Abstract
Coccidioides, a dimorphic fungus endemic within the Americas, primarily causes pulmonary disease but may disseminate. We describe a case of confirmed Coccidioides endocarditis, the seventh reported in literature. Coccidioides endocarditis often requires tissue diagnosis and combined surgical and medical treatment.
Keywords: Coccidioides, endocarditis, posaconazole
CASE PRESENTATION
A 34-year-old Hispanic woman living in Bakersfield, California with a history of disseminated coccidioidomycosis presented in early 2013 with vaginal bleeding due to spontaneous abortion. She underwent dilation and curettage for retained placenta, received blood transfusions and fluid resuscitation for postoperative bleeding, but then developed acute dyspnea. Exam revealed a grade 3 diastolic murmur, chest radiography showed pulmonary edema and pleural effusions, and laboratory results included elevated brain natriuretic peptide and chronically elevated liver function tests attributed to Coccidioides granulomatous hepatitis. Transthoracic echocardiography (TTE) and transesophageal echocardiography (TEE) revealed severe aortic insufficiency and no vegetation. She improved with diuresis and was discharged on posaconazole with Coccidioides complement fixation (CF) titer of 1:4.
Medical history included pulmonary coccidioidomycosis in 2004 when the patient presented during her first pregnancy with fever, cough, and a pulmonary infiltrate. Amphotericin B was initiated but discontinued due to acute shortness of breath during infusion. She received fluconazole for 6 weeks. This pregnancy terminated in a spontaneous abortion. In 2007, the patient presented during her second pregnancy with coccidioidomycosis relapse involving the lungs and liver. She started posaconazole but discontinued it due to cost. She delivered a healthy baby with no evidence of Coccidioides transmission. The patient did not follow-up until her third pregnancy in 2010. She restarted posaconazole but had intermittent adherence. This pregnancy resulted in a live healthy birth.
Two months after early 2013 hospitalization, the patient was readmitted with congestive heart failure. Aortic valve replacement was attempted but aborted due to significant mediastinal fibrosis. The patient was transferred to another hospital where 4 sets of routine blood cultures were negative, TEE showed aortic regurgitation and no vegetation, and chest computed tomography revealed a 3.5 by 2.0 cm mediastinal mass with paratracheal and periaortic adenopathy (Figure 1).
Figure 1.
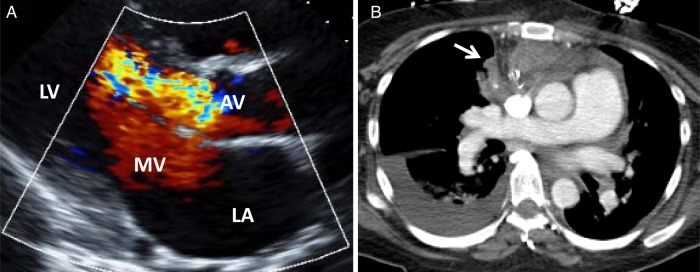
(A) Echocardiography demonstrating severe aortic regurgitation. (B) Chest computed tomography demonstrating anterior mediastinal mass (arrow) and right pleural effusion. Abbreviations: AV, aortic valve; LA, left atrium; LV, left ventricle; MV, mitral valve.
Aortic valve replacement was successfully accomplished. Histology showed granulomatous inflammation, multinucleation, and endosporulating spherules consistent with Coccidioides (Figure 2). Culture grew 1 fungal colony identified by DNA probe as Coccidioides spp. Coccidioides complement fixation titers were 1:8 before surgery and 1:2 after surgery plus 7 months of posaconazole therapy. The patient continues to receive posaconazole, which will be continued indefinitely with monitoring of symptoms, CF titers, and posaconazole levels every 3 months.
Figure 2.
