Abstract
The oral rehabilitation with conventional removable partial dentures in Kennedy class I patients allows continuous bone resorption, dislodgment of the prosthesis during the mastication caused by the resilience of the mucosa, and rotation of the prosthesis. Thus, the associations of distal implants become an attractive modality of treatment for these patients. This case report presented an association of removable partial dentures, milled crowns and osseointegrated implants to rehabilitate a partial edentulous patient. A removable partial denture associated with implants and metal-ceramic milled crowns can offer excellent esthetics, and will improve function and biomechanics, at a reduced cost.
Keywords: Partial denture, Implants, Biomechanical, Prosthetics associations
Introduction
Oral health surveys have shown an overall decline in tooth loss, but an increase of partially edentulous patients [1, 2]. The posterior region of the oral cavity is usually the first area to lose teeth, and results in a multi-factorial process of bone loss, by alveolar bone resorption [3]. This process occurs throughout life and ultimately leads to reduced bone depth, compromising oral rehabilitation. This is particularly clinically relevant in the posterior area of both the maxillary and mandibular arches, due to the presence of important anatomical structures, as well as bone quantity and quality, which represent the main limiting factors for implant insertion.
The use of tooth-implants connections has been widely discussed as an option to treat partial edentulous patients [4–8]; however, there is controversy regarding the type of connection and the design concepts needed to minimize the range of side effects associated with this technique [5, 6]. Tooth intrusion seems to be the most significant complication, as it usually leads to malfunctioning of the new prosthesis [6, 8]. The removable partial denture (RPD) represents an option for extensive edentulous areas, although it is considered a poor alternative, especially in cases with free-end condition (Kennedy class I and II). The absence of a fixed posterior support can result in rotation of the RPD, damaging the remaining teeth. The distal portion of the RPD operates as a fulcrum, and this lever movement creates pressure on the soft tissues during the displacement of the free-end saddle, which is particularly significant in mandible [9]. The extent of this rotation is influenced by the degree of bone resorption, and depends on the resilience of the alveolar mucosa.
A strategically placed implant can improve the RPD’s biomechanics [10, 11], and avoid its rotation during function, by creating a fulcrum line between the teeth closest to the edentulous area [12]. This report describes the prosthodontic rehabilitation of a partial edentulous patient, in which distal implants were used in association a RPD and single crowns in the maxilla and mandible, to improve the biomechanical behavior of the RPD.
Case Report
An 86-year-old partially edentulous woman sought oral treatment with complaints of poor aesthetics and movement of her existing prosthesis during function (Fig. 1). Anamnesis, clinical examination, and panoramic radiography were used to diagnose this patient (Fig. 2). The patient had controlled hypertension, and displayed no symptoms of temporomandibular dysfunction, dental pain or xerostomy, and presented with satisfactory oral hygiene.
Fig. 1.

Clinical oral condition
Fig. 2.

Initial panoramic radiography
The Existing Restorations Under Diagnosis
At clinical examination, one tooth-implant supported fixed prosthesis was present in the right maxilla, and two others on both sides of the posterior mandible. Two crowns were located in the maxillary central incisor regions (# 8 and # 9), and an implant supported crown was located in the left maxillary lateral incisor region (# 10). A conventional fixed prosthesis was evident in the left maxilla, which was supported by the first molar and the left maxillary canine.
At radiography examination, the right maxillary first premolar presented with a vertical fracture. Periapical lesion was observed in the left maxillary first and second molars (# 14 and 15), and in the mandibular second pre molars (# 21 and 28), which also presented mobility at the clinical examination. After removal of the existing prostheses, the patient was classified as Kennedy class I in both arches. The remaining teeth were yellowish in color, widely worn, with cervical abrasion, but no caries was present. Different options of rehabilitation were proposed to the patient. One of which was implant insertion on the edentulous areas, but the patient did not wish to be submitted to a new surgery, due the associated morbidity and high cost of the treatment. Therefore, the patient received a conventional treatment of a RPD associated with implants in the posterior area, with the intention of improving the retention of the prosthesis and enhancing its biomechanical behavior.
The Modified Design Under Treatment Planning
During the first phase, periodontal therapy was performed after removing the existing prostheses, and the existing implants were maintained. The teeth showing excess mobility, without a possibility of treatment, were extracted (# 14, 15, 21 and 28).
After the periodontal therapy, with the patient in appropriate oral condition, the rehabilitation using a RPD was began. Initially, pillars (# 5, 11, 22 and 27) received metal-ceramic milled crowns, which acted as guides to attach the prosthesis, and improve the teeth design and retention of the clasps (Fig. 3a, b). Crowns were placed in position and were removed using condensation silicone impression (Speedx, Vigodent/Coltene, Rio de Janeiro, Brazil). A cast model was obtained to facilitate the fabrication of the cobalt-chromium alloy framework of the RPD. The framework was developed maintaining a space around the healing caps, allowing O-ring capture (Fig. 4a, b). A wax plan of the metal framework was then made, for mounting to the teeth, which permitted an esthetic and functional trial (Figs. 5, 6).
Fig. 3.
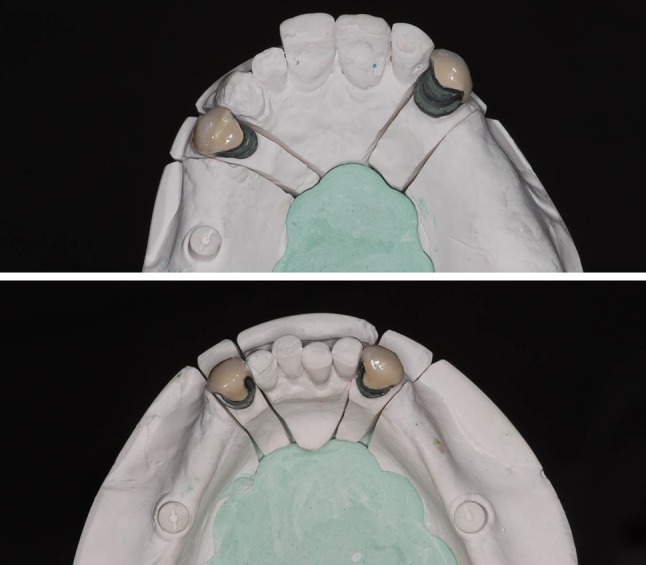
Metal-ceramic milled crowns in the master cast
Fig. 4.

