Abstract
The implementation of the Home Health Prospective Payment System in 2000 led to a dramatic reduction in home health length of stay and number of skilled nursing visits among Medicare beneficiaries. While policy leaders have focused on the rising costs of home health care, its potential underutilization and the relationship between service use and patient outcomes including hospitalization rates have not been rigorously examined. A secondary analysis of five Medicare-owned assessment and claims data sets for the year 2009 was conducted among two independently randomly selected samples of Medicare-reimbursed home health recipients (each n=31,485) to examine the relationship between home health length of stay or number of skilled nursing visits and hospitalization rates within 90 days of discharge from home health. Patients who had a home health length of stay of at least 22 days or received at least 4 skilled nursing visits had significantly lower odds of hospitalization than patients with shorter home health stays and fewer skilled nursing visits. Additional study is needed to clarify the best way to structure home health services and determine readiness for discharge to reduce hospitalization among this chronically ill population. In the mean time, the findings of this study suggest that home health providers should consider the benefits of at least four SNV and/or a home health LOS of 22 days or longer.
Keywords: skilled home health, hospitalization, Medicare, older adults, propensity score analysis
The Home Health Prospective Payment System (PPS) was implemented in 2000 as a result of escalating costs within the industry (Komisar, 2002). Home Health PPS restructured skilled home health reimbursement from a cost-based, fee-for-service system to a 60-day episodic payment determined by the Outcomes Assessment Information Set (OASIS). This per-episode payment includes reimbursement of intermittent skilled nursing, home health aide, therapy, medical social service visits, and non-routine medical supplies (Medicare Payment Advisory Commission [MedPAC], 2014). To receive the full episodic payment under Home Health PPS, Medicare beneficiaries must receive a minimum of five home health visits (including skilled nursing, physical therapy, occupational therapy, speech-language pathology, medical social work, or home health aide visits) during a 60-day episode (Centers for Medicare and Medicaid [CMS], 2012a), but agencies that provide more than five visits receive no more than the full episodic payment. Thus, Home Health PPS provides a financial incentive for home health agencies to limit both the number of visits and home health length of stay (LOS) in each 60-day episode. Potential underutilization of home health since the implementation of the Home Health PPS has not been adequately explored (Anderson et al., 2005), and whether a reduction in home health visits is linked to later hospitalization of Medicare beneficiaries has not been studied.
The financial and human costs associated with hospitalization are a tremendous burden on society, patients and caregivers. Hospitalization leads to increased costs for payers, leaves older adults at risk for adverse events such as medical errors (Institute of Medicine [IOM], 1999; 2001), reduces quality of life for patients and their caregivers through psychological distress (Naylor, Stephens, Bowles & Bixby, 2005), and exposes already-compromised elders to further decline and reduced functional status (Covinsky, Pierluissi & Johnston, 2011). Among all Medicare beneficiaries, nearly 20% discharged from hospitals are rehospitalized within 30 days, and 34% are rehospitalized within 90 days (Jencks, Williams & Coleman, 2009). MedPAC (2014) reported that 29% of skilled home health episodes that follow a hospitalization were followed by rehospitalization. The purpose of this study was to examine the association between home health LOS, the number of skilled nursing visits (SNV), and hospitalization rates within 90 days of home health discharge among Medicare beneficiaries who received only one 60-day home health episode and did not experience a hospitalization while receiving home health services.
Reductions in Home Health Care Under PPS
Number of visits
Implementation of the Home Health PPS was followed by a dramatic reduction in the number of visits (United States General Accounting Office [GAO], 2000; Eaton, 2005) and home health LOS (Murkofsky, Phillips, McCarthy, Davis, & Hamel 2003; Anderson, Clarke, Helms & Foreman, 2005). In 1997, prior to the Home Health PPS, Medicare recipients received an average of 73 total visits per home health admission. In 2000, the year the Home Health PPS was implemented, Medicare beneficiaries received an average of 37 total visits per home health admission (MedPAC, 2014), a reduction of 49%. Home health visits were further reduced to an average of 33 visits per home health admission in 2012, representing an additional 10% reduction since the Home Health PPS was implemented (MedPAC).
Length of stay
The average length of stay per Medicare-reimbursed home health episode decreased 37%, from 106 to 69 days, after the Home Health PPS was implemented (McCall & Korb, 2003). In another analysis, Medicare -reimbursed home health recipients had an average home health LOS of approximately 45 days (Schade & Brehm, 2010). In a retrospective study of national data, since Home Health PPS implementation in 2000, Medicare patients were 2.9 times more likely to be discharged from home health within the first 60 days of admission than Medicare patients who received services in prior years (Han & Remsburg, 2005).
Madigan (2008) reported that 85% of home health beneficiaries with heart failure completed home health services within one episode, and less than 5% received more than one episode. Many patients were discharged from home health with unresolved issues related to wounds, cognition, behavioral and continence status and demonstrated less improvement overall compared to patients who received home health services prior to implementation of the Home Health PPS (Eaton, 2005; Madigan 2001; Schlenker, Powell & Goodrich, 2005).
Financial Incentive to Reduce Home Health LOS under the Home Health PPS
Health care organizations are sensitive to reimbursement incentives such as those imposed by the Home Health PPS (MedPAC, 2010). Limiting reimbursement for health care resulted in the provision of fewer services (Murkofsky et al., 2003). In a retrospective analysis, patients with a longer home health LOS under the Home Health PPS contributed to financial loss for the agency (Livesay, Hanson, Anderson & Oelschlaeger, 2003). Under the Home Health PPS, agencies not only have a financial incentive to discharge patients quickly but have little incentive to focus on longer-term quality outcomes. Patients who are hospitalized after being discharged from home health services are not included in the acute care hospitalization rate reported on the CMS Home Health Compare website.
