Since the implementation of the meningococcal C conjugate vaccine as a component of the routine vaccination schedule of children in Quebec, the incidence of meningitis caused by serogroup C Neisseria meningitidis has declined significantly. Currently, serogroup B causes the majority of cases of invasive meningococcal disease in Quebec. A vaccine against serogroup B became available in 2013; accordingly, a mass vaccination campaign was launched in Saguenay–Lac-St-Jean, Quebec, in 2014. At the beginning of the campaign, a telephone survey was conducted to assess opinions on the vaccine, and willingness to be vaccinated among adolescents (16 to 18 years of age) and parents of children <16 years of age.
Keywords: 4CMenB vaccine, Adolescents, Children, Meningococcal serogroup B vaccine, Vaccine acceptability
Abstract
A mass vaccination campaign with the 4CMenB vaccine (Bexsero®; Novartis Pharmaceutical Canada Inc) was launched in a serogroup B endemic area in Quebec. A telephone survey was conducted to assess parental and adolescent opinions about the acceptability of the vaccine. Intent to receive the vaccine or vaccine receipt was reported by the majority of parents (93%) and adolescents (75%). Meningitis was perceived as being a dangerous disease by the majority of parents and adolescents. The majority of respondents also considered the 4CMenB vaccine to be safe and effective. The main reason for positive vaccination intention or behaviour was self-protection, while a negative attitude toward vaccination in general was the main reason mentioned by parents who did not intend to have their child vaccinated. Adolescents mainly reported lack of interest, time or information, and low perceived susceptibility and disease severity as the main reasons for not intending to be vaccinated or not being vaccinated.
Abstract
Une campagne de vaccination de masse avec le vaccin 4CMenB (Bexsero®; Novartis Pharma Canada Inc.) a été lancée dans une région du Québec endémique au sérogroupe B. Un sondage téléphonique afin d’évaluer l’acceptabilité du vaccin par les parents et les adolescents a été réalisé. La majorité des parents (93 %) et des adolescents (75 %) ont déclaré avoir l’intention de se faire vacciner / de faire vacciner leur enfant ou l’avoir déjà fait. La majorité des parents et des adolescents percevaient la méningite comme dangereuse et considéraient le vaccin 4CMenB comme sécuritaire et efficace. La protection de l’enfant était la principale raison d’accepter le vaccin chez les parents, tandis qu’une attitude négative envers la vaccination en général était la principale raison que donnaient les parents qui n’avaient pas l’intention de faire vacciner leur enfant. Les adolescents déclaraient surtout un manque d’intérêt, de temps ou d’information, la perception d’être peu susceptibles à la maladie et la perception que la maladie n’était pas très grave comme principales raisons de ne pas s’être fait vacciner ou de ne pas avoir l’intention de le faire.
In Canada, invasive meningococcal disease (IMD) is endemic with outbreaks caused by virulent Neisseria meningitidis clones. The incidence of IMD varies considerably depending on the different serogroups, age groups, geographical areas and time periods. Before 2005, most cases of IMD were caused by serogroup C (1). In recent years, the incidence of serogroup C disease has declined significantly due to the introduction of meningococcal C conjugate vaccine into routine immunization programs for infants, children and adolescents (2–4).
Since the widespread use of the meningococcal C conjugate vaccine, serogroup B infection now makes up the greatest proportion of reported IMD cases in Quebec (5). Between 2003 and 2010, 72% of all cases of meningococcal disease were due to serogroup B meningococci (6) and the province reported the highest incidence of serogroup B IMD across Canada. Important disparities in incidence occur among different regions in Quebec. In the area of Saguenay–Lac-St-Jean, the incidence of serogroup B IMD is seven times higher than in other areas in the province (5). Therefore, with the licensure in December 2013 of a new vaccine against meningococcal serogroup B (4CMenB, Bexsero®, Novartis Pharmaceutical Canada Inc.) (7), the Quebec Immunization Committee (CIQ) recommended vaccination of individuals from two months to 20 years of age residing in Saguenay–Lac-St-Jean to control the incidence of IMD caused by serogroup B (5). A targeted vaccination campaign was started on May 4, 2014.
In the context of the targeted mass vaccination campaign against meningococcal serogroup B disease in Saguenay–Lac-St-Jean, the objective of the present study was to assess the knowledge, attitudes and intention of parents of eligible children and of adolescents targeted to receive the 4CMenB vaccine over time. The present article describes the first phase of the study.