Proof of the RPD framework, note design and the healing caps free access
Fig. 5.

Wax plan of the mouth to determine the vertical dimension and the maxilla-mandibular relationship
Fig. 6.

Esthetic try-in
The dentures were made with poly(methylmethacrylate) resin (JET, Classico, Sao Paulo, Brazil). Gingival color characterization was determined based on the second color of the Tomas Gomez System (STG, VIPI, Pirassununga, Brazil). During installation, the crowns were cemented with glass ionomer cement (Ketac Cem, 3 M Espe, St Paul, USA). Subsequently, ball attachments of 4.1 mm (Singo Vinces, Campo Largo, Brazil) were installed, with a recommended torque of 32 N/cm. The O-ring retainers were captured one by one, in the oral cavity (Fig. 7a, b). Restorative procedures were performed on the remaining teeth (# 6, 7, 23, 24, 25 and 26) using a nano-hybrid composite resin, shade A3 (New Brillant, Vigodent, Coltene, Rio de Janeiro, Brazil). After completion of all rehabilitation procedures; the occlusion was monitored and adjusted, if necessary.
Fig. 7.

O-ring retainers in position in the a superior and b inferior RPD
Prior to leaving the dental surgery, the patient was given a hygiene procedure to follow, and provided with instructions on how to remove and insert the prosthesis. A protocol of a periodic review was followed to observe the patient’s adaptation to the RPD. In addition, 14 months after the installation, the prosthesis and the remaining teeth were evaluated clinically, and radiographed (Figs. 8, 9). No resorption around the implants was observed, and there was no requirement for relining of prosthesis. Furthermore, no caries lesions or periodontal diseases were observed. The final outcome presented a satisfactory functionality and esthetic appearance to the patient.
Fig. 8.

Clinical final aspect
Fig. 9.