Rising Costs of Both Home Health Care and Hospitalization
Despite reductions in home health visits and LOS, in 2012, approximately 3.4 million Medicare beneficiaries received home health services from over 12,311 agencies costing Medicare $18 billion (MedPAC, 2014). Home health costs increased by 89% between 2002 and 2012.
Hospitalization costs incurred by Medicare beneficiaries in 2012 rose to $120 billion from $110 billion in 2006 (MedPAC, 2014). Medicare expenditures for unplanned and potentially preventable hospitalizations may be as high as $12 billion a year (MedPAC, 2007). Consequently, preventing avoidable hospitalizations is a national health care priority, as such adverse events result in unnecessary costs for payers and leaves older adults at risk for adverse events during and after the hospital admission (IOM, 1999; Lum, Studenski, Degenholtz & Hardy, 2012; Mandawat, Mandawat, Mandawat & Tinetti, 2012).
Hospitalization after Home Health Discharge
Approximately 29% of home health episodes result in a hospital admission (MedPAC, 2014), but empirical evidence regarding factors contributing to hospitalizations following home health discharge is limited. The lack of an evidence base for optimal home health LOS combined with the financial incentives to shorten home health stays under Medicare's Home Health PPS may be contributing to hospitalizations following discharge from home health among a growing population of older adults coping with multiple chronic conditions. Thus, the generation of evidence to understand contributing factors to hospital admissions following home health discharge is crucial to the reduction of health care costs and to prevent further decline among vulnerable older adults.
The purpose of this study was to examine the association between home health LOS and the number of skilled nursing visits (SNV) on hospitalization rates within 90 days of home health discharge among Medicare beneficiaries, who received only one 60-day home health episode and did not experience a hospitalization while receiving home health services. Hypothesis One was that a home health LOS less than or equal to 3 weeks would be associated with a higher occurrence of hospitalization within 90 days of home health discharge than patients who received a longer home health LOS. Hypothesis Two was home health episodes consisting of three or fewer SNVs will be associated with a higher occurrence of hospitalization within 90 days of home health discharge than patients who received more than three SNVs within one 60-day episode.
Methods
Design
A retrospective, observational study of five CMS-owned administrative and claims databases for the year 2009 was conducted to examine the association between home health LOS, number of SNVs, and the occurrence of hospitalization within 90 days of home health discharge. Propensity score analysis was used to reduce known confounding among covariates prior to the application of logistic regression analyses. This study was approved using the expedited review procedure by the University's Institutional Review Board, Office of Regulatory Affairs.
Data Sets
Five 2009 assessment and claims data sets were obtained from CMS, through the Research Data Assistance Center (ResDAC). A 5% sample of the Outcome Assessment Information Set (OASIS) was then cross-referenced to the home health and hospital claims, eligibility, and provider files. The five 2009 data sets (ResDAC, 2013) were: OASIS, Home Health Standard Analytic File (HHSAF), Medicare Provider and Analysis Review file (MedPAR; short stay/long stay/skilled nursing facility), Denominator/Eligibility File, and the Provider of Services file (POS). The OASIS is part of a required comprehensive assessment for all Medicare and Medicaid-reimbursed patients who receive skilled home health. OASIS data form the basis for home health reimbursement and patient outcome reports (CMS, 2012b).
Power Analysis
An adequately powered study is designed to detect both statistically and clinically meaningful differences in outcome between groups. This study was powered for a three-group comparison to detect very small differences. Because the use of all eligible subjects in the dataset would lead to an overpowered study, a random sample of eligible subjects was selected. The estimated sample size was based on a logistic regression of hospitalization on HH LOS. Based on prior research (O'Connor, Hanlon, Naylor & Bowles, 2012), a 2% difference in hospitalization among the three groups was expected. To detect significant differences between the three groups, a z-test for testing equality of proportions with a sample size of 10,495 subjects per group would achieve 90% power at a 0.05 significance level (to account for pairwise differences between the three LOS groups) to detect a 2% difference (16% for medium LOS vs 18% for short LOS) in the probability of being hospitalized within 90 days of discharge. Simple random selection without replacement was accomplished using SAS™ version 9.3. Separate random samples were drawn for the home health LOS and SNV analyses.
Sample
Two independent, random samples (each with an n=31,485) were drawn to analyze the role of the two hypothesized predictors of hospitalization (home health LOS and number of SNVs). Inclusion criteria included receiving Medicare-reimbursed skilled home health in 2009, with a single, 60-day home health episode. Medicare beneficiaries were excluded from the study if they were hospitalized or died during the home health episode or if more than one home health episode (>60 days) at a time was received. Additional exclusion criteria included beginning home health services before February 1, 2009 (to allow for detection of a hospital discharge within 30 days prior to home health admission) or after September 30, 2009 (to allow for 90 days follow up). OASIS assessments without a corresponding claim were also excluded. Finally, only the index home health admission was included.
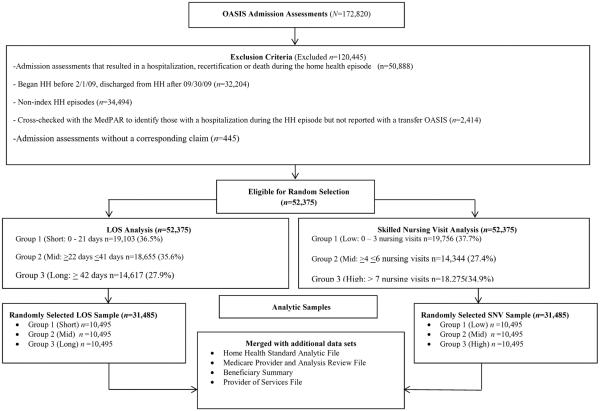
Grouping of Sample for Analysis
Figure 1 depicts the process used to prepare the final analytic file. After applying the exclusion criteria (Figure 1), 52,375 eligible home health recipients remained in the data set. These were divided into three groups based on the frequency distribution of the predictors of interest: home health LOS (low, medium, high) and number of SNVs (low, medium, high).
