Abstract
Background
Diagnostic methods for pulmonary tuberculosis (TB) have recently advanced. The aim of this study was to evaluate the changes in TB diagnostic tests that prompted the initiation of anti-TB treatment over time in South Korea, an industrialized country with an intermediate TB burden.
Methods
Patients diagnosed with pulmonary TB in the first halves of 2005 and 2013 at a tertiary referral hospital were included. Diagnostic methods that prompted the initiation of anti-TB treatment were compared between the 2 groups of patients.
Results
A greater proportion of patients were diagnosed with pulmonary TB using bronchoscopy in 2013 than in 2005 (26.7% vs. 6.6%, respectively; p<0.001), while the proportion of patients clinically diagnosed with pulmonary TB was lower in 2013 than in 2005 (24.7% vs. 49.0%, respectively; p<0.001). Additionally, more patients started anti-TB treatment based on positive polymerase chain reaction (PCR) results for Mycobacterium tuberculosis DNA in 2013 than in 2005 (47.3% vs. 7.9%, respectively; p<0.001).
Conclusion
The initiation of treatment for pulmonary TB in South Korea has become more frequently based on PCR and the use of bronchoscopic specimens.
Keywords: Tuberculosis, Pulmonary; Diagnosis; Bronchoscopy; Nucleic Acid Amplification Techniques
Introduction
The worldwide disease burden of tuberculosis (TB) is considerable, with newly reported cases in 2012 estimated at 8.6 million1. The incidence, prevalence and mortality rates of TB in South Korea are the highest of all Organization for Economic Co-operation and Development (OECD) nations2 with 36,089 patients (71.4 per 100,000 population) in 20133. Early and accurate detection of pulmonary TB is important for the timely initiation of treatment, and prevention of TB transmission4. Diagnostic methods for pulmonary TB have evolved over time, commensurate with the increasing availability of molecular diagnostic methods, as well as the introduction of procedures such as bronchoscopy.
Acid-fast staining, of sputum in patients with suspected pulmonary TB, confers cost and processing time benefits, but has low diagnostic sensitivity and specificity5. Mycobacterial culture on solid medium has good sensitivity and specificity, but is not facilitative for early diagnosis due to its protracted processing time6. To overcome the disadvantages of traditional diagnostic methods, mycobacterial culture on liquid medium with a reduced incubation period of between 2 and 3 weeks7, and nucleic acid amplification methods, including the Xpert MTB/RIF assay, have been introduced8.
The aim of this study was to evaluate changes in TB diagnostic testing (which have prompted the initiation of anti-TB treatment) in South Korea, a high-income country in which the TB burden is intermediate.
Materials and Methods
1. Inclusion criteria and data collection
Patients diagnosed with pulmonary TB in the first 6 months (i.e., between January 1 and June 30) of 2005 or 2013, at Seoul National University Hospital (a university-affiliated tertiary referral hospital in South Korea) were included in this study. The study protocol was approved by the Institutional Review Board of Seoul National University Hospital.
2. Review of clinical findings and laboratory tests
We retrospectively reviewed the demographic and clinical characteristics of patients, including age, gender, and body mass index (BMI). In addition, we checked for the presence of previous TB, malignancy, diabetes mellitus, immunosuppressive drug therapy, solid organ transplantation, chronic kidney disease, chronic liver disease, and Hepatocyte growth factor, human immunodeficiency virus infection. The results of histopathological examinations and microbiological studies, including acid-fast bacilli (AFB) staining, mycobacterial cultures, and drug susceptibility tests, were also reviewed. Chest radiographs were reviewed for the presence of cavities, and to assess the extent of involvement.
