agents. The use of non-steroidal anti-inflammatory drugs (NSAIDs) and iodinated contrast was defined as the use of these agents within 48 hours pre-operatively or their administration intra-operatively. Chronic kidney disease (CKD) was defined as eGFR < 60 ml/min/1.73m2.
Statistical Methods
Continuous variables were expressed as median with interquartile range and were compared using the Mann-Whitney test. Categorical variables were expressed as number with percentage and were compared using the Chi-square test. A multivariable logistic regression model was used to estimate odds ratios and 95% confidence intervals (CIs) of postoperative AKI following the use of diuretics or ACE-I/ARB, with non-users of these agents as a reference. Pre-specified covariates forced into the models included pre- and/or intra-operative use of diuretics and ACE-I/ARB. Other covariates were selected using the backward elimination method by likelihood ratio test. CKD was used as a covariate rather than eGFR as the latter was not significantly associated with postoperative AKI when analyzed as a continuous variable. Left ventricular ejection fractions were divided into 3 categories (> 40%, ≤ 40%, or missing), as echocardiograms were not performed for patients with low cardiac risk and thus missing echocardiogram was not random. Model fit was assessed with the Hosmer-Lemeshow goodness-of-fit test. As there were only 137 patients with the outcome (postoperative AKI), it was not possible to include several possible confounders in the logistic regression analyses. To maximize the inclusion of possible confounders, the analyses were also performed using propensity score (PS). PS for diuretic and ACE-I/ARB use were derived from all the variables in Table 1. The use of ACE-I/ARB or diuretics was included in the model when generating PS for diuretics and ACE-I/ARB, respectively. The discrimination of the model was assessed using the c-statistic and receiver operating characteristic curve. We performed three different sensitivity analyses: PS adjustment, PS matching, and inverse probability weighting. For PS adjustment, PS quintiles were used rather than the logit of the PS as a continuous variable, because the association between PS and odds of postoperative AKI proved to be nonlinear (S1 Fig). The PS quintiles were treated as a categorical variable. PS matching was also performed. The users of ACE-I/ARB and diuretics were matched with non-users on the logit of PS (+/- 0.2 SD) (user: non-user = 1:2) by a greedy matching method. The odds of postoperative AKI in a propensity-matched cohort were examined using logistic regression analyses. Interaction terms were added to multivariable logistic regression analyses to determine whether the presence of CKD was an effect modifier of the association between diuretics, ACE-I/ARB use and AKI, and whether the use of ACE-I/ARB or the propensity for diuretic use was an effect modifier of the association between diuretic use and AKI. Values of p ≤ 0.05 were considered statistically significant except for interactions where p ≤ 0.10 was considered statistically significant [33, 34].
Table 1. Clinical characteristics of patients.
| No AKI (n = 2,588) | AKI (n = 137) | p | |
|---|---|---|---|
| Age | 63 (52–72) | 71 (61–76) | <0.001 |
| Male sex | 1281 (49.5) | 92 (67.2) | <0.001 |
| Intra-thoracic surgery Intra-abdominal surgery Surgery with large fluid shift Others | 478 (18.5) 1140 (44.0) 441 (17.0) 529 (20.5) | 36 (26.3) 79 (57.7) 16 (11.7) 6 (4.3) | <0.001 |
| Emergency surgery | 169 (6.5) | 23 (16.8) | <0.001 |
| eGFR (ml/min/1.73m2) | 77.7 (66.3–93.6) | 67.9 (53.7–85.5) | <0.001 |
| eGFR ≥ 60 30 ≤ eGFR < 60 15 ≤ eGFR < 30 eGFR < 15 | 2241 (86.6) 335 (12.9) 10 (0.4) 2 (0.1) | 88 (64.2) 42 (30.7) 6 (4.4) 1 (0.7) | |
| Body mass index | 22.0 (19.8–24.7) | 23.3 (21.0–25.4) | 0.003 |
| Smoking | 652 (25.2) | 28 (20.4) | 0.21 |
| Diabetes Mellitus | 392 (15.1) | 42 (30.7) | <0.001 |
| Insulin | 48 (1.9) | 11 (8.0) | <0.001 |
