Abstract
Objective
The purpose of this investigation was to examine the economic impact of performing elective repeat cesarean during the 37th or 38th week of gestation relative to the ACOG recommendation of 39 week delivery.
Methods
Decision analysis modeling was used to estimate economic outcomes for a hypothetical cohort of neonates using data from the NICHD/MFMU study entitled “Timing of elective repeat cesarean delivery at term and neonatal outcomes.” Costs and charges were estimated using the Florida Healthcare Cost and Utilization Project.
Results
82,541 deliveries occurring between 37–39 complete weeks gestation were analyzed for the incidence of adverse outcomes and their hospital costs and charges. The model demonstrated increased costs through increasing adverse outcomes among elective repeat cesarean deliveries performed prior to 39 weeks gestation.
Conclusion
Our findings suggest that there are benefits to waiting until 39 weeks of gestation to perform an elective repeat cesarean delivery.
Keywords: cost effectiveness, adverse outcomes, economic, neonatal intensive care
Introduction
The number of births by cesarean section was 31.8% of all births in the United States as reported in 2007. This represents the eleventh consecutive year of increase in the cesarean birth rate. 1 It has been well characterized that infants who are delivered prior to 39 weeks gestation have increased rates of adverse outcomes that primarily result from respiratory complications and the need for prolonged hospitalization.2–10 As the cesarean delivery rate has increased by more than 50% from 1996 to 2006, there has been growing concerns over the impact of elective repeat cesarean delivery on neonatal health.1 This is especially concerning given the known increase in adverse outcomes for infants who undergo elective repeat cesarean delivery in the absence of labor prior to 39 weeks gestation.2, 5 However, the practice of elective repeat cesarean delivery prior to 39 weeks gestation remains common.3, 6 This was recently noted in an investigation of a cohort of patients who underwent repeat cesarean delivery within the nineteen centers of the Eunice Kennedy Shriver Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network (NICHD-MFMU). In this investigation that examined elective repeat cesarean delivery between 1999–2002 in these centers, 35.8% of these elective repeat cesarean deliveries were performed prior to 39 weeks completed gestation.6 Thus, the practice of elective repeat cesarean delivery remains common despite the American College of Obstetrics and Gynecology (ACOG) recommendation to await 39 weeks completed gestational age prior to elective repeat cesarean delivery.11 The purpose of this investigation was to utilize the rates of adverse outcome characterized in the NICHD-MFMU study of elective cesarean delivery at term to characterize the cost benefits of delay of elective repeat cesarean delivery to 39 weeks completed gestational age in a hypothetical cohort of neonates using decision tree analysis.
Methods
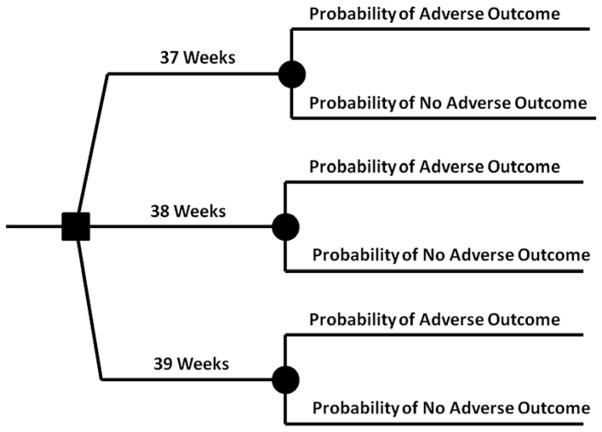
The Institutional Review Board at the Medical University of South Carolina (MUSC) approved this cost benefit economic investigation. This study utilized cost benefit modeling to integrate outcomes data with cost information by different gestational ages at time of elective repeat cesarean delivery. The goal of using this approach is to estimate the difference in cost expected in a population of neonates that underwent an elective repeat cesarean delivery at 37, 38, or 39 completed weeks of gestational age. In this investigation, the costs of care for infants delivered at either 37 or 38 weeks completed gestational age would be compared to those encountered at the ACOG recommended 39 completed weeks of gestational age.11 Adverse outcomes considered in this decision economic analysis included respiratory distress syndrome (RDS), transient tachypnea of the newborn (TTN), admission to the neonatal intensive care unit (NICU), neonatal sepsis, neonatal hypoglycemia, requirement for ventilation, and hospital stay of greater than or equal to 5 days. Proportions for each adverse outcome were derived from the prior patient cohort of elective cesarean delivery and are