3. Classification of diagnostic methods
The diagnostic methods applied to the two TB patient cohorts were compared. Diagnostic methods that prompted anti-TB medication initiation were classified into the following four groups:
1) Sputum-based diagnosis
- Positive staining for AFB
- Negative AFB but positive polymerase chain reaction (PCR) for Mycobacterium tuberculosis (M.TB)
- Negative AFB but positive culture of M.TB
2) Bronchoscopic specimen-based diagnosis
- Positive staining for AFB
- Negative AFB but positive PCR for M.TB
- Negative AFB but positive culture of M.TB
3) Pathological diagnosis
- Presence of caseating granulomas or positive AFB staining, or positive PCR for M.TB DNA, or growth of M.TB from tissue
4) Clinical diagnosis
- Physical findings (i.e., cough, generally of 2-3-week duration, lymphadenopathy, fevers, night sweats, weight loss) and radiographic features consistent with pulmonary TB
Patients were additionally classified based on the type of specimen from which M.TB was cultured.
4. Statistical analysis
Group comparisons of demographic characteristics, laboratory results, and radiographic findings were performed using Pearson's chi-square test or Fisher exact test for categorical variables, and Student's t test for continuous variables. To elucidate changes in diagnostic tools, Pearson's chi-square test or Fisher exact test was applied. A value of p<0.05 was taken to indicate statistical significance. All analyses were performed using the SPSS version 21 (IBM Corp., Armonk, NY, USA).
Results
1. Demographic and clinical characteristics of patients
During the first 6 months of 2005 and 2013, 150 and 151 patients, respectively, were diagnosed and treated for pulmonary TB at Seoul National University Hospital. The median age of TB patients in the 2005 group was 52 years; 88 of these patients (58%) were male. The median age of TB patients in the 2013 group was 53 years, of whom 91 (61%) were male. There were no group differences in BMI, past treatment of TB, or radiographic characteristics. However, malignancy was more common in the 2013 cohort compared with the 2005 cohort (16.7% vs. 2.6%, p<0.001) (Table 1).
Table 1. Demographic and clinical characteristics of patients in 2005 and 2013.
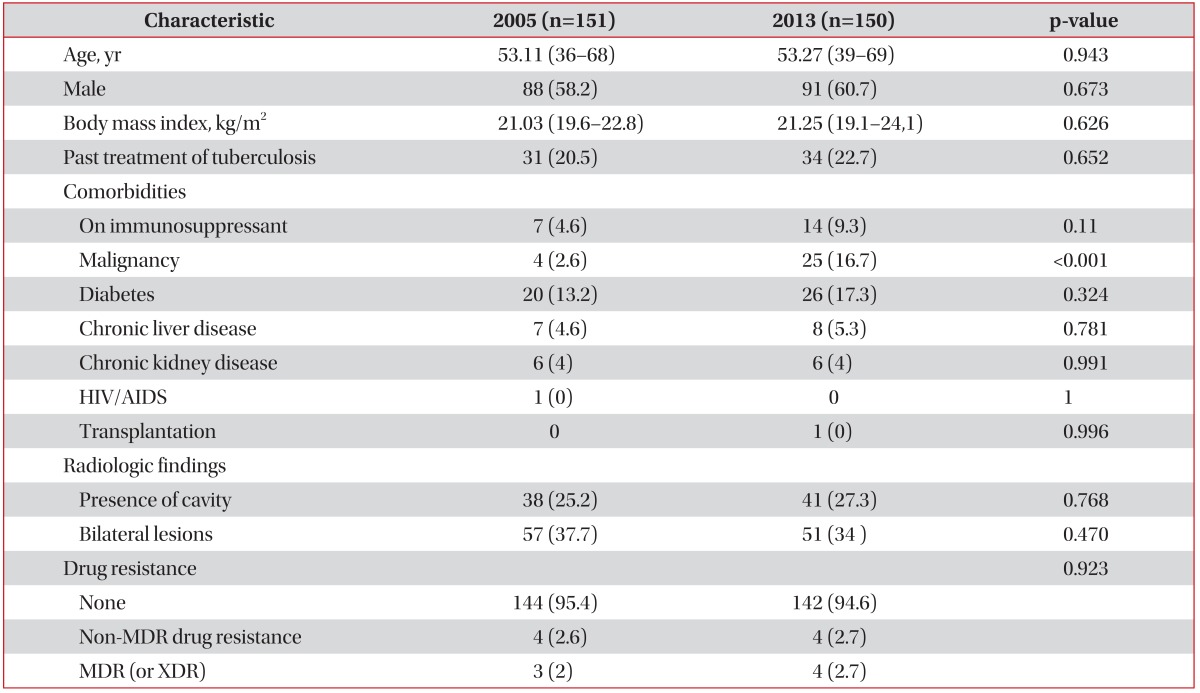
Values are presented as median (interquartile range) or number (%).