Radiography final aspect
Discussion
In this case the use of RPDs associated with implants was an alternative to unsuccessful fixed tooth-implant therapy. The existing implants supported the RPD thereby improving the biomechanics. The RPD has the potential to solve clinical problems linked to teeth-implant associations, including a fail of osseointegration, screw-loosening, or prosthesis failure as reported [13–15]. In this clinical report, the patient presented with previously fixed prostheses, which failed, and she declined any additional surgery. There is no consensus regarding the union of tooth-implants to restore partial edentulous patients, and this association should only be performed in specific cases [6, 8, 16, 17]. Moreover, the lack of a periodontal ligament in implants results in the increased risk of intrusion of natural teeth can lead to movement of the remaining teeth [6, 8, 18, 19].
After considering all options of treatment a RPD associated to implants, and the restoration of the remaining teeth was the treatment chosen in consensus. This option provided cost-effective advantages and good aesthetics [20]. The implants in the posterior regions offered good retention of the RPD, and reduced the lever movement that could overload the distal pillar. The distal support reduced the movements of the prosthesis in the free-end space, preserving the remaining teeth [21].
The free-end saddle, present as Kennedy class I and II, can result in lever movement creating pressure on the soft tissues during vertical displacement, which may lead to destructive lateral forces on the remaining teeth [22]. This would occur mainly in the mandible, since support is provided by hard palate in the maxilla [9]. This explains why no extra implants were inserted into the free-end space in the maxilla. Implants placed distally, especially in second molar area, would effectively change the Kennedy class I or II to Kennedy class III, and eliminate the vertical movement [11], improving stability and/or retention and avoiding repeated relining of the prosthesis [10]. This will improve patient satisfaction, by offering better comfort and function [12, 23]. In addition, the distal implants decreased the pressure exerted on the soft tissue, preventing alveolar bone resorption [24].
Instability of a mandibular denture during mastication is a common complaint in clinical practice. The implant-support improves masticatory function, and is the preferred option for the majority of patients [24]. Furthermore, the use of osseointegrated implants reduces the difficulties associated with a large edentulous space. The current esthetic concept requires that unaesthetic buccal retentive arm clasps must be avoided in anterior area [21]; however, in this case, the metallic clasps were used, as they were required to improve the retention of the RPD, due the large length of its removable base. Metal-ceramic milled crowns were made to serve as a framework for the prosthesis enhancing its stability and retention [25, 26]. They also helped preserve the ball attachments, by ensuring the denture settled down in the right position, avoiding the grooves at the sphere equator in the long-term [27].
The clinical choice described here represents a reliable and cost-effective treatment option [12]. It is a viable alternative to unsuccessful fixed implant therapy [13–15], as it will restore functionality and enhance esthetic appearance.
Conclusion
A RPD associated with implants and metal-ceramic milled crowns can offer excellent esthetics, and will improve function and biomechanics, at a reduced cost.
Acknowledgments
We wish to thank Dr. Lourdes Servían, specialist in restorative process, Uningá, University of Maringá/Bauru - SP, Brazil for her assistance in the oral rehabilitation.
Disclosure
All authors affirm that they do not have any financial interest in the products mentioned and have not received any remuneration for this article.
References
- 1.Douglass CW, Watson AJ. Future needs for fixed and removable partial dentures in the United States. J Prosthet Dent. 2002;87:9–14. doi: 10.1067/mpr.2002.121204. [DOI] [PubMed] [Google Scholar]
- 2.Kelly M, Steele J, Nuttal N. Adult dental health survey–oral health in the United Kingdom 1998. London: National Statistics Public Inquiry Service; 2000. [Google Scholar]
- 3.Soikkonen K, Ainamo A, Xie Q. Height of the residual ridge and radiographic appearance of bony structure in the jaws of clinically edentulous elderly people. J Oral Rehabilit. 1996;23:470–475. doi: 10.1111/j.1365-2842.1996.tb00881.x. [DOI] [PubMed] [Google Scholar]
- 4.Nickenig HJ, Schäfer C, Spiekermann H. Survival and complication rates of combined tooth-implant-supported fixed partial dentures (FPDs) Clin Oral Implant Res. 2006;17:506–511. doi: 10.1111/j.1600-0501.2006.01259.x. [DOI] [PubMed] [Google Scholar]
- 5.Akaça K, Uysal S, Çehreli MC. Implant–tooth-supported fixed partial prostheses: correlations between in vivo occlusal bite forces and marginal bone reactions. Clin Oral Implant Res. 2006;17:331–336. doi: 10.1111/j.1600-0501.2005.01169.x. [DOI] [PubMed] [Google Scholar]