METHODS
Study design
The first phase of the present longitudinal study was conducted at the beginning of the mass vaccination campaign to assess the determinants of parents’ intention to have their child vaccinated with the 4CMenB vaccine (or adolescents’ intention to receive the 4CMenB vaccine). A professional research and polling firm (SOM Recherches et Sondages) handled recruitment and data collection. Computer-assisted telephone interviews were performed from May 9 to May 17, 2014. The sample was constituted using random-digit dialling methodology (8). The households and potential respondent in the household were both randomly selected. When the selected person was <16 years of age, the person in charge of health decisions for the selected child responded to the survey questionnaire, while participants ≥16 years of age answered for themselves. Eligibility criteria were: to be either the main caregiver of at least one child between two months and 15 years of age or between 16 and 20 years of age; and to live or study in Saguenay–Lac-St-Jean at the time of the survey. To participate, respondents had to be able to answer a French questionnaire. The target was to enroll 875 respondents to provide a precision of ±5% for the most conservative variable estimation.
The study was evaluated positively with regard to its methodology by the Ethics Review Board (ERB) of the CHU de Québec, but was exempted from complete evaluation by the ERB due to article 2.5 of the Tri-Council Policy Statement on Ethical Conduct for Research Involving Humans in Canada (9). Before beginning the interview, respondents were informed about the objectives and the sponsors of the survey, and verbal consent was obtained.
Survey instrument
The survey instrument was developed only in French and included questions to measure the respondents’ knowledge and attitudes about IMD and the 4CMenB vaccine as well as the respondents’ intention to have their child vaccinated (or, for adolescents, to be vaccinated themselves) and main reasons for intending or not intending to receive the 4CMenB vaccine. Most of the questions used a four-point Likert scale ranging from “totally agree” to “totally disagree”. Open-ended questions were used to collect reasons for vaccinating or not vaccinating. The survey questionnaire was developed based on questions used in similar studies (10–12). Before initiation of the study, the survey was reviewed by public health practitioners, physicians and nurses involved in the mass campaign for content validity. Questions perceived to be ambiguous were modified or removed. The survey questionnaire was also pretested with 10 respondents and additional clarifications were made in the wording of some questions. Standard sociodemographic variables were collected (for parents: age, level of education as well as age and sex of the child; for adolescents: main occupation, level of education). The survey instrument is available on request.
Data analysis
Expansion weights were assigned to ensure that the results were representative of the target population by adjusting for disproportionate sampling and nonresponse bias. Weighting included a calibration that was applied to each respondent in the sample, based on sociodemographic characteristics drawn from the data contained in the Quebec immunization registry developed specifically for the campaign as well as from census data.
Descriptive statistics were generated for all variables. For each estimate, 95% CIs were calculated. Comparison between respondent groups according to demographic characteristics (age and sex of the child, level of parents’ education, etc) were performed using χ2 or Fisher’s exact tests as appropriate. Beliefs and attitudes about meningococcal B vaccination were analyzed to explore the associated factors with vaccination intention. Percent of agreement was dichotomized in agree (totally agree, somewhat agree) versus disagree (somewhat disagree and totally disagree). A multivariate logistic regression model was used to determine variables independently associated with the adolescent’s intention not to be vaccinated with the 4CMenB. Dependent and explanatory variables were dichotomized. The verbatim wording of the open-ended questions was transcribed by the interviewers and submitted to content analysis. Qualitative data were organized into main coded themes and concepts belonging to a similar theme were regrouped. These themes were updated and revised until no new properties, dimensions or relationships emerged during analysis. This content analysis was first performed using Word processing software and then imported into SAS version 9.3 (SAS Institute, USA) when completed. All statistical analyses were performed using SAS version 9.3. All tests were considered to be statistically significant at the threshold of 5% (P<0.05).
RESULTS
The response rate was 72% and 887 interviews were completed (703 interviews with parents of children between two months and 16 years of age and 184 with adolescents ≥16 years of age). More than one-half of parents were between 30 and 39 years of age (54%). Almost two-thirds of parents had a university (32%) or collegial degree (31%). Almost all adolescents were in school. The majority of parents reported that their child had received all recommended vaccines (92%), whereas 66% of adolescents reported this. Less than 1% of parents and adolescents mentioned not receiving any vaccine (Table 1). A higher proportion of parents of children five to 12 years of age reported that their child was fully vaccinated compared with parents of children <5 years of age or >12 years of age.
TABLE 1.