provided in Table 1.6 (Table 1) The incidence of these same outcomes were determined from the Florida 2007 discharge data from the Healthcare Cost and Utilization Project (HCUP) State Inpatient Database (SID). (Table 1) As each of these outcomes are not independent (i.e. a single live birth can experience multiple adverse outcome simultaneously), the cost benefit analysis was undertaken with the consideration of each adverse outcome independently. Data used in this investigation consisted of: (1) the incidence of adverse outcomes as reported in the NICHD-MFMU investigation of “Timing of Elective Repeat Cesarean Delivery at Term and Neonatal Outcomes” and (2) Neonatal discharge costs and data as derived from the 2007 discharge data from the Healthcare Cost and Utilization Project (HCUP) State Inpatient Database (SID) for Florida which was developed by the Agency for Healthcare Research and Quality.6, 12 The Florida HCUP-SID data comprises approximately 90% of inpatient discharge abstracts that include both clinical and non-clinical data from 269 of 294 (91.5%) hospitals across Florida. Costs were assessed from this database as the mean cost for healthcare of an infant in the hospitalization following delivery. The cost of a delivery that involved an adverse outcome of interest was assessed through the use of the International Statistical Classification of Diseases and Related Health Problems (ICD-9) coding that was delivered by repeat cesarean delivery between 37 to 39 weeks of completed gestational age (259 to 279 days from last menstrual period). As the HCUP records primary and secondary diagnosis at discharge, the ICD-9 code of interest had to be listed in either of these fields for the neonatal record to be included in the calculation of mean cost for the specific adverse outcome. Actual charges were used to estimate costs using a birth-specific set of cost-to-charge ratios developed from a proprietary data set for Florida that contained both cost and charges for each admission (Personal Communication with Dr. Kit Simpson, January, 2010). The effects of early delivery on charges were also reported because charges are a good estimator of differences in the medical care resources used for treating specific competing hospital conditions. Costs were adjusted for inflation to 2009 U.S. Dollars according to the 2007–2009 Hospital-related Services Consumer Price Index.13 The adverse outcomes that were analyzed in this manner included respiratory distress syndrome (ICD-9 code 769.0), transient tachypnea of the newborn (ICD-9 code 770.6), neonatal hypoglycemia (ICD-9 code 775.6), confirmed neonatal sepsis (ICD-9 code 771.81). The required admission to the NICU following birth was recorded in this database as was the need for early ventilator management (within 24 hours of delivery) allowing ascertainment of these complications. Births that were complicated by fetal anomalies or stillbirth were excluded from this costing data. In this manner, infant costs at discharge were obtained for infants that were discharged with these outcomes within the same gestational age strata (37–39 weeks gestational age) as were used in the NICHD-MFMU investigation of “Timing of Elective Repeat Cesarean Delivery at Term and Neonatal Outcomes” where adverse event incidence was derived.6 This allowed a representative (mean) cost to be assigned to each neonate that was discharged from the hospital with or without an adverse outcome following repeat cesarean delivery. In this investigation, costs and outcomes were calculated using a hypothetical cohort of 100 neonates delivered at each gestational age. Using a decision tree methodology, the total cost of care for each 100 neonate hypothetical cohort was calculated based upon the sum total cost of the anticipated incidence of the adverse event multiplied by 100 and then multiplied by the mean cost for that adverse outcome with the remainder of the neonates without the adverse event present multiplied by (1-the incidence of the adverse event rate) multiplied by the discharge mean cost for uncomplicated neonatal care. The decision analysis model utilized in this investigation was constructed in Microsoft Excel 2007 (Seattle, Washington) and is shown in Figure 1. (Figure 1)
Table 1.