HIV: human immunodeficiency virus; AIDS: acquired immune deficiency syndrome; MDR: multidrug-resistant; XDR: extensively-drug resistant.
2. Diagnostic methods prompting use of anti-TB medication
Of the 151 TB patients diagnosed in 2005, 47 (31.1%) were initially diagnosed based on their sputum study results: 10 (6.6%) others were diagnosed based on their bronchoscopic specimens. Among them, eight patients submitted sputum for AFB staining and mycobacterial culture. In 20 patients (13.2%), anti-TB treatment was initiated based on pathological diagnosis; for the remaining 74 patients (49%), treatment was initiated based on clinical diagnosis (Table 2). Among these 74 patients, 51 submitted their sputum but none of them showed result for positive AFB staining.
Table 2. Diagnostic methods for the initiation of anti-tuberculosis medication in 2005 and 2013.
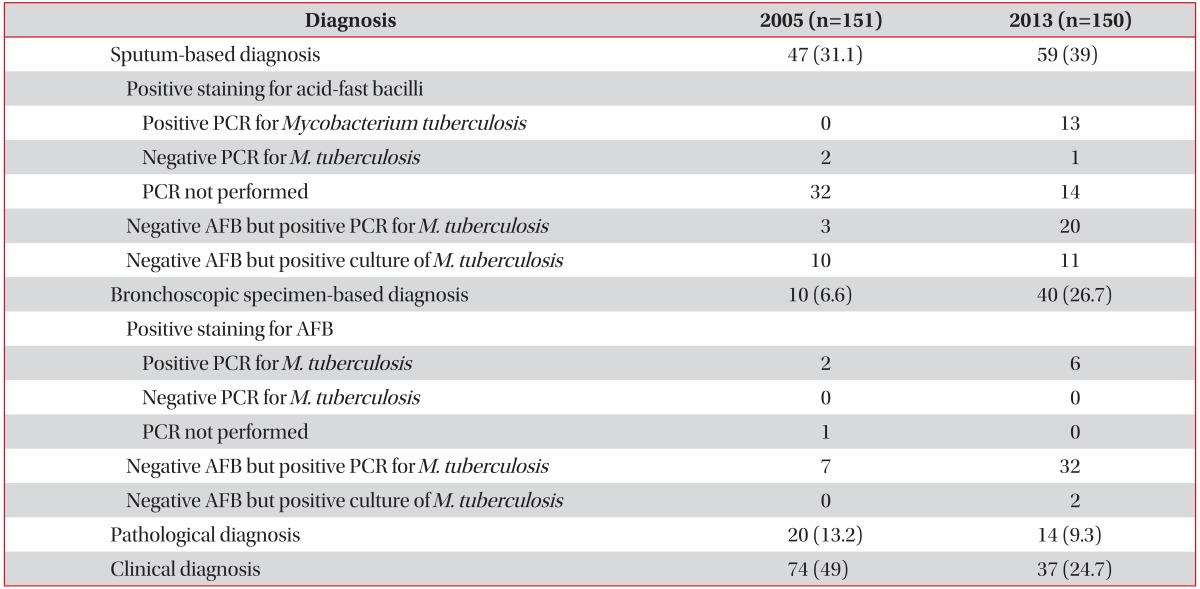
Values are presented as number (%).
PCR: polymerase chain reaction; AFB: acid-fast bacilli.
Of the 150 patients in 2013, 59 (39%) were diagnosed based on their sputum study results: 40 others (26.7%) were diagnosed based on their bronchoscopic specimens. Among them, 15 patients submitted sputum for AFB staining and mycobacterial culture. Fourteen patients (9.3%) were diagnosed following pathologic examination; the remaining 37 (24.7%) were diagnosed clinically (Table 2). Among these 37 patients, 25 submitted their sputum but none of them showed positive AFB staining.