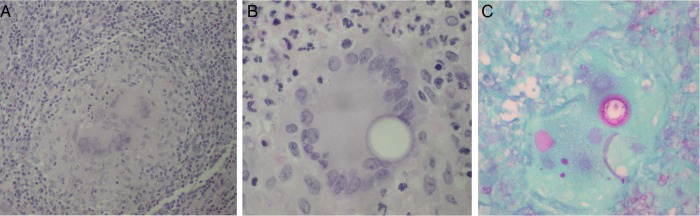
Pathology of periaortic and valvular tissue: (A) granulomatous inflammation by hematoxylin and eosin (H&E) stain, (B) multinucleation and Coccidioides spherule by H&E stain, and (C) endosporulating Coccidioides by Periodic acid-Schiff stain.
DISCUSSION
Coccidioides is a dimorphic fungus endemic to the Americas and comprises 2 species, Coccidioides immitis and Coccidioides posadasii, although they are nearly indistinguishable by laboratory tests [1, 2]. Approximately 40% of cases have self-resolving flu-like symptoms with clinically evident pneumonia, although 5% develop pulmonary nodules or cavities [3]. Dissemination can occur to skin, bone, joints, and meninges [3]. Cardiac involvement is uncommon and can affect the pericardium, but endocarditis is extraordinarily rare even with documented fungemia [1–6]. Our literature review identified 6 case reports and 1 conference abstract of Coccidioides endocarditis that met modified Duke′s criteria for definite or possible endocarditis (Table 1) [7–11]. Other reports lack clinical or histopathological confirmation of endocarditis [5, 8].
Table 1.
Seven Cases of Coccidioides Endocarditis
| Age | Sex | Ethnicity | Cardiac Pathology | Echo | Blood Cultures | CF Titers | Treatment | Outcome | Ref. |
|---|---|---|---|---|---|---|---|---|---|
| 34 yr | F | Hispanic | Mediastinal mass; aortic valve | No veg | Neg | 1:8 | Surgery + Posaconazole | Survived | Current |
| 10 yr | M | Hispanic | Right atrial mass; tricuspid valve veg | +mass | n/a | 1:2048 | Surgery + Amphotericin + Fluconazole | Survived | [7] |
| 3 wk | F | White | Mitral and tricuspid valve veg | +veg | Neg | 1:1 | No antifungals | Died | [8] |
| 21 yr | M | Black | Mitral valve abscess; myocarditis | n/a | positive | n/a | No antifungals | Died | [9] |
| 37 yr | M | White | Mitral valve veg | +veg | Neg | 1:256 | Amphotericin | Died | [8] |
| 53 yr | M | Hispanic | Prosthetic aortic valve veg | +veg | Neg | 1:32 | Surgery + Amphotericin + Fluconazole | Survived | [8] |
| 40 yr | M | White | Mitral, aortic, tricuspid, and pulmonic valve veg | +veg | Neg | 1:2 | Amphotericin + Fluconazole | Died | [8] |
Abbreviations: CF, serum Coccidioides complement fixation; F, female; M, male; n/a, not available; neg, negative; Ref, References; veg, vegetation(s).
Diagnosing Coccidioides endocarditis can be difficult: our patient′s routine blood cultures were repeatedly negative, and TTE and TEE showed no vegetation. Among prior cases, 2 had positive blood cultures, 5 had vegetations, 1 had an atrial mass, 1 had a valvular abscess, and CF titers ranged from 1:1 to 1:2048 [7–10]. Reliable diagnostics were culture and histopathology of surgically excised valvular tissue.
Prognosis depends on combined surgical and medical treatment. Our patient and 2 prior cases survived with surgery and antifungals [7–9]. Our patient is the only adult female among these cases and had pregnancies during infection and treatment. Coccidioides can cause aggressive disease during pregnancy with resultant maternal and fetal mortality [1]. Recommendations are to initiate azoles unless with rapidly progressive infection or pregnancy, in which case amphotericin B is recommended [2]. Fluconazole and, less often, itraconazole are often first-line antifungals in coccidioidomycosis, but studies show that posaconazole has over 70% success treating severe infections that are refractory to other antifungals [12, 13]. Our patient did not tolerate amphotericin and relapsed after fluconazole administration.
