A 46 year old Caucasian female was referred to the breast center with complaints of an enlarging, tender breast mass. She had noticed the mass five days prior to presentation, and reported that it was accompanied by mild swelling and a burning sensation. On physical exam, she was noted to have a palpable abnormality in the right breast, although examination was somewhat limited by dense breast tissue bilaterally. A mammogram performed 18 months earlier was normal (Figure 1). The patient’s clinical history was notable for a diagnosis of acute myelogenous leukemia made two years earlier. She had undergone allogeneic bone marrow transplantation and was subsequently undergoing therapy for relapsed disease at the time that she noticed the breast mass. A mammogram was performed which demonstrated an area of asymmetric breast tissue in the right upper outer quadrant (Figure 2). A breast ultrasound showed a circumscribed mass in the right breast measuring 4.4 cm with heterogeneous and hypoechoic internal echotexture. A repeat ultrasound performed six weeks later showed an oval mass parallel to the skin with indistinct margins, hypoechoic echotexture, posterior acoustic shadowing, and internal vascularity. Due to these findings, an ultrasound-guided biopsy of the mass was performed.
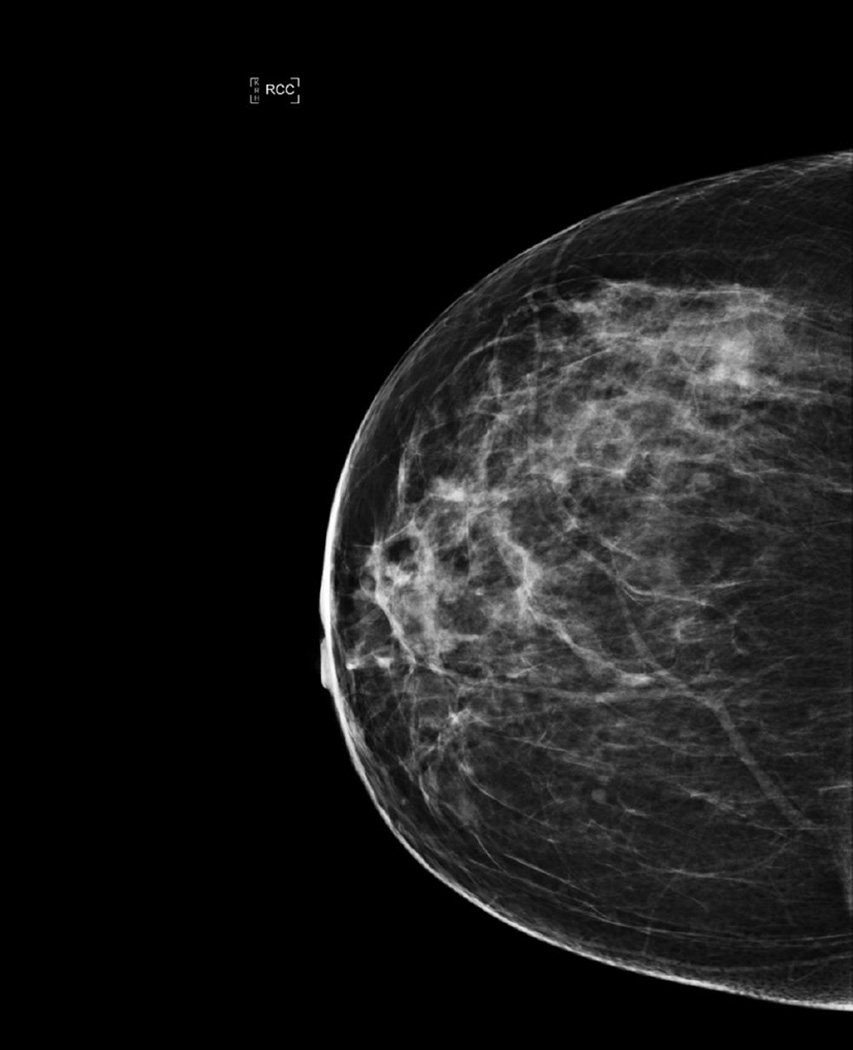
Figure 1.
Right breast mammogram, craniocaudad view: Normal on prior study.