Figure 1.
Preparation of the Analytic Data File
The home health LOS distribution revealed that 33% of eligible beneficiaries received a home health LOS of 0 to 21 days (low). The middle third of eligible beneficiaries received between 22 and 41 days of home health (medium). The upper third of the data set received between 42 and 59 days of home health (high). In the SNV analysis, the first 33% of the sample received 0 to 3 SNVs (low). The middle third received between 4 and 6 SNVs (medium) and the upper third received 7 SNVs or more (high).
Variables
Independent variables
Home health LOS (low≤21 days; medium≥22 and ≤41 days; high≥42 days) was the independent variable in one sample, and number of SNVs (low≤3 SNVs; medium≥4 and ≤6 SNVs; high≥7 SNVs) was the independent variable in the second sample. Home health LOS was measured from the start of care or day of admission, as defined by the first service date on the home health claim found on the HHSAF until the day of discharge.
Covariates
O'Connor (2012) described patient characteristics associated with risk of hospitalization among home health recipients and categorized the risk factors in the domains of sociodemographic characteristics, clinical history, and functional status. These factors were extracted either from the OASIS, HHSAF or Provider of Services summary file (Table 1). According to Austin (2011),
There is a lack of consensus in the applied literature as to which variables to include in the propensity score model. Possible sets of variables for inclusion in the propensity score model include the following: all measured baseline covariates, all baseline covariates that are associated with treatment assignment, all covariates that affect the outcome (i.e., the potential confounders), and all covariates that affect both treatment assignment and the outcome (i.e., the true confounders). (p. 414)
Therefore, we chose to include all observed baseline variables that were associated with the SNV/LOS, risk of hospitalization, or both.
Table 1.
Study Variables and Sources
| Variable Type | Variable | Source |
|---|---|---|
| Outcome | Hospitalization (occurrence of a hospital admission, all causes) | MedPAR |
| Independent | Home health Length of Stay Group | HHSAF |
| (Low: 0 – 21 days, Medium: 22–41 days, High: ≥ 42 days) | ||
| Number of Skilled Nursing Visits Group (Low: 0–3, Medium: 4–6, High: ≥ 7) | HHSAF | |
| Covariates (continuous) | Number of diagnoses | HHSAF |
| High risk diagnosis counta | HHSAF | |
| Severity of illness | OASIS | |
| Age | OASIS | |
| Confusion | OASIS | |
| Cognitive function | OASIS | |
| Bathing ability | OASIS | |
| Ambulation ability | OASIS | |
| Dyspnea | OASIS | |
| Anxiety | OASIS | |
| Transfer ability | OASIS | |
| Feeding ability | OASIS | |
| Ambulation ability | OASIS | |
| Living alone | OASIS | |
| Covariates (dichotomous) | Urinary incontinence | OASIS |
| Depressed mood | OASIS | |
| Memory deficits | OASIS | |
| Female | OASIS | |
| Hispanic | OASIS | |
| White | OASIS | |
| Prior inpatient stay | MedPAR | |
| Serviced by a for-profit home health agency | POS File | |
| Presence of a primary caregiver | OASIS | |
| Covariates (categorical) | Guarded rehabilitative prognosis | OASIS |
| Requires assistance with ADLs | OASIS | |
| Requires assistance with IADLs | OASIS | |
| Presence of a pressure ulcer | OASIS | |
| Presence of a stasis ulcer | OASIS | |
| Requires assistance with oral medications | OASIS |
DM, depression, ischemic heart disease, HIV/AIDS, renal failure, HF, COPD; cardiomyopathy, dysrythmia, skin ulcers, CAD, Alzheimer's disease, HTN, personality disorders, osteoporosis, MI, wounds
Several of the variables derived from the OASIS have a category of “unknown.” This is not missing data, but is rather an option on the OASIS assessment when the clinician was unable to accurately determine the appropriate answer at the time the tool was completed and is therefore considered an acceptable response (ResDAC, 2013). It should also be noted that while we did have subjects with “unknown” as a response, there was no missing data among the eligible subjects. Because the OASIS is the mechanism that supports skilled home health reimbursement from CMS and the commercially available OASIS submission software, missing data in the OASIS submission is uncommon.
Outcome variable
The occurrence of hospitalization following discharge from home health services was measured beginning the day after home health discharge and ended 90 days following home health discharge and was found in the MedPAR file (ResDAC, 2013).
Statistical Analysis
Because home health LOS and number of SNV were highly correlated (0.40, p<0.01), two separate analyses were conducted. Two independent randomly selected samples totaling 31,485 Medicare-reimbursed home health recipients were created for the two analyses.
Propensity score analysis (Rosenbaum & Rubin, 1983) using matching methods (Stuart, 2010) was conducted to balance the distribution of observed covariates across the three independent variable groups in each sample (Rubin, 1997). Propensity score analysis controls for observed confounders that might influence group assignment (Rosenbaum & Rubin, 1983) by reducing the confounding covariates into a single variable, the propensity score. The propensity scores were created using the covariates found in Table 1 and were matched using the full-matching technique (Stuart & Green, 2008). Covariates were carefully selected and checked for multicollinearity.
Matching methods balance the distribution of observed covariates in the comparison groups, imitating what would have occurred in a randomized controlled trial (Stuart, 2010). This controls for the observed confounders between the groups. Therefore, after matching, beneficiaries with similar propensity scores in the three groups had similar distributions of the observed covariates included in the propensity score (Stuart & Green, 2008). To assess the performance of the matching method, the covariate balance in the “treated” and “control” groups is compared by examining the absolute standardized mean difference (ASMD), which is the weighted difference in means, divided by the standard deviation in the original full comparison group (Rubin, 1997). Standardized biases of less than 0.20 imply the groups are well-matched (Ho, Imai, King & Stuart, 2007).