Incidence of Adverse Neonatal Outcome Following Elective Repeat Cesarean Delivery by Completed Week of Gestation at Delivery
| NICHD-MFMU Data* Weeks Gestation (%)† |
Florida HCUP-SID Data‡ | |||
|---|---|---|---|---|
| Outcome | 37 Weeks Completed Gestation (6.3%) | 38 Weeks Completed Gestation (29.5%) | 39 Weeks Completed Gestation (49.1%) | 37–39 Weeks Completed Gestation |
| Respiratory Distress Syndrome (%) | 3.7 | 1.9 | 0.9 | 2.47 |
| Transient Tachypnea of the Newborn (%) | 4.8 | 3.9 | 2.7 | 4.75 |
| Admission to NICU (%) | 12.8 | 8.1 | 5.9 | NR |
| Newborn Sepsis (proved cases) (%) | 0.4 | 0.1 | 0.1 | 0.00 |
| Treated Hypoglycemia (%) | 2.4 | 0.9 | 0.7 | 1.97 |
| Ventilation Required in 1st 24 hours (%) | 1.9 | 0.9 | 0.4 | 0.19 |
| Hospital stay ≥ 5 days (%) | 9.1 | 5.7 | 3.6 | 4.37 |
FIGURE 1.
Decision tree model
In the decision tree model, first decision was to determine gestational age at delivery. At that point, cost was determined in a hypothetical cohort of 100 neonates delivered who experienced rate of adverse outcome per specific gestational age strata (ie, 37, 38, or 39 weeks of completed gestation).
Robinson. Timing of elective repeat cesarean delivery: a cost analysis. Am J Obstet Gynecol 2010.
Results
A total of 82,541 repeat cesarean deliveries occurred between 37 and 39 completed weeks gestation in the 2007 Florida HCUP SID database. Of these deliveries, there was a 0.26% incidence (n=214) of neonatal death. Costs and charges accrued at repeat cesarean delivery were obtained in U.S. dollars based on the 2007 Florida HCUP SID database and are reported as the mean costs and charges of neonatal discharge billing with either no adverse outcome (uncomplicated delivery) or with an adverse outcome affecting neonatal care in Table 2 (Table 2). Each of the adverse events examined in this investigation resulted in at least a five-fold increase in neonatal discharge costs, as evidenced by neonates affected by transient tachypnea of the newborn, when compared to a normal outcome after repeat cesarean delivery as experienced in the 37–39 week completed gestational age window. Costs at discharge were noted to rise as much as 152-fold over an uncomplicated neonate delivered by repeat cesarean delivery in the case of confirmed neonatal sepsis. These costs were used with the observed rates of adverse neonatal outcome reported in the NICHD-MFMU study of timing of elective cesarean delivery in the decision tree model to estimate the cost of delivery of 100 hypothetical neonates at each of 37, 38, and 39 weeks completed gestational age. In each of these cohorts, the contribution of each neonatal adverse event was found to be in excess of the cost of management of an uncomplicated neonatal delivery. It was noted that the excess costs of delivery at 37 or 38 weeks completed gestation compared to 39 weeks gestation were greater when repeat cesarean delivery occurred at 37 weeks rather than 38 weeks. (Table 3) Both of these cohorts (37 weeks and 38 weeks) had greater costs associated with elective cesarean delivery than those encountered at 39 weeks completed gestational age. Thus, this model is a dominant model where costs were always greater with delivery at earlier gestation than 39 completed weeks gestation. The cost savings associated with a delay of elective repeat cesarean delivery from 37 weeks or 38 weeks to 39 weeks gestation are reported in Table 4 for each 100 infant hypothetical cohort. (Table 4). It is noted that there is a cost savings for delaying delivery by either two weeks (37 weeks to 39 weeks) or by one week (38 weeks to 39 weeks). The costs were noted to decline the most when neonatal intensive care admission or respiratory distress syndrome was avoided through delay of elective cesarean delivery by either one or two weeks. However, there were also savings encountered with delay of elective repeat cesarean delivery in avoiding transient tachypnea of the newborn, proven newborn sepsis, and hypoglycemia that required treatment. Thus, with any of the adverse events analyzed, there was cost savings with each incremental week of delay of elective cesarean delivery from 37 to 39 completed weeks of gestational age.