Parents’ and adolescents’ self-reported vaccine status
| All recommended vaccines | Some vaccines only | No vaccine | Do not know | |
|---|---|---|---|---|
| Parents of children: | ||||
| 2 months to <5 years of age | 88.3 (84.42–92.17) | 9.5 (6.00–13.02) | 1.7 (0.00–3.42) | 0.5 (0.00–1.17) |
| 5 years to <12 years of age | 96.2 (93.45–98.90) | 3.6 (0.91–6.29) | 0.2 (0.00–0.67) | 0.0 |
| 12 years to <16 years of age | 91.2 (86.62–95.86) | 7.9 (3.54–12.17) | 0.0 | 0.9 (0.00–2.69) |
| Total (parents) | 92.5 (90.40–94.53) | 6.5 (4.58–8.46) | 0.6 (0.06–1.21) | 0.4 (0.00–0.87) |
| Adolescents | 65.8 (57.98–73.64) | 29.0 (21.56–36.52) | 0.7 (0.00–2.19) | 4.4 (0.93–7.89) |
Data presented as % (95% CI)
Overall, most parents (99%) and adolescents (90%) knew that a vaccination campaign against meningitis was launched in their region. Among adolescents, more girls than boys were aware of the campaign (98% versus 83%; P=0.0001). The majority of parents (93%) intended to have their child vaccinated with the 4CMenB vaccine or had already done so (Table 2).A higher proportion of parents of children <5 years of age did not know whether they would have their child vaccinated with the 4CMenB vaccine. Approximately 75% of adolescents also intended to be vaccinated or had received the 4CMenB vaccine (Table 2). A positive association between self-reported complete vaccination status for other recommended vaccines and intention to receive the 4CMenB vaccine (or being already vaccinated) was observed, for both parents and adolescents.
TABLE 2.
Intention to receive the 4CMenB vaccine
| Intend to receive | Do not intend to receive | Vaccinated with 4CMenB vaccine | Do not know | |
|---|---|---|---|---|
| Parents of children: | ||||
| 2 months to <5 years of age | 54.9 (48.98–60.78) | 3.4 (1.11–5.72) | 34.9 (29.29–40.46) | 6.8 (3.63–10.03) |
| 5 years to <12 years of age | 90.3 (85.85–94.78) | 4.3 (1.18–7.38) | 4.5 (1.32–7.69) | 0.9 (0.00–2.15) |
| 12 years to <16 years of age | 91.8 (87.56–96.13) | 1.5 (0.00–3.09) | 2.1 (0.00–4.26) | 4.5 (1.07–7.99) |
| Total (parents) | 79.5 (76.42–82.67) | 3.3 (1.74–4.90) | 13.5 (10.96–15.97) | 3.7 (2.22–5.11) |
| Adolescents | 50.7 (42.50–58.97) | 22.1 (15.12–29.00) | 22.4 (15.64–29.21) | 4.8 (1.23–8.33) |
Data presented as % (95% CI)
The main reason cited by parents for intending to have or having had their child vaccinated with the 4CMenB vaccine was to protect him/her against meningitis. The desire to be protected against meningitis was also the main reason stated by adolescents who intended to receive or had received the vaccine. General trust in vaccines, the perception that the benefits of the 4CMenB outweighed the risks, and knowing someone who suffered from meningitis were others reasons for vaccination reported by parents and adolescents. In addition, some adolescents indicated ease of access to the 4CMenB vaccine and that it was free as reasons for intending to be or being vaccinated. The most frequent reason mentioned by parents who did not intend to have their child vaccinated was opposition to vaccination in general. For adolescents, lack of interest, time or information about the vaccine and low perceived susceptibility to infection and perceived low disease severity were the main reasons cited by adolescents who did not intend to be vaccinated.
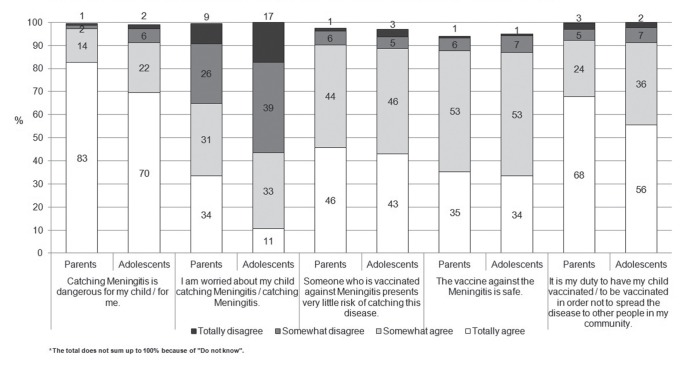
The results of questions assessing respondents’ knowledge, beliefs and attitudes regarding IMD and the 4CMenB vaccine are illustrated in Figure 1. Generally, the majority of respondents considered IMD to be a severe disease and were worried about their own or their child’s susceptibility to it. Most respondents also perceived 4CMenB vaccine to be safe and effective. Five percent of adolescents and 6% of parents answered “I don’t know” to the question about the vaccine’s safety. More than 90% of respondents also considered that it was their duty to receive the vaccine or to vaccinate their child to prevent the transmission of meningitis to others in their community.