| Hypertension | 1030 (39.8) | 87 (63.5) | <0.001 |
| COPD | 203 (7.8) | 18 (13.1) | 0.027 |
| Atrial fibrillation | 67 (2.6) | 9 (6.6) | 0.006 |
| Peripheral arterial disease | 32 (1.2) | 1 (0.7) | 0.60 |
| Cerebrovascular disease | 91 (3.5) | 19 (13.9) | <0.001 |
| Coronary artery disease | 154 (6.0) | 16 (11.7) | 0.007 |
| Hematocrit (%) | 39.2 (35.8–42.2) | 37.7 (33.0–41.2) | 0.001 |
| INR > 1.5 | 14 (0.5) | 2 (1.5) | 0.17 |
| Platelet < 150,000/μl | 241 (9.3) | 24 (17.5) | 0.002 |
| Vasopressors | 1273 (49.2) | 97 (70.8) | <0.001 |
| Left ventricular ejection fraction >40% ≤40% missing | 1298 (50.2) 7 (0.3) 1283 (49.5) | 77 (56.2) 0 (0) 60 (43.8) | 0.33 |
| NSAIDs | 2318 (89.6) | 116 (84.7) | 0.071 |
| Contrast | 160 (6.2) | 16 (11.7) | 0.011 |
| Diuretics | 83 (3.2) | 16 (11.7) | <0.001 |
| ACE-I/ARB | 420 (16.2) | 40 (29.2) | <0.001 |
Data are shown as median (interquartile range) or number (%). P values were determined using the Mann-Whitney U test or Chi-square test. AKI: acute kidney injury, eGFR: estimated glomerular filtration rate, COPD: chronic obstructive pulmonary disease, INR: international normalized ratio of prothrombin time, NSAIDs: non-steroidal anti-inflammatory drugs, ACE-I: angiotensin-converting enzyme inhibitor, ARB: angiotensin receptor blocker
All analyses were performed using SPSS version 19.0 (SPSS Inc, Chicago, IL).
Ethics Statement
The study protocol and waiver of consents were approved by the Ethics Committee of Kyoto Katsura Hospital and the study was conducted in accordance with the Declaration of Helsinki.
Results
During the study period, 3,455 patients underwent non-cardiac surgeries under general anesthesia at Kyoto Katsura Hospital. Of these, the following 730 patients were excluded: 196 who underwent urological surgeries, 504 without available creatinine values within 1 week preoperatively and/or 48 hours postoperatively, 20 who had undergone dialysis preoperatively, and 10 who had incomplete data. Thus 2,725 patients were eligible for analyses.
One hundred thirty-seven patients (5.0%) developed AKI and 3 (0.1%) required renal replacement therapy. In-hospital mortality was 1.2% (33/2725) [0.8% (21/2588) for patients without AKI and 8.0% (11/137) for patients with AKI]. Patients’ clinical characteristics are shown in Table 1. Preoepratively, 396 patients (14.5%) had CKD stage 3 or more. Patients with AKI were significantly older, more likely to be males, more likely to have undergone intra-thoracic, intra-abdominal or emergency surgeries, and more likely to have significantly lower eGFR, higher BMI and more comobidities, preoperatively. Significantly more patients with AKI received vasopressors intraoperatively, iodinated contrast, diuretics or ACE-I/ARB pre- and/or intra-operatively. No patients skipped diuretics or ACE-I/ARB on the day of surgery. Twenty-two patients were given diuretics during surgery to maintain urine output. No patients received ACE-I/ARB only on the day of surgery.
Multivariable logistic regression analyses were performed using pre- and/or intra-operative use of diuretics and ACE-I/ARB as well as covariates selected by backward elimination using the likelihood ratio test. The p value by Hosmer-Lemeshow test was 0.51. Pre- and/or intra-operative use of diuretics, but not the use of ACE-I/ARB, was significantly associated with development of AKI (Table 2). Other covariates significantly associated with the development of AKI included male sex, intra-thoracic surgery, intra-abdominal surgery, surgery with large fluid shifts, emergency surgery, the presence of CKD, BMI, the use of insulin, hypertension, CVA, pre-operative hematocrit and intra-operative use of vasopressors. The association of pre- and/or intra-operative use of diuretics or ACE-I/ARB and postoperative AKI was not significantly modified by the presence of CKD stage 3 or more (eGFR < 60 ml/min/1.73 m2) (p for interaction [diuretic use * CKD] = 0.25 and p for interaction [ACE/ARB use * CKD] = 0.51).