Compared to the 2005 cohort, the proportion of TB patients diagnosed using bronchoscopy increased in 2013 (6.6% vs. 26.7%, p<0.001), whereas the proportion of clinically diagnosed TB cases decreased (49.0% vs. 24.7%, p<0.001). In addition, more patients in 2013, vs. 2005, had PCR results confirming TB infection prior to treatment commencement (47.3% vs. 7.9%, p<0.002).
3. Results of M.TB culture
In 2005, M.TB was cultured from sputum in 91 patients (60.3%); from bronchial washes in four patients (2.6%); and from biopsy specimens in six patients (4%). In total, M.TB was cultured from 101 patients (66.9%) in whom anti-TB medications had been initiated. In 2013, M.TB was cultured from sputum in 70 patients (46.7%); from bronchial washing in 27 patients (18%); and from biopsy specimens in two patients (13%). In total, M.TB was cultured from 99 patients (66.0%) in whom anti-TB medications were initiated (Table 3).
Table 3. Specimen types from which Mycobacterium tuberculosis was cultured in 2005 and 2013.
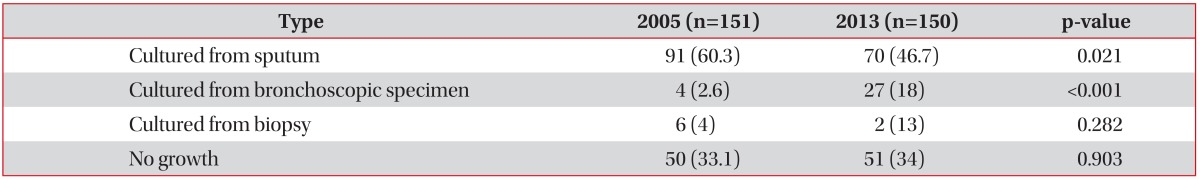
Values are presented as number (%).
Although the proportion of TB patients in whom M.TB was cultured did not differ (p=0.870), M.TB was cultured more frequently from bronchoscopic specimens in 2013 compared with 2005 (18.0% vs. 2.6%, p<0.001) (Table 3).
Discussion
In the present study, the diagnostic methods used for pulmonary TB in the first 6 months of 2005 and 2013 were compared. More TB patients were diagnosed using bronchoscopy in 2013 compared with 2005. Additionally, more patients received anti-TB treatments based upon the results of PCR, for M.TB DNA, in 2013. Conversely, the proportion of TB patients clinically diagnosed without bacteriological confirmation decreased in 2013, compared with 2005.
The utility of nucleic acid amplification tests, including PCR, is well-established: guidelines recommend using this method in cases of suspected TB8,9. Due to its good sensitivity and rapidity for detection of M.TB and rifampin resistance in sputum samples10,11 the Xpert MTB/RIF assay was endorsed by the World Health Organization for the diagnosis of pulmonary TB. The higher proportion of TB patients diagnosed using PCR methods in 2013 reflects this trend.
Recent studies illustrate the benefits of bronchoscopy as a diagnostic method in patients with possible pulmonary TB12,13. According to one of our recent studies, TB patients diagnosed using bronchoscopy exhibit higher culture conversion rates at 2 months and reduced time to culture conversion compared with other patients14. In this context, increased use of bronchoscopy to diagnose TB could have a positive impact on prognosis and disease transmission.
Regarding the present study's limitations, it is difficult to generalize the results due to the use of data from a single-center, in a developed country in which bronchoscopy and TB-PCR are readily available. Second, we evaluated the diagnostic methods only at two time points. Adopting more time points could provide more precise information. Third, the different methods for TB-PCR were used for 2005 and 2013 in our institution. This could affect the results of this study. Finally, the difference in experience of bronchoscopists as well as laboratory technicians between 2005 and 2013 could have affected the results of this study.