Table 2.
Mean Cost and Mean Charges (per Delivery) Associated with Adverse Outcomes Following Cesarean Delivery at 37–39 Completed Weeks Gestation
| Mean Cost* (U.S. Dollars) | Increased Cost over Referent | Mean Charges* (U.S. Dollars) | Increased Charge over Referent | |
|---|---|---|---|---|
| No Adverse Event | $1,442 (800–1400) | Referent | $3,435 | Referent |
| Respiratory Distress Syndrome | $58,731 (5500–25,000) | 41 fold | $158,732 | 46 fold |
| Transient Tachypnea of the Newborn | $6,918 (2200–7400) | 5 fold | $18,206 | 5 fold |
| Admission to NICU | $24,391 (5700–12,000) | 17 fold | $35,368 | 10 fold |
| Newborn Sepsis (proved cases) | $219,386 (NA) | 152 fold | $535,089 | 156 fold |
| Treated Hypoglycemia | $24,221 (1500–10,000) | 17 fold | $63,741 | 19 fold |
| Ventilation Required in 1st 24 hours | $130,905 (35,000–50,000) | 91 fold | $385,014 | 112 fold |
| Hospital Length of Stay > 5 days | $23,433 | 16 fold | $55,794 | 16 fold |
NICU = Neonatal Intensive Care Unit
All costs/charges adjusted for inflation to 2009 U.S. Dollars according to the 2007–2009 Hospital-related Services Consumer Price Index reported as mean (Q1–Q3)
N/A = There were only 4 cases of confirmed sepsis in the 2007 Florida HCUP-SID Database
Table 3.
Cost and Charges per 100 Neonates Delivered by Elective Repeat Cesarean at 37, 38, and 39 Completed Weeks Gestation According to Adverse Outcome Incidence
| 37 Weeks Completed Gestation | 38 Weeks Completed Gestation | 39 Weeks Completed Gestation | ||||
|---|---|---|---|---|---|---|
| Adverse Outcome | Cost* (per 100 neonates) | Charge* (per 100 neonates) | Cost* (per 100 neonates) | Charge* (per 100 neonates) | Cost* (per 100 neonates) | Charge* (per 100 neonates) |
| Respiratory Distress Syndrome | $356,209 | $918,141 | $253,089 | $638,607 | $195,800 | $483,310 |
| Transient Tachypnea of the Newborn | $170,524 | $414,443 | $165,596 | $401,149 | $159,025 | $383,424 |
| Admission to NICU | $437,988 | $752,275 | $330,128 | $602,194 | $279,640 | $531,943 |
| Newborn Sepsis (proved cases) | $231,418 | $556,204 | $166,035 | $396,708 | $166,035 | $396,708 |
| Treated Hypoglycemia | $198,910 | $488,275 | $164,742 | $397,817 | $160,186 | $385,756 |
| Ventilation Required in 1st 24 hours | $390,220 | $1,068,542 | $260,757 | $686,964 | $196,026 | $496,174 |
| Hospital Stay > 5 days | $344,357 | $820,010 | $269,588 | $641,989 | $223,407 | $532,035 |
All costs/charges adjusted for inflation to 2009 U.S. Dollars according to the 2007–2009 Hospital-related Services Consumer Price Index
NICU – Neonatal Intensive Care Unit
Table 4.