After matching, all covariates had an ASMD well below the 0.20 threshold, indicating excellent balance (results available from the authors). Additional assessment on the effectiveness of the propensity score matching was evaluated in three diagnostic plots: convergence with dot plots, overlap between groups using side-by-side box plots, and balance using line plots pre and post weighting. All diagnostic plots indicated accurate propensity score estimates. Linearity was examined using the Hosmer-Lemeshow test of goodness of fit, which showed no indication of lack of fit.
Following propensity score analysis, bivariate logistic regression models were conducted for each independent variable using the SAS Proc Logistic feature. Other than the primary predictors of interest, LOS and SNV, only covariates demonstrating significance at the p≤0.05 level in the bivariate analyses were included in the final multivariate analyses (Kleinbaum, Kupper, Nizam & Muller, 2008). Statistical significance in the final analyses was set at p≤0.05.
The occurrence of hospitalization was regressed on home health LOS and number of SNV using adjusted and unadjusted logistic regression modeling. Variables significant at the 0.05 level were included in the adjusted modeling. Both models in the home health LOS and SNV analyses included weights as generated by the propensity score analysis. Odds ratios for independent variables along with their 95% confidence intervals are reported.
Results
Home Health Length of Stay and Hospitalization
Patients in this sample were on average, 77.6 years old, 63.7% women, 80.3% white, had 5.5 comorbid conditions, and received a mean LOS of 32 days in skilled home health. After weighting (Table 2), the hospitalization rates among the three LOS groups were significantly different, with the most hospitalizations occurring in the low LOS group (17.1%) compared to the medium (15.5%) and high (15.2%) LOS groups (p<0.01).
Table 2.
90-Day Hospital Admission Rates In Low, Medium, and High Length of Stay and Skilled Nursing Visit Groups
| Length of Stay Groupsa |
Skilled Nursing Visit Groupsb |
|||||||
|---|---|---|---|---|---|---|---|---|
| Low | Medium | High | p * | Low | Medium | High | p * | |
| Unweighted | 15.68% | 15.34% | 16.41% | 0.09 | 23.3% | 10.8% | 11.7% | <0.01 |
| Weighted | 17.09% | 15.51% | 15.19% | <0.01 | 24.7% | 11.4% | 11.2% | <0.01 |
Low: 0 – 21 days, medium: 22–41 days, high: ≥ 42 days
Low: 0–3, Medium: 4–6, High: ≥ 7 visits
Chi-square
The weighted model (Table 3) indicates a home health LOS of 22 to 41 days or more (medium), when compared to a LOS of 21 days or less (low), decreased the odds of hospitalization by 11% (p<0.01), and that a home health LOS of 42 days or more (high), when compared to a LOS of 21 days or less (low), decreased the odds of hospitalization by 13% (p<0.01). There was minimal difference in the odds of hospitalization between the medium and high home health LOS groups. Hypothesis One, that a home health LOS less than or equal to 3 weeks would be associated with a higher occurrence of hospitalization within 90 days of home health discharge than patients who received a longer home health LOS, was supported.
Table 3.
Home Health Length of Stay as Predictor of Hospital Admission within 90 Days of Home Health Discharge: Logistic Regression Models
| Unadjusted Models | Adjusted Model* | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
|
||||||||||
| Unweighted | OR | SE | 95% CI | P | OR | SE | 95% CI | P | ||
| Medium vs. High Length of Stay | 0.92 | 0.03 | 0.86 | 0.99 | 0.03 | 1.03 | 0.04 | 0.95 | 1.11 | 0.45 |
| Medium vs. Low Length of Stay | 0.97 | 0.04 | 0.90 | 1.05 | 0.49 | 0.90 | 0.04 | 0.83 | 0.97 | <0.01 |
| High vs. Low Length of Stay | 1.06 | 0.04 | 0.98 | 1.14 | 0.15 | 0.87 | 0.03 | 0.81 | 0.94 | <0.01 |
| PS-weighted | OR | SE | 95% CI | P | |
|---|---|---|---|---|---|
| Medium vs. High Length of Stay | 1.03 | 0.02 | 0.98 | 1.07 | 0.27 |
| Medium vs. Low Length of Stay | 0.89 | 0.02 | 0.85 | 0.93 | <0.01 |
| High vs. Low Length of Stay | 0.87 | 0.02 | 0.83 | 0.91 | <0.01 |
Note. OR = odds ratio; SE = standard error (per the delta method); 95% CI = 95% confidence interval, PS=propensity score.
Adjusted for the following 12 covariates based on imbalance before weighting: confusion, cognitive function, bathing ability, ambulation ability, presence of dyspnea, transfer ability, feeding ability, urinary incontinence, prior inpatient stay, serviced by a for-profit home health agency, presence of a pressure ulcer, requires assistance with oral medications. Adjusted and PS weighted model findings are similar, but variability in the PS weighted model is significantly reduced over the adjusted model.
Number of Skilled Nursing Visits and Hospitalization
Patients in this analysis were on average, 77.7 years old, 63.3% women, 80.7% white, had 5.5 comorbid conditions, and received a mean of 5.7 SNV. After weighting (Table 2), the hospitalization rates among the three SNV groups were significantly different, with the most hospitalizations occurring in the low SNV group (24.7%), compared to the mid (11.4%) and high (11.2%) number of SNV groups (p<0.01).
The weighted model (Table 4) indicated that 4 to 6 SNV (medium), when compared to 3 SNV or less (low), decreased the odds of hospitalization by 61% (p<0.01), and that 7 SNV or more (high), when compared to 3 SNV or less (low), decreased the odds of hospitalization by 62% (p<0.01). As was found in the home health LOS analysis, there was minimal difference in the odds of hospitalization between the medium and high SNV groups. Hypothesis Two, that home health episodes consisting of 3 or fewer SNVs will be associated with a higher occurrence of hospitalization within 90 days of home health discharge than patients who received more than 3 SNVs within one 60-day episode, was supported.
Table 4.