Table 2. Multivariable logistic regression analysis.
| Odds ratio (95% CI) | p | |
|---|---|---|
| Diuretics | 2.07 (1.10–3.89) | 0.02 |
| ACE-I/ARB | 0.89 (0.56–1.42) | 0.63 |
| Age | 1.02 (1.00–1.03) | 0.10 |
| Male sex | 1.92 (1.26–2.92) | 0.002 |
| Intra-thoracic surgery Intra-abdominal surgery Surgery with large fluid shift Others | 8.16 (3.32–20.10) 3.61 (1.52–8.56) 3.66 (1.37–9.79) 1 (reference) | <0.001 0.004 0.01 |
| Chronic kidney disease* | 1.93 (1.28–2.93) | 0.002 |
| Emergency surgery | 2.57 (1.49–4.43) | 0.001 |
| Body mass index | 1.08 (1.03–1.14) | 0.003 |
| Insulin | 3.40 (1.57–7.36) | 0.002 |
| Hypertension | 1.84 (1.18–2.86) | 0.007 |
| Cerebrovascular disease | 2.25 (1.25–4.02) | 0.006 |
| Hematocrit (%) | 0.96 (0.92–0.99) | 0.02 |
| Vasopressors | 1.82 (1.21–2.73) | 0.004 |
ACE-I: angiotensin-converting enzyme inhibitor, ARB: angiotensin receptor blocker
*Chronic kidney disease was defined by estimated glomerular filtration rate < 60 ml/min/1.73m2.
PS for the use of diuretics and ACE-I/ARB were derived from all the variables in Table 1. C-statistics for diuretics and ACE-I/ARB were 0.86 and 0.75, respectively. Multivariable logistic regression analyses using PS quintiles and the use of diuretics and ACE-I/ARB showed that pre- and/or intra-operative use of diuretics, but not ACE-I/ARB, was significantly associated with the development of postoperative AKI (Table 3). P values by the Hosmer-Lemeshow test for diuretics and ACE-I/ARB were 0.95 and 0.86, respectively.
Table 3. Comparison of odds ratio of postoperative acute kidney injury estimated by different statistical analyses.
| Odds ratio (95% CI) | p | ||
|---|---|---|---|
| Diuretics | Multivariable logistic regression | 2.07 (1.10–3.89) | 0.02 |
| Adjustment for PS quintiles | 2.35 (1.30–4.24) | 0.005 | |
| PS matching | 2.36 (1.06–5.24) | 0.04 | |
| Inverse probability weighting | 2.97 (1.29–6.80) | 0.01 | |
| ACE-I/ARB | Multivariable logistic regression | 0.89 (0.56–1.42) | 0.63 |
| Adjustment for PS quintiles | 0.98 (0.63–1.53) | 0.92 | |
| PS matching | 0.75 (0.43–1.32) | 0.32 | |
| Inverse probability weighting | 1.25 (0.66–2.34) | 0.50 |
Propensity scores for diuretics and ACE-I/ARB were derived using all the variables in Table 1. PS: propensity score, ACE-I; angiotensin-converting enzyme inhibitor, ARB: angiotensin receptor blocker
PS matching yielded pairs of 94 diuretic users and 188 non-users, and 309 users of ACE-I/ARB and 618 non-users. Demographics of the propensity-matched patients were well-balanced (S1 and S2 Tables). In the propensity-matched cohort, pre-operative use of diuretics, but not the use of ACE-I/ARB, was significantly associated with post-operative AKI (Table 3). We failed to match about one-third of the patients receiving ACE-I/ARB because of a considerable difference in the distribution of PS between the users and non-users. Thus, inverse probability weighting was also performed as a sensitivity analysis. The results were similar to those of other analyses (Table 3). Excluding patients whose inverse-probability weight was < 1 percentile and > 99 percentile or excluding patients whose PS do not overlap among users and non-users of ACE-I/ARB or diuretics did not significantly change the results (S3 Table).
To examine whether propensity for diuretic use would affect the effect size of diuretic use, the associations of diuretic use and postoperative AKI were examined in each PS quintile for diuretic use. The use of diuretics was significantly associated with postoperative AKI in the first and second quintiles combined (the first and second quintiles were grouped as the number of outcomes in these quintiles were small) and in the third quintile of PS for diuretic use, but not in other quintiles (Fig 1) (p for interaction [PS quintiles * diuretic use] = 0.057 < 0.1). Thirty-nine patients used ACE-I/ARB and diuretics concomitantly. Pre- and/or intra-operative use of ACE-I/ARB was a significant effect modifier for the association between diuretics use and postoperative AKI (p for interaction [ACE-I/ARB*diuretics] = 0.007). The use of diuretics was significantly associated with postoperative AKI among non-users of ACE-I/ARB but not among users of ACE-I/ARB (Table 4).
Fig 1. Odds ratio of postoperative acute kidney injury in diuretic user in each quintile of propensity score for diuretic use.