- 6.Chee WW, Mordohai N. Tooth-to-implant connection: a systematic review of the literature and a case report utilizing a new connection design. Clin Implant Dent Relat Res. 2010;12:122–133. doi: 10.1111/j.1708-8208.2008.00144.x. [DOI] [PubMed] [Google Scholar]
- 7.Abduo J. An innovative prostheses design for rehabilitation of severely mutilated dentition: a case report. J Adv Prosthodont. 2011;3:37–42. doi: 10.4047/jap.2011.3.1.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lang NP, Pjetursson BE, Tan K, Bragger U, Egger M, Zwahlen M. A systematic review of survival and complication rates of fixed partial dentures (FPDs) after an observation period of at least 5 years II. Combined tooth–implant-supported FPDs. Clin Oral Implant Res. 2004;15:643–653. doi: 10.1111/j.1600-0501.2004.01118.x. [DOI] [PubMed] [Google Scholar]
- 9.Ben-Ur Z, Aviv I, Maharshak B. Factors affecting displacement of free-end saddle removable partial dentures. Quintessence Int. 1991;22:23–27. [PubMed] [Google Scholar]
- 10.Mijiritsky E. Implants in conjunction with removable partial dentures: a literature review. Implant Dent. 2007;16(2):146–151. doi: 10.1097/ID.0b013e3180500b2c. [DOI] [PubMed] [Google Scholar]
- 11.Ohkubo C, Kurihara D, Shimpo H, Suzuki Y, Kokubo Y†, Hosoi Y. Effect of implant support on distal extension removable partial dentures: in vitro assessment. Oral Rehabilit. 2007;34:52–56. doi: 10.1111/j.1365-2842.2006.01641.x. [DOI] [PubMed] [Google Scholar]
- 12.Mijiritsky E, Ormianer Z, Klinger A, Mardinger O. Use of dental implants to improve unfavorable removable partial denture design. Compend Contin Educ Dent. 2005;26:744–746. [PubMed] [Google Scholar]
- 13.Mijiritsky E, Karas S. Removable partial denture desing involving teeth and implants as an alternative to unsuccessful fixed implant therapy: a case report. Implant Dent. 2004;13:218–220. doi: 10.1097/01.id.0000136919.13387.94. [DOI] [PubMed] [Google Scholar]
- 14.Asvanund C, Morgano SM. Restoration of unfavorably positioned implants for a partially edentulous patient by using an overdenture retained with milled bar and attachments: a clinical report. J Prosthet Dent. 2004;91:6–10. doi: 10.1016/j.prosdent.2003.09.009. [DOI] [PubMed] [Google Scholar]
- 15.Jivraj SA, Chee WWL. Use of a removable partial denture in the management of chronic screw loosening. J Prosthet Dent. 2005;93:13–16. doi: 10.1016/j.prosdent.2004.10.007. [DOI] [PubMed] [Google Scholar]
- 16.Pesun IJ. Intrusion of teeth in the combination implant-to-natural-tooth fixed partial denture: a review of the theories. J Prosthodont. 1997;6:268–277. doi: 10.1111/j.1532-849X.1997.tb00107.x. [DOI] [PubMed] [Google Scholar]
- 17.Pjetursson BE, Bragger U, Lang N, Zwahlen M. Comparison of survival and complication rates of tooth-supported fixed dental prostheses (FDPs) and implant-supported FDPs and single crowns (SCs) Clin Oral Implant Res. 2007;18(Suppl. 3):97–113. doi: 10.1111/j.1600-0501.2007.01439.x. [DOI] [PubMed] [Google Scholar]
- 18.Rieder CE, Parel SM. A survey of natural tooth abutment intrusion with implant-connected fixed partial dentures. Int J Periodontics Restorative Dent. 1993;13:335–347. [PubMed] [Google Scholar]
- 19.Schlumberger TL, Bowley JF, Maze GI. Intrusion phenomenon in combination tooth-implant restorations: a review of the literature. J Prosthet Dent. 1998;80:199–203. doi: 10.1016/S0022-3913(98)70110-6. [DOI] [PubMed] [Google Scholar]
- 20.Bassi F. Comparing overdenture therapies with teeth and implant abutments. Int J Prosthodont. 2009;22:527–528. [PubMed] [Google Scholar]
- 21.Senna PM, Silva-Neto JP, Sanchez-Ayala A, Sotto-Maior BS. Implants to improve removable partial denture retention. Dent Today. 2011;30:118. [PubMed] [Google Scholar]
- 22.Voller R. Removable prosthetics: clinical indications and treatment principles. Dent Today. 2008;27(1):94–98. [PubMed] [Google Scholar]
- 23.Mitrani R, Brudvik JS, Phillips KM. Posterior implants for distal extension removable prostheses: a retrospective study. Int J Periodontics Restorative Dent. 2003;23:353–359. [PubMed] [Google Scholar]
- 24.Ohkubo C, Kobayashi M, Suzuki Y, Hosoi T. Effect of implant support on distal-extension removable partial dentures: in vivo assessment. Int J Oral Maxillofac Implant. 2008;23:1095–1101. [PubMed] [Google Scholar]
- 25.Chaiyabutr Y, Brudvik JS. Removable partial denture design using milled abutment surfaces and minimal soft tissue coverage for periodontally compromised teeth: a clinical report. J Prosthet Dent. 2008;99:263–266. doi: 10.1016/S0022-3913(08)60058-X. [DOI] [PubMed] [Google Scholar]
- 26.Brudvik JS, Shor A. The milled surface as a precision attachment. Dent Clin North Am. 2004;48:685–708. doi: 10.1016/j.cden.2004.03.005. [DOI] [PubMed] [Google Scholar]
- 27.Wolf K, Ludwig K, Hartfil H, Kern M. Analysis of retention and wear of ball attachments. Quintessence Int. 2009;40:405–412. [PubMed] [Google Scholar]