In conclusion, initiation of treatment for pulmonary TB in South Korea is more frequently based on PCR for M.TB DNA as well as bronchoscopic specimens gathered over time. Further study regarding whether changes in diagnosis influence treatment outcomes is required.
Footnotes
Conflicts of Interest: No potential conflict of interest relevant to this article was reported.
References
- 1.World Health Organization. Global tuberculosis report 2013. Geneva: World Health Organization; 2013. [Google Scholar]
- 2.Organisation for Economic Co-operation and Development; World Health Organization. Health at a glance: Asia/Pacific. Paris: OECD Publishing; 2012. [Google Scholar]
- 3.Korea Centers for Disease Control and Prevention. Annual report on the notified tuberculosis patient in Korea, 2013. Osong: Korea Centers for Disease Control and Prevention; 2014. [Google Scholar]
- 4.World Health Organization. Tuberculosis prevalence surveys: a handbook. Geneva: World Health Organization; 2011. [Google Scholar]
- 5.Steingart KR, Henry M, Ng V, Hopewell PC, Ramsay A, Cunningham J, et al. Fluorescence versus conventional sputum smear microscopy for tuberculosis: a systematic review. Lancet Infect Dis. 2006;6:570–581. doi: 10.1016/S1473-3099(06)70578-3. [DOI] [PubMed] [Google Scholar]
- 6.Morgan MA, Horstmeier CD, DeYoung DR, Roberts GD. Comparison of a radiometric method (BACTEC) and conventional culture media for recovery of mycobacteria from smear-negative specimens. J Clin Microbiol. 1983;18:384–388. doi: 10.1128/jcm.18.2.384-388.1983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dinnes J, Deeks J, Kunst H, Gibson A, Cummins E, Waugh N, et al. A systematic review of rapid diagnostic tests for the detection of tuberculosis infection. Health Technol Assess. 2007;11:1–196. doi: 10.3310/hta11030. [DOI] [PubMed] [Google Scholar]
- 8.Centers for Disease Control and Prevention (CDC) Updated guidelines for the use of nucleic acid amplification tests in the diagnosis of tuberculosis. MMWR Morb Mortal Wkly Rep. 2009;58:7–10. [PubMed] [Google Scholar]
- 9.National Collaborating Centre for Chronic Conditions (UK); Centre for Clinical Practice at NICE (UK) Tuberculosis: clinical diagnosis and management of tuberculosis, and measures for its prevention and control. London: National Institute for Health and Clinical Excellence; 2011. [PubMed] [Google Scholar]
- 10.Boehme CC, Nabeta P, Hillemann D, Nicol MP, Shenai S, Krapp F, et al. Rapid molecular detection of tuberculosis and rifampin resistance. N Engl J Med. 2010;363:1005–1015. doi: 10.1056/NEJMoa0907847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kwak N, Choi SM, Lee J, Park YS, Lee CH, Lee SM, et al. Diagnostic accuracy and turnaround time of the Xpert MTB/RIF assay in routine clinical practice. PLoS One. 2013;8:e77456. doi: 10.1371/journal.pone.0077456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lee HY, Seong MW, Park SS, Hwang SS, Lee J, Park YS, et al. Diagnostic accuracy of Xpert(R) MTB/RIF on bronchoscopy specimens in patients with suspected pulmonary tuberculosis. Int J Tuberc Lung Dis. 2013;17:917–921. doi: 10.5588/ijtld.12.0885. [DOI] [PubMed] [Google Scholar]
- 13.Willcox PA, Benatar SR, Potgieter PD. Use of the flexible fibreoptic bronchoscope in diagnosis of sputum-negative pulmonary tuberculosis. Thorax. 1982;37:598–601. doi: 10.1136/thx.37.8.598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lee HY, Chae KO, Lee CH, Choi SM, Lee J, Park YS, et al. Culture conversion rate at 2 months of treatment according to diagnostic methods among patients with culture-positive pulmonary tuberculosis. PLoS One. 2014;9:e103768. doi: 10.1371/journal.pone.0103768. [DOI] [PMC free article] [PubMed] [Google Scholar]