Number of Skilled Nursing Visits as Predictor of Hospital Admission within 90 Days of Home Health Discharge: Logistic Regression Models
| Unadjusted Model | Adjusted Model* | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
|
||||||||||
| Unweighted | OR | SE | 95% CI | P | OR | SE | 95% CI | P | ||
| Medium vs. High | 0.91 | 0.04 | 0.91 | 0.84 | 0.04 | 1.05 | 0.05 | 0.96 | 1.15 | 0.28 |
| Medium vs. Low | 0.40 | 0.02 | 0.40 | 0.37 | <0.01 | 0.40 | 0.02 | 0.37 | 0.44 | <0.01 |
| High vs. Low | 0.44 | 0.02 | 0.40 | 0.47 | <0.01 | 0.38 | 0.02 | 0.36 | 0.42 | <0.01 |
| PS-weighted | OR | SE | 95% CI | P | |
|---|---|---|---|---|---|
| Medium vs. High | 1.02 | 0.03 | 0.97 | 1.07 | 0.45 |
| Medium vs. Low | 0.39 | 0.01 | 0.37 | 0.41 | <0.01 |
| High vs. Low | 0.38 | 0.01 | 0.37 | 0.40 | <0.01 |
Note. Note. OR = odds ratio; SE = standard error (per the delta method); 95% CI = 95% confidence interval, PS=propensity score.
Adjusted model includes adjustment for the following 3 covariates based imbalance before weighting: number of high risk diagnoses, presence of dyspnea, prior inpatient stay. Adjusted and PS weighted model findings are similar but variability in the PS weighted model is significantly reduced over the adjusted model.
Discussion
Home health LOS as well as number of SNV were associated with the occurrence of hospitalization among Medicare-reimbursed skilled home health beneficiaries. Given these results, the number of SNV appears to have a greater impact on hospitalization than the home health LOS. However, keeping Medicare beneficiaries in skilled home health services for 22 days or more or by providing at least four SNV could result in fewer hospitalizations following home health discharge among the fee-for-service Medicare population.
Fewer subsequent hospitalizations among this chronically ill population could reduce the potential for medical errors (IOM, 1999; 2001), decline in function, reduced quality of life (Naylor et al., 2005) and costs that accompany hospitalization among older adults. Furthermore, the costs of providing skilled home health could offset the costs related to hospitalization. In 2012, CMS spent $18 billion on home health services and $120 billion on hospitalization costs incurred by fee-for-service Medicare beneficiaries (MedPAC, 2014). Decreasing hospitalizations by 5.2% could save CMS an estimated $5 billion annually (MedPAC, 2007). However, further research is required to identify which patients require more SNV or a longer home health LOS because it would be cost-prohibitive to provide this level of services to every Medicare-reimbursed skilled home health patient.
Several interventions during the home health episode, such as remote telehealth monitoring (Bowles et al., 2011; Bowles, Holland & Horowitz, 2009; Dansky, Vasey & Bowles, 2008), could be implemented during a longer home health episode (≥ 22 days) to keep a vigilant watch on Medicare beneficiaries between SNV. Disease management (Bowles, Holland, et al., 2009; Quinn, 2006) and evidence-based nursing protocols (Feldman et al., 2004) have also been effective. Implementation of transitional care between hospitalization and home health services is another effective strategy to reduce the need for hospitalization among chronically ill older adults, allowing them to transfer safely from one level of care or setting to another (Naylor et al., 2004; Naylor et al., 2005; Naylor, Aiken, Kurtzman, Olds & Hirschman, 2011).
While this study focused on traditional Medicare-reimbursed home health recipients, study findings could have implications for managed-Medicare recipients as well. Managed-Medicare home health recipients receive even less home health care than traditional Medicare-reimbursed home health beneficiaries (Experton, Li, Branch, Ozminkowski & Mellon-Lacey, 1997; Experton, Ozminkowski, Pearlman, Li &Thompson, 1999; Schlenker, Shaughnessy & Hittle, 1995). Thus, managed-Medicare home health recipients are at risk for hospitalization related to receiving a reduced number of SNV and a shortened home health LOS. More recent studies of managed-Medicare home health utilization could not be found, most likely because CMS (MedPAR, HHSAF) does not require managed-Medicare providers to submit claims for analysis (Jencks et al., 2009).
The findings of this study also have implications for home health agency administrators. Skilled home health is often a replacement for more expensive post-acute services and is used to avoid or delay hospitalization (MedPAC, 2014). However, as suggested in this study, too little skilled home health can lead to adverse outcomes. Furthermore, generally accepted home health standards and evidence-based practice recommendations regarding home health LOS and number of SNV are lacking (Murtaugh et al., 2009).
Home health LOS and number of SNV are a result of decision-making by home health agencies and clinicians, who may be influenced by the episodic reimbursement of the Home Health PPS but may be open to change. Particularly worthy of their attention are patients who do not receive any skilled nursing visits and are referred to as therapy-only patients. Twenty percent of our sample had no skilled nursing visits. Among these patients, 33% were hospitalized, as compared to 12% of those with at least one skilled nursing visit. Therapy-only patients should be reconsidered for skilled nursing needs due to the high percentage of hospitalizations among this group. Furthermore, Medicare-reimbursed home health recipients at high risk for hospitalization should be flagged upon admission to home health or even while still an inpatient. Each Medicare-reimbursed home health episode is potentially 60 days long. However, home health agencies and clinicians have the option to discharge patients from home health services prior to the completion of the 60-day episode. The findings of this study suggest that home health providers should consider the benefits of at least four SNV and/or a home health LOS of 22 days or longer.
In 2013, CMS announced its decision to further reduce skilled home health's 60-day episodic payment from 2014 to 2017 by 3.5 percent per year, known as rebasing (Office of the Federal Register, 2013). Based on 2011 data, Rosati and colleagues (2014) predicted that this reduction of the home health 60-day episodic payment may lead to higher service costs and therefore less profit, particularly for care of skilled home health patients with clinically complex conditions and social vulnerabilities (low income, living alone). Rebasing has the potential to further reduce access to skilled home health for these clinically complex and socially vulnerable patients and increase costs and adverse events such as hospitalization, emergency department use, and death.