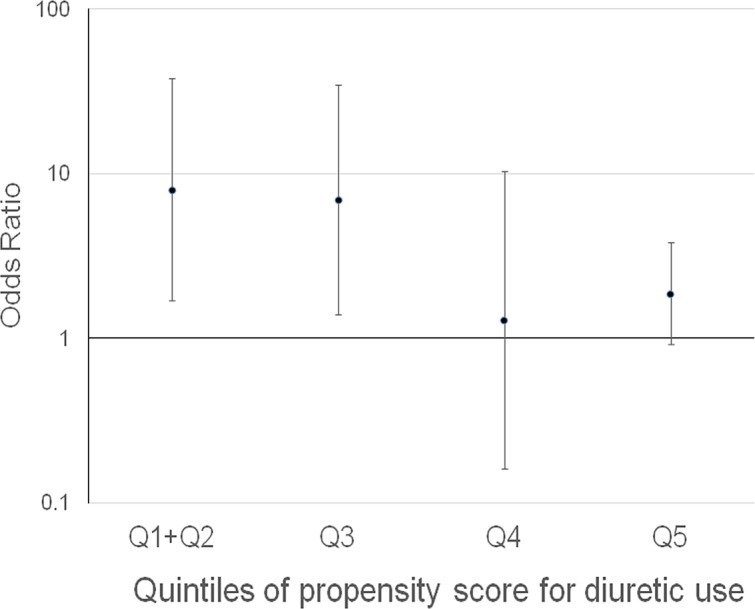
p for interaction [PS quintiles * diuretic use] = 0.057<0.1.
Table 4. Odds ratio of postoperative acute kidney injury in diuretic users stratified by the use of ACE-I/ARB.
| Odds ratio | 95% CI | p | |
|---|---|---|---|
| ACE-I/ARB (-) | 4.16 | 2.00–8.64 | <0.001 |
| ACE-I/ARB (+) | 0.44 | 0.12–1.61 | 0.22 |
ACE-I; angiotensin-converting enzyme inhibitor, ARB: angiotensin receptor blocker
P for interaction (ACE-I/ARB*diuretics) = 0.007
Among 99 diuretic users, 63 patients used loop diuretics, 23 used thiazides, 26 used potassium-sparing diuretics, and one used carperitide (the sum exceeds 99 as 13 received both a loop and a potassium-sparing diuretics and 1 received both a thiazide and a potassium-sparing diuretics). The odds ratios (95% CI) of postoperative AKI among users compared with non-users were 2.64 (1.28–5.43), 1.80 (0.50–6.48), and 1.33 (0.36–4.87) for loop diuretics, thiazides, and potassium-sparing diuretics, respectively.
Discussion
Diuretics, ACE-I and ARB can possibly increase the risk of postoperative AKI by their hemodynamic effect on kidneys. In this study, pre- and/or intra-operative use of diuretics, but not ACE-I/ARB, was significantly associated with the development of AKI after non-cardiac surgery. Diuretic use was significantly associated with postoperative AKI among patients with low propensity for diuretic use.
Several previous studies addressed whether diuretics, ACE-I or ARB were associated with AKI after cardiac surgery. Preoperative use of diuretics was not a significant predictor of AKI after cardiac surgery [15, 18, 19]. The association of preoperative ACE-I/ARB use and AKI after cardiac surgery has varied among studies, with results showing positive [17, 22], negative [19], and no association [6, 15, 16, 18]. The reasons for this discrepancy are not completely clear. The definitions of AKI were different (requirement of renal replacement therapy, RIFLE criteria or AKI network criteria). Previous studies showed that ACE-I was associated with decreased systemic vascular resistance and increased cardiac index and creatinine clearance after on-pump coronary artery bypass surgery in patients with left ventricular dysfunction (left ventricular ejection fraction < 40%) [35, 36]. Whether ACE-I or ARB increases or decreases the risk of postoperative AKI might be determined by the balance between their beneficial effects on cardiac function and their effects of decreasing glomerular filtration pressure via dilation of efferent arterioles. The surgical techniques used in these studies also differed (on-pump, off-pump or both). Cardiopulmonary bypass was shown to increase plasma renin activity [36] and thus the effects of ACE-I or ARB could differ between on- and off-pump cardiac surgery.