Evidence on azole safety in pregnancy is conflicting. Studies show that single, low-dose fluconazole is safe, but higher doses are linked with teratogenicity in animals and possibly with tetralogy of Fallot in humans [14, 15]. A systematic review concluded the following: low-dose fluconazole is safe after first trimester, itraconazole and voriconazole should be avoided, and isavuconazole and posaconazole lack conclusive human data [15]. Posaconazole is US Food and Drug Administration-labeled category C [15]. It is difficult to speculate about effects of posaconazole versus Coccidioides itself on our patient′s pregnancies [1].
CONCLUSIONS
In conclusion, Coccidioides rarely causes endocarditis, vegetations may not be detected by echocardiography, and a successful outcome can be achieved with combined surgical and medical management.
Acknowledgments
We thank the staff at Sequoia Hospital and Kern Medical Center for help with care of the patient.
Financial support. This work was supported by the National Institute of Allergy and Infectious Diseases at the National Institutes of Health (grant number 5T32AI052073-09).
Potential conflicts of interest. All authors: No reported conflicts.
All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest.
References
- 1.Stevens DA. Coccidioidomycosis. N Engl J Med 1995; 332:1077–82. [DOI] [PubMed] [Google Scholar]
- 2.Galgiani JN, Ampel NM, Blair JE et al. . Coccidioidomycosis. Clin Infect Dis 2005; 41:1217–23. [DOI] [PubMed] [Google Scholar]
- 3.Mirels L, Deresinski S. Coccidioidomycosis. In: Clinical Infectious Disease. Cambridge University Press, 2008; 1141–1150. [Google Scholar]
- 4.Forbus WD, Bestebreurtje AM. Coccidioidomycosis; a study of 95 cases of the disseminated type with special reference to the pathogenesis of the disease. Mil Surg 1946; 99:653–719. [PubMed] [Google Scholar]
- 5.Evans N, Ball HA. Coccidioidal granuloma analysis of fifty cases. JAMA 1929; 93:1881–5. [Google Scholar]
- 6.Keckich DW, Blair JE, Vikram HR. Coccidioides fungemia in six patients, with a review of the literature. Mycopathologia 2010; 170:107–15. [DOI] [PubMed] [Google Scholar]
- 7.La Via WV, Koulouri S, Ross LA et al. . Right atrial mass in a child with disseminated coccidioidomycosis. Pediatr Infect Dis J 2005; 24:470–2. [DOI] [PubMed] [Google Scholar]
- 8.Reuss CS, Hall MC, Blair JE et al. . Endocarditis caused by Coccidioides species. Mayo Clin Proc 2004; 79:1451–4. [DOI] [PubMed] [Google Scholar]
- 9.Merchant RK, Louria DB, Geisler PH et al. . Fungal endocarditis: review of the literature and report of three cases. Ann Intern Med 1958; 48:242–66. [DOI] [PubMed] [Google Scholar]
- 10.Dopf M, Reed W. Coccidioides endocarditis presenting as hand abscess. Presented at American College of Physicians; Reno, Nevada; 2008. Available at: http://www.pdfio.net/k-57414050.html. Accessed 1 October 2014.
- 11.Arsura EL, Bobba RK, Reddy CM. Coccidioidal pericarditis: a case presentation and review of the literature. Int J Infect Dis 2005; 9:104–9. [DOI] [PubMed] [Google Scholar]
- 12.Kim MM, Vikram HR, Kusne S et al. . Treatment of refractory coccidioidomycosis with voriconazole or posaconazole. Clin Infect Dis 2011; 53:1060–6. [DOI] [PubMed] [Google Scholar]
- 13.Stevens DA, Rendon A, Gaona-Flores V et al. . Posaconazole therapy for chronic refractory coccidioidomycosis. Chest 2007; 132:952–8. [DOI] [PubMed] [Google Scholar]
- 14.Mølgaard-Nielsen D, Pasternak B, Hviid A. Use of oral fluconazole during pregnancy and the risk of birth defects. N Engl J Med 2013; 369:830–9. [DOI] [PubMed] [Google Scholar]
- 15.Pilmis B, Jullien V, Sobel J et al. . Antifungal drugs during pregnancy: an updated review. J Antimicrob Chemother 2015; 70:14–22. [DOI] [PubMed] [Google Scholar]