Limitations
This study was subject to several limitations, most of which are inherent in secondary data analysis. The analyses were restricted to data collected in 2009 and included only one year of data. However, combining five data sets provided a unique opportunity to fulfill the study aims. The study design did not permit causal inferences. However, the application of propensity score analysis controlled the influence of confounders in analysis of dissimilar groups.
Other limitations are related to the data sets employed. The study included only traditional, fee-for-service Medicare beneficiaries because managed-Medicare beneficiary claims are not found in the MedPAR or HHSAF. OASIS data are collected by home health agency staff, which may compromise reliability and validity (O'Connor & Davitt, 2012). Information regarding the experience or expertise of the clinician completing the OASIS is not included in the data sets. No data on the length of SNVs or the type and quality of nursing interventions that occurred during visits were available.
Finally, while propensity score analysis reduced a great deal of bias, several potentially confounding factors were not included in the data sets and could not be controlled for in this analysis. These include primary care physician follow-up visits, access to primary care, and number of medications. Non-adherence by patients and socio-economic factors such as beneficiaries' education, income, financial resources, or their type of dwelling were not included in the data. Despite the limitations of the data sets, these data represent the largest and most robust source of information available to address the study hypotheses in this population and reflect the current state of the science in the provision and measurement of skilled home health.
Recommendations for Future Research
Results of this study indicate that some Medicare-reimbursed skilled home health patients are not receiving enough skilled nursing visits or an adequate home health LOS. This could be attributed to a lack of evidence-based protocols in skilled home health that assist clinicians to decide when to discharge from services. Bowles, Holmes and colleagues (2003; Bowles, Holmes, et al., 2009) are developing a body of evidence and decision support tools designed to assist inpatient discharge planners in identifying patients who are most appropriate for referral to post-acute services. Similarly, additional research is recommended to develop a discharge decision support tool to assist home health clinicians to determine discharge readiness from skilled home health. While the exact mechanisms by which SNV and home health LOS impact hospitalization are unknown, additional research is critical to assist home health clinicians to determine the ideal number of SNV and lengths of stay in home health, based on a Medicare beneficiary's characteristics and continuing need for home health services. Therapy-only patients also warrant further investigation.
The Patient Protection and Affordable Care Act of March 2010 empowered CMS to penalize hospitals financially for the readmission of heart failure, myocardial infarction and pneumonia patients within 30 days of hospital discharge. This has spurred a massive array of initiatives designed to reduce 30-day readmissions among Medicare beneficiaries. Further study of home health's role in preventing 30-day readmissions is imperative to furthering our understanding of how to improve this quality benchmark.
Conclusion
The findings of this study contribute to the body of evidence related to hospitalizations among Medicare home health beneficiaries and suggest that home health LOS and number of SNV may be important components to reducing hospitalization among this vulnerable population. Although not without limitations, these results help to inform current home health practice and future research. Additional study is needed to clarify the best way to structure home health services and determine readiness for discharge, in order to maximize home health benefits and reduce hospitalization among this chronically ill population. The challenges hospitalization imposes upon individuals and families are severe and extensive, posing a tremendous burden on all stakeholders, and the generation of evidence on contributors to hospital admissions is crucial to reduce health care costs and to prevent further decline among the elderly population.
Supplementary Material
Funding acknowledgements
This work was supported by the National Institute for Nursing Research [1F31NR012090]; the John A. Hartford Foundation's Patricia G. Archbold Scholarship [2010–2012]; the Frank Morgan Jones Fund; and the Center for Nursing Research, Villanova University College of Nursing.
References
- Anderson MA, Clarke MM, Helms LB, Foreman MD. Hospital readmission from home health care before and after prospective payment. Journal of Nursing Scholarship. 2005;37:73–79. doi: 10.1111/j.1547-5069.2005.00001.x. doi:10.1111/j.1547-5069.2005.00001.x. [DOI] [PubMed] [Google Scholar]
- Austin PC. An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivariate Behavioral Research. 2011;46:399–424. doi: 10.1080/00273171.2011.568786. doi:10.1080/00273171.2011.568786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowles KH, Foust JB, Naylor MD. Hospital discharge referral decision making: a multidisciplinary perspective. Applied Nursing Research. 2003;16:134–143. doi: 10.1016/s0897-1897(03)00048-x. doi:10.1016/S0897-1897(03)00048-X. [DOI] [PubMed] [Google Scholar]
- Bowles KH, Holland DE, Horowitz DA. A comparison of in-person home care, home care with telephone contact and home care with telemonitoring for disease management. Journal of Telemedicine and Telecare. 2009;15:344–350. doi: 10.1258/jtt.2009.090118. doi:10.1258/jtt.2009.090118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowles KH, Holmes JH, Ratcliffe SJ, Liberatore M, Nydick R, Naylor MD. Factors identified by experts to support decision making for post-acute referral. Nursing Research. 2009;58(2):115–122. doi: 10.1097/NNR.0b013e318199b52a. doi:10.1097/NNR.0b013e318199b52a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowles KH, Hanlon AL, Glick HA, Naylor MD, O'Connor M, Riegel B, Weiner MG. Clinical effectiveness, access to, and satisfaction with care using a telehomecare substitution intervention: A randomized controlled trial. International Journal of Telemedicine and Applications, 2011. 2011:1–13. doi: 10.1155/2011/540138. doi:10.1155/2011/540138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Medicare and Medicaid Home health prospective payment system: Payment system fact series. 2012a Retrieved from http://www.cms.gov/Outreachand-Education/Medicare-Learning-NetworkMLN/MLNProducts/downloads/HomeHlthProsPaymt.pdf.