On the other hand, patients undergoing non-cardiac surgery are less likely to have left ventricular dysfunction than those undergoing cardiac surgery. We speculated that the hemodynamic effect of these agents on kidneys would predominate and that they would be independently associated with AKI after non-cardiac surgery. Pre- and/or intra-operative use of diuretics was significantly associated with postoperative AKI, but contrary to our hypothesis, the use of ACE-I/ARB was not. Our cohort included only 7 (0.3%) patients with left ventricular ejection fraction of 40% or less and 396 (14.5%) patients with eGFR less than 60 ml/min/1.73m2, both groups at high risk of developing AKI. As a result, the proportion of patients in this study who developed postoperative AKI was much lower (5.0%) than those in prior studies who underwent cardiac surgery (20–40%) [17, 18], despite the use of the same AKI network criteria for the definition of AKI. Patients in our cohort might have had sufficient renal reserve and thus the risk of developing postoperative AKI might not have been increased by the preoperative use of ACE-I/ARB. It is of note, however, that the use of diuretics was significantly associated with the development of postoperative AKI though patients in our study seemed to have renal reserve. During the postoperative period, fluids shift from the intravascular space to the third space and administration of diuretics may exacerbate the intravascular volume contraction. This may explain the significant increase in the risk of postoperative AKI observed in our study.
Our results differed from those of several previous studies focusing on non-cardiac surgery. The preoperative use of ACE-I/ARB was shown to be an independent predictor of postoperative AKI (defined by AKIN network criteria) in elective orthopedic surgery [26], lung resection surgery [28], and esophageal cancer surgery [30]. The sample sizes and number of outcomes (postoperative AKI) were smaller than in our study and logistic regression models were either overfitted [26] or insufficiently adjusted [28]. The study by Lee EH et al [30] was limited by a large percentage of patients with missing data (25–30%) and the use of multiple imputations, and preoperative chemotherapy might have contributed to postoperative AKI. In this study, we performed not only logistic regression analyses but also PS adjustment, PS matching, and inverse probability weighting to confirm the results and there were a very small number of patients with missing data. Shah M et al. showed that preoperative use of ACE-I/ARB was significantly associated with a lower incidence of postoperative AKI (defined by need for renal replacement therapy) [37] after major elective surgery. Their study included both patients undergoing cardiac and non-cardiac surgery and there was no subgroup analysis in the non-cardiac surgery cohort. They also showed that the presence of CKD was a significant effect modifier and that this association between ACE-I/ARB use and postoperative AKI was primarily evident in patients with CKD. In our study, the presence of CKD was not a significant effect modifier.
We found that diuretic use was significantly associated with postoperative AKI but only in patients with a low propensity for diuretic use (Fig 1). The preoperative use of ACE-I/ARB was also a significant effect modifier for the association between diuretic use and postoperative AKI. The use of diuretics was significantly associated with postoperative AKI only among non-users of ACE-I/ARB (Table 4). This is consistent with the fact that users of ACE-I/ARB are more likely to have heart failure, hypertension and CKD, which corresponds to patients with a high propensity for diuretic use. Patients with a high propensity for diuretic use, such as those with congestive heart failure and/or CKD, are at high risk of developing volume overload. It is suggested that elevated venous pressure is associated with worsening renal function, and animal studies demonstrated improvements in renal function after venous pressure was lowered [38–40]. Thus, in patients with high propensity for diuretic use, the benefit of avoiding volume overload might have offset the risk of volume contraction. On the other hand, in patients with a low propensity for diuretic use, such as those with essential hypertension or those who received diuretics only to maintain urine output, diuretics might have resulted in intravascular volume contraction and caused postoperative AKI.
Among the different classes of diuretics, only loop diuretics were significantly associated with postoperative AKI. This is likely because it is the most potent diuretic and it causes greater intravascular volume contraction than other agents [41]. However, it is possible that the observed difference was due to the lack of statistical power with thiazides or other agents, leading to low accuracy of parameter estimates.
The strength of our study is that our cohort included a large number of patients who underwent non-cardiac surgery at a community hospital and who were representatives of those being treated in a general medical practice setting. We selected as many potential predictors of post-operative AKI as possible based on previous studies [5–30], and the covariates used for multivariable logistic regression analyses and PS estimation were more complete than those in previous studies [5–30]. Multivariable logistic regression analyses, PS adjustment, PS matching, and inverse probability weighting yielded similar results. Our study also had several limitations. As this was an observational study, the possibility of unknown confounders cannot be excluded. The low incidence of dialysis requirement and in-hospital mortality precluded the analysis of associations between the use of diuretics or ACE-I/ARB and these outcomes. Also, the relatively small number of patients with CKD precluded subgroup analysis in these patients. PS was estimated using the demographics at the time of preoperative evaluation, not those at the time of drug initiation.