Cost and Charge Savings per 100 Neonates Delivered by Elective Repeat Cearean at 39 Weeks Verses 100 Neonates Delivered at 37 or 38 Weeks Gestational Age
| Savings for 100 neonates delivered at 39 weeks rather than 37 weeks | Savings for 100 neonates delivered at 39 weeks rather than 38 weeks | |||
|---|---|---|---|---|
| Adverse Event | Cost Savings* | Charge Savings* | Cost Savings* | Charge Savings* |
| No Adverse Event | Referent | Referent | Referent | Referent |
| Respiratory Distress Syndrome | $160,408 | $434,831 | $57,289 | $155,297 |
| Transient Tachypnea of the Newborn | $11,499 | $31,019 | $6,571 | $17,725 |
| Admission to NICU | $158,348 | $220,332 | $50,488 | $70,251 |
| Newborn Sepsis (proved cases) | $65,383 | $159,496 | None | None |
| Treated Hypoglycemia | $38,724 | $102,519 | $4,556 | $12,061 |
| Ventilation Required in 1st 24 hours | $194,194 | $572,368 | $64,731 | $190,789 |
| Hospital Length of Stay > 5 days | $120,949 | $287,975 | $46,181 | $109,954 |
All costs/charges adjusted for inflation to 2009 U.S. Dollars according to the 2007–2009 Hospital-related Services Consumer Price Index
NICU = Neonatal Intensive Care Unit
Comment
Approximately 4.3 million births occurred in the United States in 2007, the same year as costs were assessed in this study. Of these births, 1.34 million of these deliveries were accomplished through cesarean delivery.1 Given that almost one third of pregnancies are completed by cesarean delivery, the optimal timing for repeat elective cesarean delivery is an important decision in improving neonatal outcome and controlling healthcare costs. Based upon this investigation, the delay of elective repeat cesarean section to 39 weeks completed gestational age was associated with significant cost savings in terms of neonatal management. This cost savings was anticipated due to a prior prospective observational cohort examining neonatal outcomes of elective repeat cesarean deliveries that occurred in the nineteen U.S. academic centers of the NICHD-MFMU which found decreasing incidence of the adverse outcomes examined in this investigation with delay of elective repeat cesarean delivery beyond 39 weeks completed gestational age. In this prior investigation, the authors concluded that elective repeat cesarean delivery prior to 39 weeks completed gestation was associated with a “preventable increase in neonatal morbidity and admissions to the NICU which carry a high economic cost.” 6 In this investigation, we sought to define the cost of elective repeat cesarean delivery at 37 and 38 weeks completed gestation relative to those completed at 39 weeks gestational age. While our study has limitations, it is able to assign a reasonable economic cost in terms of neonatal discharge expenditures using a large state database of neonatal discharge data.12 In order to demonstrate the similarity of outcomes in this state database to the neonatal outcomes of the large cohort reported by the NICHD-MFMU, the Florida HCUP-SID was examined for the incidence of these same outcomes in the 37–39 week completed gestational age window. Both reports were similar for the neonatal outcomes of interest. Thus, it appears that those outcomes seen in the NICHD-MFMU cohort investigation were representative of those in the Florida neonatal population in 2007. By selecting the mean discharge cost for neonates who experienced an adverse outcome, the cost data is more likely to represent the actual economic impact to the healthcare system that would be used in state budgeting. In using a large database from a state with a large birth population, our cost estimates are likely more representative of those seen in hospital based management in other areas of the United States. The cost estimates that were derived from the State of Florida HCUP database are striking in that any adverse neonatal outcome resulted in at least a five-fold increase in the discharge cost for a neonate delivered at 37–39 weeks gestation by repeat cesarean delivery. However, if any neonate required respiratory ventilation, sepsis management, or a NICU admission, these costs increased more than fortyfold. Thus, the cost associated with the management of a newborn with any adverse outcome was greatly increased over those without complicated neonatal admissions. Given the increased incidence of adverse outcomes encountered at 37 or 38 completed weeks gestation relative to 39 weeks completed gestation, it was anticipated that a significant increase in costs would be noted among neonates delivered prior to 39 completed weeks gestational age. In this investigation, the hypothetical cohort of 100 neonates illustrated the significant increased cost associated with the decision to proceed with elective repeat cesarean delivery at either 37 or 38 weeks completed gestational age rather than awaiting the ACOG goal of 39 weeks gestation. It is important to recognize that this analysis is based on elective repeat cesarean delivery and not those cases where an indication for repeat cesarean delivery is indicated in order to reduce fetal morbidity or mortality. However, it is apparent that a delay of two or one week to achieve 39 weeks completed gestation is associated with a reduction in costs for neonatal management during the birth admission. Thus, adhering to the recommendations of ACOG and awaiting 39 weeks gestational age prior to elective repeat cesarean delivery would be anticipated to reduce costs based on the cost analysis of the hypothetical cohort presented in this investigation.