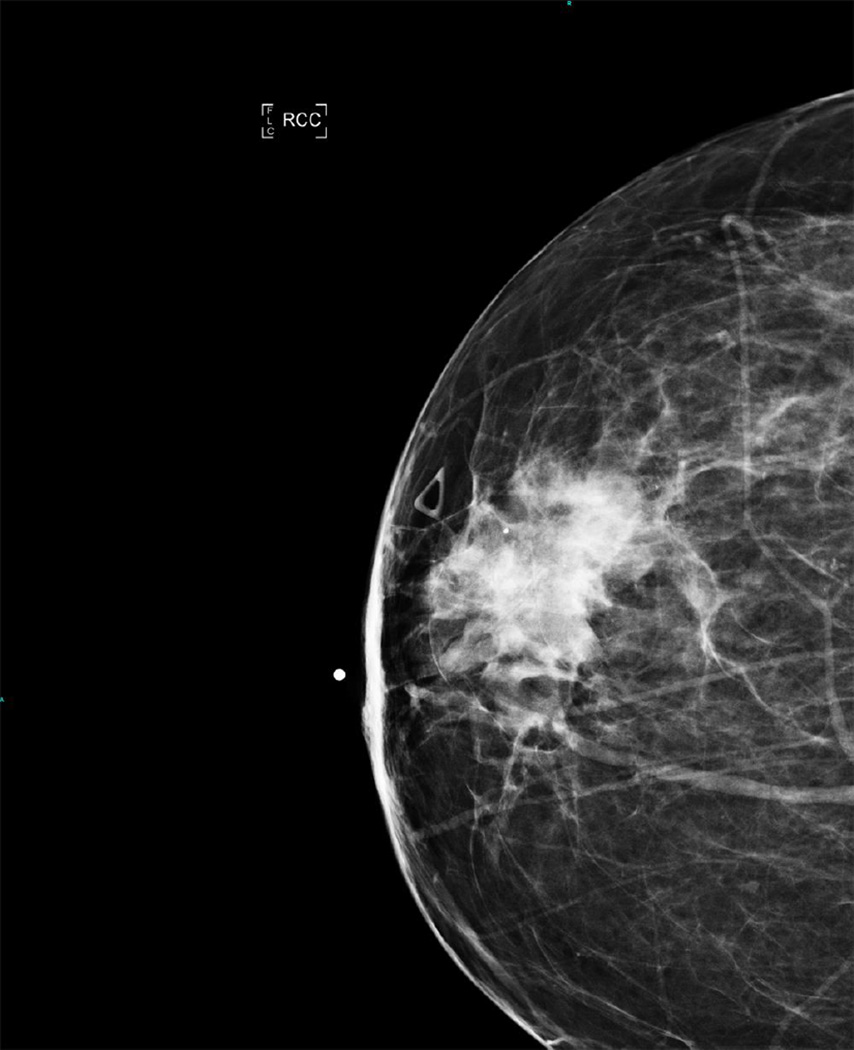
Figure 2.
Right breast mammogram, craniocaudad view, 18 months later performed for evaluation of a new rapidly enlarging right breast mass: 4.4 cm irregular mass with indistinct margins, suspicious.
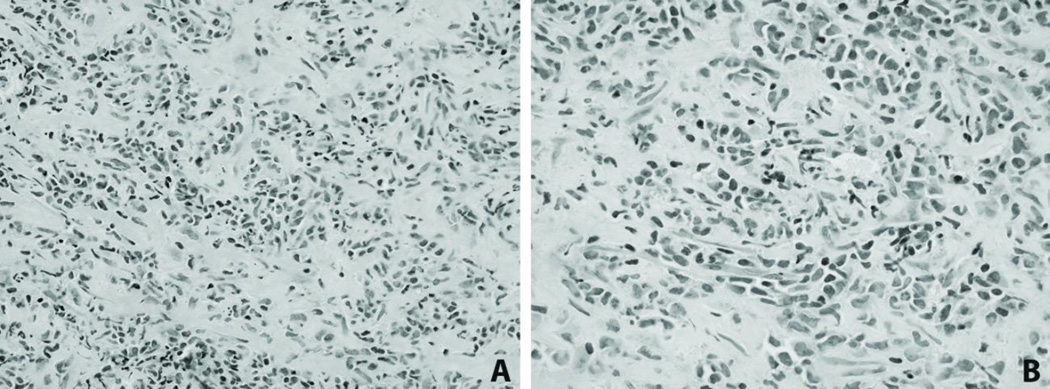
Microscopic examination revealed numerous neoplastic cells infiltrating in a single-cell pattern with some preservation of ductal and lobular structures (Figure 3). Initial immunohistochemical stains performed for ER, PR, HER2, and E-cadherin were negative. The case was initially signed out as poorly differentiated mammary carcinoma with lobular features. Subsequently, the case was reviewed and presented at breast tumor board, where the clinical history of acute myeloid leukemia was presented. Based on the unusual morphology and clinical presentation, immunohistochemical stains for pancytokeratin, myeloperoxidase, lysozyme, CD34 and CD117 were performed. Notably, the tumor cells were positive for lysozyme, CD117 and myeloperoxidase, variably positive for CD34, and negative for pancytokeratin. In addition to poorly differentiated infiltrating cells, cells with eosinophilic granules were also noted. In light of these findings, the diagnosis was revised to myeloid sarcoma.
Figure 3.
(A) Neoplastic cells infiltrating in a single cell pattern (400×), (B) High power view demonstrating intermediate to large cells with scant cytoplasm, irregular nuclei and rare scattered eosinophils (600×).
Myeloid sarcoma (granulocytic sarcoma, chloroma) is an extramedullary solid tumor usually composed of myeloid blasts with varying degrees of maturation, and is most commonly seen in patients with previously diagnosed myeloid leukemia. Myeloid sarcoma can be mistaken for invasive lobular breast carcinoma in part due to the single-cell pattern of infiltration associated with both tumor types. A clue to the diagnosis of invasive lobular carcinoma is that is should stain positively for cytokeratins, and in most cases is accompanied by positive staining for estrogen and progesterone receptors. In contrast, myeloid sarcoma is negative for cytokeratins and often strongly positive for myeloperoxidase. This case highlights the importance of appropriate clinicopathologic correlation and is a reminder to consider a broad differential diagnosis when faced with an unusual breast lesion.
Acknowledgments
Funding Statement:
This study was supported by National Institutes of Health T32 CA160003 (RLS).
Footnotes
Conflict of Interest:
The authors report no conflicts of interest.