- Centers for Medicare and Medicaid OASIS C based home health agency patient outcome, process and potentially avoidable event reports. 2012b Retrieved from https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/OASIS/09aa_hhareports.html.
- Covinsky KE, Pierluissi E, Johnston CB. Hospitalization-associated disability: “She was probably able to ambulate, but I'm not sure. Journal of the American Medical Association. 2011;306:1782–1793. doi: 10.1001/jama.2011.1556. doi:10.1001/jama.2011.1556. [DOI] [PubMed] [Google Scholar]
- Dansky KH, Vasey J, Bowles K. Impact of telehealth on clinical outcomes in patients with heart failure. Clinical Nursing Research. 2008;17:182–199. doi: 10.1177/1054773808320837. doi:10.1177/1054773808320837. [DOI] [PubMed] [Google Scholar]
- Eaton MK. The influence of a change in Medicare reimbursement on the effectiveness of stage III or greater decubitus ulcer home health nursing care. Policy, Politics, & Nursing Practice. 2005;6:39–50. doi: 10.1177/1527154404272608. doi:10.1177/1527154404272608. [DOI] [PubMed] [Google Scholar]
- Experton B, Li Z, Branch LG, Ozminkowski RJ, Mellon-Lacey DM. The impact of payor/provider type on health care use and expenditures among the frail elderly. American Journal of Public Health. 1997;87:210–216. doi: 10.2105/ajph.87.2.210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Experton B, Ozminkowski RJ, Pearlman DN, Li Z, Thompson S. How does managed care manage the frail elderly? The case of hospital readmissions in fee-for-service versus HMO systems. American Journal of Preventive Medicine. 1999;16:163–172. doi: 10.1016/s0749-3797(98)00098-1. doi:10.1016/S0749-3797(98)00098-1. [DOI] [PubMed] [Google Scholar]
- Feldman PH, Peng TR, Murtaugh CM, Kelleher C, Donelson SM, McCann ME, Putnam ME. A randomized intervention to improve heart failure outcomes in community-based home health care. Home Health Care Services Quarterly. 2004;23(1):1–23. doi: 10.1300/J027v23n01_01. doi:10.1300/J027v23n01_01. [DOI] [PubMed] [Google Scholar]
- Foster D, Harkness G. Healthcare reform: Pending changes to reimbursement for 30-day readmissions. 2010 Retrieved from http://www.communitysolutions.com/assets/2012_Institute_Presentations/acareimbuesementchanges051812.pdf.
- Han B, Remsburg RE. Impact of the Medicare Interim Payment System on length of use in home care among patients with Medicare-only payment source. Home Health Care Services Quarterly. 2005;24(4):65–79. doi: 10.1300/J027v24n04_04. doi:10.1300/J027v24n04_04. [DOI] [PubMed] [Google Scholar]
- Ho DE, Imai K, King G, Stuart EA. Matching as nonparametric preprocessing for reducing model dependence in parametric causal inference. Political Analysis. 2007;15:199–236. doi:10.1093/pan/mpl013. [Google Scholar]
- Institute of Medicine To err is human: Building a safer health system. 1999 Retrieved from http://www.iom.edu/Reports/1999/To-Err-is-Human-Building-A-Safer-Health-System.aspx.
- Institute of Medicine Crossing the quality chasm: A new health system for the 21st century. 2001 Retrieved from http://www.iom.edu/Reports/2001/Crossing-the-Quality-Chasm-A-New-Health-System-for-the-21st-Century.aspx. [PubMed]
- Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. New England Journal of Medicine. 2009;360:1418–1428. doi: 10.1056/NEJMsa0803563. doi:10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- Kleinbaum DG, Kupper LL, Nizam A, Muller KE. Applied regression analysis and other multivariate methods. Duxbury Press; California: 2008. [Google Scholar]
- Komisar HL. Rolling back Medicare home health. Health Care Financing Review. 2002;24(2):33–55. [PMC free article] [PubMed] [Google Scholar]
- Livesay JL, Hanson KS, Anderson MA, Oelschlaeger M. Client characteristics and the cost of home care in the prospective payment system. Public Health Nursing. 2003;20:287–296. doi: 10.1046/j.1525-1446.2003.20406.x. doi:10.1046/j.1525-1446.2003.20406.x. [DOI] [PubMed] [Google Scholar]
- Lum HD, Studenski SA, Degenholtz HB, Hardy SE. Early hospital readmission is a predictor of one-year mortality in community-dwelling older Medicare beneficiaries. Journal of General Internal Medicine. 2012;27:1467–1474. doi: 10.1007/s11606-012-2116-3. doi:10.1007/s11606-012-2116-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Madigan EA. Comparison of home health care outcomes and service use for patients with wound/skin diagnoses. Outcomes Management for Nursing Practice. 2001;5(2):63–67. [PubMed] [Google Scholar]
- Madigan EA. People with heart failure and home health care resource use and outcomes. Journal of Clinical Nursing. 2008;17:253–259. doi: 10.1111/j.1365-2702.2008.02334.x. doi: 10.1111/j.1365-2702.2008.02334.x. [DOI] [PubMed] [Google Scholar]
- Mandawat A, Mandawat A, Mandawat MK, Tinetti ME. Hospitalization rates and in-hospital mortality among centenarians. Archives of Internal Medicine. 2012;172:1179–1180. doi: 10.1001/archinternmed.2012.2155. doi:10.1001/archinternmed.2012.2155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCall N, Korb J. Medicare home health use after the 1997 BBA. Policy Brief. Center for Home Care Policy Research; 2003. Retrieved from http://www.vnsny.org/research/publications/pdf/no14_fact_sheet.pdf. [PubMed] [Google Scholar]
- Medicare Payment Advisory Commission Report to the Congress: Promoting greater efficiency in Medicare. 2007 Retrieved from http://medpac.gov/documents/reports/Jun07_EntireReport.pdf?sfvrsn=0.