Our study also has limitations that should be noted. First, this investigation was limited to an examination of the neonatal hospitalization costs and did not examine other costs (maternal, non-healthcare related, social) that would also be important in the decision of timing of repeat cesarean. Some potential risks that are inherent in delay of elective repeat cesarean would include stillbirth or uterine rupture. In the Florida HCUP-SID data there were ninety nine cases of stillbirth (0.12%) documented with 214 (0.26%) incidence of neonatal death.12 If earlier cesarean delivery could prevent these outcomes, the cost benefit would shift to earlier intervention. When considering the risk for antepartum uterine rupture, a prior large, population based cohort of women who selected to undergo elective repeat cesarean delivery at term found a risk of uterine rupture of 0.05% (11/23,794).14 Thus, the risk for stillbirth or uterine rupture is far less common than the neonatal complications examined by this study. However, when stillbirth or uterine rupture occur, the associated costs would far exceed those seen in the neonate delivered at 37 or 38 weeks gestation.
There are also ascertainment problems with the use of ICD-9 codes to identify a clinical condition. As personnel who code neonatal discharge charts are motivated to capture all billable diagnoses, there may be an assignment of adverse outcome by ICD-9 coding that may not be as clinically apparent. Thus, the ICD-9 code does not take into consideration the severity of the adverse outcome encountered which may affect other aspects of neonatal care and discharge cost depending on severity of the clinical condition. In order to best estimate the economic impact of timing of elective repeat cesarean, we selected the mean cost for the adverse outcome of interest in each case. Another potential limitation of this investigation is the use of a single state neonatal discharge database for assignment of cost to adverse outcomes. As Florida is designated a “Red Alert” state by the American College of Obstetricians and Gynecologists due to its high risk climate for medical-legal action, it is plausible that physicians may practice differently in the management of neonates who experience complications after birth than in other states where measures are in place to control medical-legal exposure in patient care.15 Finally, this study does not control for the variations among states in the rate of potential interactions between some of the adverse outcomes that were analyzed. The results of this economic investigation classify the individual adverse outcomes by the most costly event reported for that admission. Thus, the cost-weight used in the model could be affected by differences in the rates of combinations of adverse events that could differ geographically due to differences in patient risk, compositions, and local practice patterns. Thus, the combinations of events reflect Florida rates of combinations of outcomes that are not mutually independent as in the case of ventilator management and NICU admission which often occur concurrently. This limitation may not have a large effect on our findings because this economic investigation seeks to examine how more common complications after elective repeat cesarean delivery (i.e. hypoglycemia) can affect the cost significantly in only a small hypothetical cohort (n=100) of neonates.
In conclusion, our investigation demonstrates significant increased neonatal hospitalization cost associated with the elective repeat cesarean delivery when accomplished at 37 or 38 weeks gestation relative to 39 weeks gestation. Further studies of the timing of the elective repeat cesarean delivery are necessary to characterize the economic burden and quality of life issues surrounding delivery prior to 39 weeks completed gestation. However, neonatal hospitalization costs may be contained through careful consideration of timing of delivery in patients undergoing elective repeat cesarean delivery.
Acknowledgments
Financial Support: Clinical and Translational Science K12 Award, Medical University of South Carolina
Footnotes
Presented at the South Atlantic Association of Obstetricians and Gynecologists, Naples, Florida; January 2010.