Conclusion
In our cohort with relatively preserved cardiac and renal function, pre- and/or intra-operative use of diuretics, but not ACE-I/ARB, was significantly associated with the development of AKI following non-cardiac surgery. The effect size of diuretics was greater in patients with low propensity for diuretic use. While the observational nature of our study did not establish causality and randomized controlled trials are warranted, it may be prudent to withhold diuretics preoperatively or to refrain from administering diuretics with the sole goal of maintain urine output in non-cardiac surgery, considering the minimal downsides of this approach in patients with preserved cardiac and renal function.
Supporting Information
In unadjusted model, only quintiles of PS were included as covariates. In adjusted model, the use of diuretics or ACE-I/ARB was also included as a covariate.
(TIF)
(DOCX)
(DOCX)
(DOCX)
Acknowledgments
Preliminary results of this study were presented in an abstract form at the American Society of Nephrology’s Renal Week in Denver, Colorado, from November 16–21, 2010, and at the American Society of Nephrology’s Kidney Week in Philadelphia, Pennsylvania, from November 8–13, 2011.
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
The authors have no support or funding to report.
References
- 1. Lassnigg A, Schmidlin D, Mouhieddine M, Bachmann LM, Druml W, Bauer P, et al. Minimal changes of serum creatinine predict prognosis in patients after cardiothoracic surgery: a prospective cohort study. J Am Soc Nephrol 2004; 15: 1597–1605. [DOI] [PubMed] [Google Scholar]
- 2. Brown JR, Cochran RP, Dacey LJ, Ross CS, Kunzelman KS, Dunton RF, et al. Perioperative increases in serum creatinine are predictive of increased 90 day mortality after coronary artery bypass graft surgery. Circulation 2006; 114 [Suppl 1]: I 409–413. [DOI] [PubMed] [Google Scholar]
- 3. Chertow GM, Levy EM, Hammermeister KE, Grover F, Daley J. Independent association between acute renal failure and mortality following cardiac surgery. Am J Med 1998; 104: 343–348. [DOI] [PubMed] [Google Scholar]
- 4. van Kuijk JP, Flu WJ, Chonchol M, Hoeks SE, Winkel TA, Verhagen HJ, et al. Temporary perioperative decline of renal function is an independent predictor for chronic kidney disease. Clin J Am Soc Nephrol 2010; 5: 1198–1204. 10.2215/CJN.00020110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Fortescue EB, Bates DW, Chertow GM. Predicting acute renal failure after coronary bypass surgery: cross-validation of two risk-stratification algorithms. Kidney Int 2000; 57: 2594–2602. [DOI] [PubMed] [Google Scholar]
- 6. Karkouti K, Wijeysundera DN, Yau TM, Callum JL, Cheng DC, Crowther M, et al. Acute kidney injury after cardiac surgery: focus on modifiable risk factors. Circulation 2009; 119: 495–502. 10.1161/CIRCULATIONAHA.108.786913 [DOI] [PubMed] [Google Scholar]
- 7. Conlon PJ, Stafford-Smith M, White WD, Newman MF, King S, Winn MP, et al. Acute renal failure following cardiac surgery. Nephrol Dial Transplant 1999; 14: 1158–1162. [DOI] [PubMed] [Google Scholar]
- 8. Mehta RH, Grab JD, O’Brien SM, Bridges CR, Gammie JS, Haan CK, et al. Bedside tool for predicting the risk of postoperative dialysis in patients undergoing cardiac surgery. Circulation 2006; 114: 2208–2216. [DOI] [PubMed] [Google Scholar]
- 9. Thakar CV, Arrigain S, Worley S, Yared JP, Paganini EP. A clinical score to predict acute renal failure after cardiac surgery. J Am Soc Nephrol 2005; 16: 162–168. [DOI] [PubMed] [Google Scholar]
- 10. Seabra VF, Alobaidi S, Balk EM, Poon AH, Jaber BL. Off-pump coronary artery bypass surgery and acute kidney injury: a meta-analysis of randomized controlled trials. Clin J Am Soc Nephrol 2010; 5: 1734–1744. 10.2215/CJN.02800310 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Thakar CV, Liangos O, Yared JP, Nelson DA, Hariachar S, Paganini EP. Predicting acute renal failure after cardiac surgery: validation and re-definition of a risk-stratification algorithm. Hemodial Int 2003; 7: 143–147. 10.1046/j.1492-7535.2003.00029.x [DOI] [PubMed] [Google Scholar]