- Medicare Payment Advisory Commission Report to the Congress: Medicare payment policy. 2010 doi: 10.3109/15360288.2010.503732. Retrieved from http://www.medpac.gov/documents/Mar10_EntireReport.pdf. [DOI] [PubMed]
- Medicare Payment Advisory Commission Report to the Congress: Medicare payment policy. 2014 Retrieved from http://medpac.gov/documents/reports/Mar10_EntireReport.pdf?sfvrsn=0.
- Murkofsky RL, Phillips RS, McCarthy EP, Davis RB, Hamel MB. Length of stay in home care before and after the 1997 Balanced Budget Act. Journal of the American Medical Association. 2003;289:2841–2848. doi: 10.1001/jama.289.21.2841. doi:10.1001/jama.289.21.2841. [DOI] [PubMed] [Google Scholar]
- Murtaugh C, Peng T, Totten A, Costello B, Moore S, Aykan H. Complexity in geriatric home healthcare. Journal for Healthcare Quality. 2009;31(2):34–43. doi: 10.1111/j.1945-1474.2009.00017.x. [DOI] [PubMed] [Google Scholar]
- Naylor MD, Aiken LH, Kurtzman ET, Olds DM, Hirschman KB. The care span: The importance of transitional care in achieving health reform. Health Affairs. 2011;30:746–754. doi: 10.1377/hlthaff.2011.0041. doi:10.1377/hlthaff.2011.0041. [DOI] [PubMed] [Google Scholar]
- Naylor MD, Brooten DA, Campbell RL, Maislin G, McCauley KM, Schwartz JS. Transitional care of older adults hospitalized with heart failure: A randomized, controlled trial. Journal of the American Geriatrics Society. 2004;52:675–684. doi: 10.1111/j.1532-5415.2004.52202.x. doi:10.1111/j.1532-5415.2004.52202.x. [DOI] [PubMed] [Google Scholar]
- Naylor MD, Stephens C, Bowles KH, Bixby MB. Cognitively impaired older adults: From hospital to home. American Journal of Nursing. 2005;105(2):52–61. doi: 10.1097/00000446-200502000-00028. [DOI] [PubMed] [Google Scholar]
- O'Connor M. Hospitalization among Medicare-reimbursed skilled home health recipients. Home Health Care Management & Practice. 2012;24(1):27–37. doi: 10.1177/1084822311419498. doi:10.1177/1084822311419498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Connor M, Davitt JK. The Outcome and Assessment Information Set (OASIS): A review of validity and reliability. Home Health Care Services Quarterly. 2012;31:267–301. doi: 10.1080/01621424.2012.703908. doi:10.1080/01621424.2012.703908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Connor M, Hanlon A, Naylor MD, Bowles KH. University of Pennsylvania, ProQuest, UMI Dissertations Publishing. 2012. Impact of length of stay and number of skilled nursing visits on hospitalization following home health discharge. 3509382. [Google Scholar]
- Office of the Federal Register Medicare and Medicaid programs; Home Health Prospective Payment System rate update for CY 2014, home health quality reporting requirements, and cost allocation of Home Health Survey expenses. 2013 Retrieved from https://www.federalregister.gov/articles/2013/12/02/2013-28457/medicare-and-medicaid-programs-home-health-prospective-payment-system-rate-update-for-cy-2014-home. [PubMed]
- Quinn C. Low-technology heart failure care in home health: Improving patient outcomes. Home Healthcare Nurse. 2006;24:533–540. doi: 10.1097/00004045-200609000-00012. [DOI] [PubMed] [Google Scholar]
- Research Data Assistance Center (ResDAC) CMS data. 2013 Retrieved from http://www.resdac.org/cms-data/search?f[0]=im_field_program_type%3A1.
- Rosenbaum PR, Rubin DB. The central role of the propensity score in observational studies for causal effects. Biometrika. 1983;70(1):41–55. [Google Scholar]
- Rosati RJ, Russell D, Peng T, Brickner C, Kurowski D, Christopher MA, Sheehan KM. Medicare home health payment reform may jeopardize access for clinically complex and socially vulnerable patients. Health Affairs. 2014;33:946–956. doi: 10.1377/hlthaff.2013.1159. doi: 10.1377/hlthaff.2013.1159. [DOI] [PubMed] [Google Scholar]
- Rubin DB. Estimating causal effects from large data sets using propensity scores. Annals of Internal Medicine. 1997;127:757–763. doi: 10.7326/0003-4819-127-8_part_2-199710151-00064. [DOI] [PubMed] [Google Scholar]
- Schade CP, Brehm JG. Improving the home health acute-care hospitalization quality measure. Health Services Research. 2010;45:712–727. doi: 10.1111/j.1475-6773.2010.01106.x. doi: 10.1111/j.1475-6773.2010.01106.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schlenker RE, Powell MC, Goodrich GK. Initial home health outcomes under prospective payment. Health Services Research. 2005;40:177–193. doi: 10.1111/j.1475-6773.2005.00348.x. doi:10.1111/j.1475-6773.2005.00348.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schlenker RE, Shaughnessy PW, Hittle DF. Patient-level cost of home health care under capitated and fee-for-service payment. Inquiry. 1995;32:252–270. [PubMed] [Google Scholar]
- Stuart EA. Matching methods for causal inference: A review and a look forward. Statistical Science. 2010;25(1):1–21. doi: 10.1214/09-STS313. doi:10.1214/09-STS313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stuart EA, Green KM. Using full matching to estimate causal effects in nonexperimental studies: Examining the relationship between adolescent marijuana use and adult outcomes. Developmental Psychology. 2008;44:395–406. doi: 10.1037/0012-1649.44.2.395. doi:10.1037/0012-1649.44.2.395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- United States General Accounting Office Medicare home health: Prospective payment health system could reverse declines in spending (GAOHEHS-00-176) 2000 Retrieved from http://www.gao.gov/archive/2000/he00176.pdf.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.