Institutional Review Board Approval NHR#321
Reprints not available
References
- 1.Hamilton BE, Martin JA, Ventura SJ. National vital statistics reports, Web release. Vol. 57. Hyattsville, MD: National Center for Health Statistics; 2009. Births: Preliminary data for 2007. National vital statistics reports, Web release. [Google Scholar]
- 2.Hansen AK, Wisborg K, Uldbjerg N, Henriksen TB. Risk of respiratory morbidity in term infants delivered by elective caesarean section: cohort study. BMJ. 2008 Jan 12;336(7635):85–87. doi: 10.1136/bmj.39405.539282.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Laye MR, Dellinger EH. Timing of scheduled cesarean delivery in patients on a teaching versus private service: adherence to American College of Obstetricians and Gynecologists guidelines and neonatal outcomes. Am J Obstet Gynecol. 2006;195(2):577–582. doi: 10.1016/j.ajog.2006.03.078. [DOI] [PubMed] [Google Scholar]
- 4.Morrison JJ, Rennie JM, Milton PJ. Neonatal respiratory morbidity and mode of delivery at term: influence of timing of elective caesarean section. Br J Obstet Gynaecol. 1995;102(2):101–106. doi: 10.1111/j.1471-0528.1995.tb09060.x. [DOI] [PubMed] [Google Scholar]
- 5.Riskin A, Abend-Weinger M, Riskin-Mashiah S, Kugelman A, Bader D. Cesarean section, gestational age, and transient tachypnea of the newborn: timing is the key. Am J Perinatol. 2005;22(7):377–382. doi: 10.1055/s-2005-872594. [DOI] [PubMed] [Google Scholar]
- 6.Tita AT, Landon MB, Spong CY, et al. Timing of elective repeat cesarean delivery at term and neonatal outcomes. N Engl J Med. 2009;360(2):111–120. doi: 10.1056/NEJMoa0803267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zanardo V, Simbi AK, Franzoi M, Solda G, Salvadori A, Trevisanuto D. Neonatal respiratory morbidity risk and mode of delivery at term: influence of timing of elective caesarean delivery. Acta Paediatr. 2004;93(5):643–647. doi: 10.1111/j.1651-2227.2004.tb02990.x. [DOI] [PubMed] [Google Scholar]
- 8.Abouzeid H, Aggarwal D, De Graaf F. Timing of planned repeated caesarean section: an enigma. J Obstet Gynaecol. 2007;27(8):798–801. doi: 10.1080/01443610701666843. [DOI] [PubMed] [Google Scholar]
- 9.Schreiner RL, Stevens DC, Smith WL, Lemons JA, Golichowski AM, Padilla LM. Respiratory distress following elective repeat cesarean section. Am J Obstet Gynecol. 1982;143(6):689–692. doi: 10.1016/0002-9378(82)90116-8. [DOI] [PubMed] [Google Scholar]
- 10.Bowers SK, MacDonald HM, Shapiro ED. Prevention of iatrogenic neonatal respiratory distress syndrome: elective repeat cesarean section and spontaneous labor. Am J Obstet Gynecol. 1982;143(2):186–189. doi: 10.1016/0002-9378(82)90653-6. [DOI] [PubMed] [Google Scholar]
- 11.ACOG educational bulletin. . Assessment of fetal lung maturity. Number 230, November 1996. Committee on Educational Bulletins of the American College of Obstetricians and Gynecologists. Int J Gynaecol Obstet. 1997;56(2):191–198. [PubMed] [Google Scholar]
- 12.HCUP State Inpatient Databases (SID) Healthcare Cost and Utilization Project. Agency for Health Care Research and Quality; 2007. ( http://www.hcup-us.ahrq.gov/sidoverview.jsp). http://www.hcup-us.ahrq.gov/db/state/siddist/Introduction_to_SID.pdf. Updated 2006. [Google Scholar]
- 13.U.S. Bureau of Labor Statistics. Division of Consumer Prices and Price Indexes. [Accessed January 31, 2010];Consumer Price Index. www.bls.gov/cpi/home.htm.
- 14.Spong CY, Landon MB, Gilbert S, et al. Risk of uterine rupture and adverse perinatal outcome at term after cesarean delivery. Obstet Gynecol. 2007;110(4):801–807. doi: 10.1097/01.AOG.0000284622.71222.b2. [DOI] [PubMed] [Google Scholar]
- 15.Robinson P, Xu X, Keeton K, Fenner D, Johnson TR, Ransom S. The impact of medical legal risk on obstetrician-gynecologist supply. Obstet Gynecol. 2005;105(6):1296–1302. doi: 10.1097/01.AOG.0000157468.12907.1a. [DOI] [PubMed] [Google Scholar]