- 12. Eriksen BO, Hoff KR, Solberg S. Prediction of acute renal failure after cardiac surgery: retrospective cross-validation of a clinical algorithm. Nephrol Dial Transplant 2003; 18: 77–81. [DOI] [PubMed] [Google Scholar]
- 13. Wijeysundera DN, Karkouti K, Dupuis JY, Rao V, Chan CT, Granton JT, et al. Derivation and validation of a simplified predictive index for renal replacement therapy after cardiac surgery. JAMA 2007; 297:1801–1809. [DOI] [PubMed] [Google Scholar]
- 14. Mangano CM, Diamondstone LS, Ramsay JG, Aggarwal A, Herskowitz A, Mangano DT. Renal dysfunction after myocardial revascularization: risk factors, adverse outcomes, and hospital resource utilization. The Multicenter Study of Perioperative Ischemia Research Group. Ann Intern Med 1998; 128:194–203. [DOI] [PubMed] [Google Scholar]
- 15. Provenche`re S, Plantefe`ve G, Hufnagel G, Vicaut E, De Vaumas C, Lecharny JB, et al. Renal dysfunction after cardiac surgery with normothermic cardiopulmonary bypass: incidence, risk factors, and effect on clinical outcome. Anesth Analg 2003; 96: 1258 –1264. [DOI] [PubMed] [Google Scholar]
- 16. Grayson AD, Khater M, Jackson M, Fox MA. Valvular heart operation is an independent risk factor for acute renal failure. Ann Thorac Surg 2003; 75:1829 –1835. [DOI] [PubMed] [Google Scholar]
- 17. Arora P, Rajagopalam S, Ranjan R, Kolli H, Singh M, Venuto R, et al. Preoperative use of angiotensin-converting enzyme inhibitors/angiotensin receptor blockers is associated with increased risk for acute kidney injury after cardiovascular surgery. Clin J Am Soc Nephrol 2008; 3: 1266–1273. 10.2215/CJN.05271107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Yoo YC, Youn YN, Shim JK, Kim JC, Kim NY, Kwak YL. Effects of renin-angiotensin system inhibitors on the occurrence of acute kidney injury following off-pump coronary artery bypass grafting. Circ J 2010; 74: 1852–1858. [DOI] [PubMed] [Google Scholar]
- 19. Benedetto U, Sciarretta S, Roscitano A, Fiorani B, Refice S, Angeloni E, et al. Preoperative angiotensin-converting enzyme inhibitors and acute kidney injury after coronary artery bypass grafting. Ann Thorac Surg 2008; 86: 1160–1165. 10.1016/j.athoracsur.2008.06.018 [DOI] [PubMed] [Google Scholar]
- 20. Parolari A, Pesce LL, Pacini D, Mazzanti V, Salis S, Sciacovelli C, et al. Risk factors for perioperative acute kidney injury after adult cardiac surgery: role of perioperative management. Ann Thorac Surg 2012; 93: 584–591. 10.1016/j.athoracsur.2011.09.073 [DOI] [PubMed] [Google Scholar]
- 21. Yacoub R, Patel N, Lohr JW, Rajagopalan S, Nader N, Arora P. Acute kidney injury and death associated with renin angiotensin system blockade in cardiothoracic surgery: a meta-analysis of observational studies. Am J Kidney Dis 2013; 62: 1077–1086. 10.1053/j.ajkd.2013.04.018 [DOI] [PubMed] [Google Scholar]
- 22. Coca SG, Garg AX, Swaminathan M, Garwood S, Hong K, Thiessen-Philbrook H, et al. Preoperative angiotensin-converting enzyme inhibitors and angiotensin receptor blocker use and acute kidney injury in patients undergoing cardiac surgery. Nephrol Dial Transplant 2013; 28: 2787–2799. 10.1093/ndt/gft405 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Kheterpal S, Tremper KK, Englesbe MJ, O’Reilly M, Shanks AM, Fetterman DM, et al. Predictors of postoperative acute renal failure after noncardiac surgery in patients with previously normal renal function. Anesthesiology 2007; 107:892–902. [DOI] [PubMed] [Google Scholar]
- 24. Abelha FJ, Botelho M, Fernandes V, Barros H. Determinants of postoperative acute kidney injury. Critical Care 2009; 13:R79 10.1186/cc7894 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Licker M, Cartier V, Robert J, Diaper J, Villiger Y, Tschopp JM, et al. Risk factors of acute kidney injury according to RIFLE criteria after lung cancer surgery. Ann Thorac Surg 2011; 91: 844–850. 10.1016/j.athoracsur.2010.10.037 [DOI] [PubMed] [Google Scholar]
- 26. Nielson E, Hennrikus E, Lehman E, Mets B. Angiotensin axis blockade, hypotension, and acute kidney injury in elective major orthopedic surgery. J Hosp Med 2014; 9: 283–288. 10.1002/jhm.2155 [DOI] [PubMed] [Google Scholar]
- 27. Ulucay C, Eren Z, Kaspar EC, Ozler T, Yuksel K, Kantarci G, et al. Risk factors for acute kidney injury after hip fracture surgery in the elderly individuals. Geriatr Orthop Surg Rehabil 2012; 3: 150–156. 10.1177/2151458512473827 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Ishikawa S, Griesdale DE, Lohser J. Acute kidney injury after lung resection surgery: incidence and perioperative risk factors. Anesth Analg 2012; 114: 1256–1262. 10.1213/ANE.0b013e31824e2d20 [DOI] [PubMed] [Google Scholar]
- 29.Teixeira C, Rosa R, Rodrigues N, Mendes I, Peixoto L, Dias S, et al. Acute kidney injury after major abdominal surgery: a retrospective cohort analysis. Crit Care Res Pract 10.1155/2014/132175, 2014 [DOI] [PMC free article] [PubMed]
- 30. Lee EH, Ryul Kim H, Baek SH, Kim KH, Chin JH, Choi DK, et al. Risk factors of postoperative acute kidney injury in patients undergoing esophageal cancer surgery. J Cardiothorac Vasc Anesth 2014; 28: 948–954. 10.1053/j.jvca.2013.12.006 [DOI] [PubMed] [Google Scholar]
- 31. Molitoris BA, Levin A, Warnock DG, Joannidis M, Mehta RL, Kellum JA, et al. Improving outcomes of acute kidney injury: report of an initiative. Nat Clin Pract Nephrol 2007; 3: 439–442. [DOI] [PubMed] [Google Scholar]
- 32. Matsuo S, Imai E, Horio M, Yasuda Y, Tomita K, Nitta K, et al. Revised equations for estimated GFR from serum creatinine in Japan. Am J Kidney Dis 2009; 53: 982–992. 10.1053/j.ajkd.2008.12.034 [DOI] [PubMed] [Google Scholar]
- 33. Duncan JL, Harrild KA, Iversen L, Lee AJ, Godden DJ. Long-term outcomes in men screened for abdominal aortic aneurysm: prospective cohort study. BMJ 2012; 344; e2958 10.1136/bmj.e2958 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Selvin S. Statistical Analysis of Epidemiologic Data. Oxford, United Kingdom: Oxford University Press; 2004. [Google Scholar]
- 35. Ryckwaert F, Colson P, Ribstein J, Boccara G, Guillon G. Haemodynamic and renal effects of intravenous enalaprilat during coronary artery bypass graft surgery in patients with ischaemic heart dysfunction. Br J Anaesth 2001; 86: 169–175. [DOI] [PubMed] [Google Scholar]
- 36. Wagner F, Yeter R, Bisson S, Siniawski H, Hetzer R. Beneficial hemodynamic and renal effects of intravenous enalaprilat following coronary artery bypass surgery complicated by left ventricular dysfunction. Crit Care Med 2003; 31: 1421–1428. [DOI] [PubMed] [Google Scholar]
- 37. Shah M, Jain AK, Brunelli SM, Coca SG, Devereaux PJ, James MT, et al. Association between angiotensin converting enzyme inhibitor or angiotensin receptor blocker use prior to major elective surgery and the risk of acute dialysis. BMC Nephrol 2014; 15: 53 10.1186/1471-2369-15-53 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Firth JD, Raine AR, Ledingham JG. Raised venous pressure: A direct cause of renal sodium retention in oedema? Lancet 1988; 1: 1033–1035. [DOI] [PubMed] [Google Scholar]
- 39. Winton FR. The influence of venous pressure on the isolated mammalian kidney. J Physiol 1931; 72: 49–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Anand IS. Cardiorenal syndrome: a cardiologist’s perspective of pathophysiology. Clin J Am Soc Nephrol 2013; 8: 1800–1807. 10.2215/CJN.04090413 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Puschett JB. Pharmacological classification and renal actions of diuretics. Cardiology. 1994;84 Suppl 2:4–13. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
In unadjusted model, only quintiles of PS were included as covariates. In adjusted model, the use of diuretics or ACE-I/ARB was also included as a covariate.
(TIF)
(DOCX)
(DOCX)
(DOCX)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.