Figure 1).
Parents’ and adolescents’ knowledge, attitudes and beliefs regarding invasive meningococcal disease and the 4CMenB vaccine*
Parents who were less educated (high school diploma or less) were more worried that their child could contract meningitis when compared with parents with a college or university degree (78%, 62% and 57%, respectively, P<0.0001). In addition, among adolescents, more girls than boys were worried about the risk of contracting meningitis (57% versus 29%, P=0.0002).
Because almost all parents intended to have or had their child vaccinated, it was not possible to perform multivariate analyses. However, a multivariate regression analysis was performed to identify the factors associated with adolescents’ intention not to be vaccinated. The results of this multivariate analysis are presented in Table 3. Not being aware of the vaccination campaign, believing that the 4CMenB was not safe and not believing that it was a duty to be vaccinated to prevent the spread of infection in the community were associated with the intention not to be vaccinated with the 4CMenB vaccine.
TABLE 3.
Factors associated with adolescents’ intention not to receive the 4CMenB vaccine
| Adjusted OR* | 95% CI | P | |
|---|---|---|---|
| Have you heard about a vaccination campaign against meningitis that is ongoing in your region? (No) | 18.45 | 4.79–71.13 | <0.0001 |
| Catching meningitis is dangerous for me (Disagree) | 1.72 | 0.35–8.45 | 0.5045 |
| I am worried about catching meningitis (Disagree) | 2.91 | 0.95–8.92 | 0.0617 |
| Someone who is vaccinated against meningitis presents very little risk of catching this disease (Disagree) | 1.20 | 0.16–8.90 | 0.8561 |
| The vaccine against meningitis is safe (Disagree) | 25.17 | 5.13–123.46 | <0.0001 |
| It is my duty to be vaccinated in order not to spread the disease to other people in my community (Disagree) | 9.41 | 2.11–42.09 | 0.0033 |
Adjusted OR with all items in the model.
DISCUSSION
Results of the first phase of our study indicated that the majority of respondents were aware of the mass vaccination campaign against meningococcal serogroup B disease that was going on in Saguenay– Lac-St-Jean. This is not surprising given that the survey was conducted two weeks after the official announcement of the campaign, which was highly publicized in local media (13–16).
Our results illustrated a high willingness to receive the new 4CMenB in the context of a targeted mass campaign. More than nine of 10 parents indicated an intention to have their child vaccinated or had already done so. Almost three of four adolescents surveyed indicated an intention to receive the vaccine or had received it. As in other studies, our results indicate a strong association between having received all recommended vaccines and intending to receive the new vaccine (17,18).
Our results mirror findings from prelicensure trials that showed a high level of acceptability for the vaccine (17–26). Because it can arise in an unpredictable manner, develop rapidly and lead to serious consequences, meningitis has characteristics that increase the population’s perception of risk (27). Meningitis was perceived as being a dangerous disease by the majority of parents and adolescents surveyed. The death due to serogroup B meningitis of a 16-year-old adolescent living in Saguenay–Lac-St-Jean in spring 2014, before the launch of the campaign, was covered extensively by the media and has probably contributed to the perceived risk of the disease in the public (28–30). In fact, approximately two-thirds of parents reported that they were worried about the risk for their child contracting the disease. Although adolescents between 15 and 20 years of age have high rates of IMD (31), fewer adolescents were concerned about their own risk for contracting meningitis.
Different studies have shown that new vaccines are likely to engender doubts and concerns (17,32,33). For instance, in a recent pan-Canadian survey, one-half of the parents were concerned that new vaccines are not as safe as older vaccines, and one-third believed that children today receive too many vaccines (34). The fact that the 4CMenB vaccine is new did not have an important influence on its acceptability by parents and adolescents in our study. A minority of respondents have cited the novelty of the vaccine as a reason for not intending to be vaccinated. In the particular context of an endemic situation, the perceived threat of the disease may outweigh the perceived risks associated with new vaccines (35,36).
Clinical trials showed the 4CMenB vaccine to be more reactogenic than vaccines routinely used in Quebec, which we hypothesized could have a negative impact on its acceptability (37,38). We anticipated that (real or perceived) side effects after the first dose, such as pain and fever, could compromise the acceptability of the subsequent doses and even have a negative impact on the acceptability of other routine vaccines (39–42). For instance, the results of one study on vaccination against seasonal influenza highlighted the reduced acceptability of a second dose of the vaccine on the basis of the severity of side effects perceived by parents after the first dose (39). The second phase of our study will provide additional information on this issue.
The present study had both strengths and limitations. The response rate of 72% is well above rates typically obtained with telephone surveys (43,44). Other strengths of the present study were the use of random-digit dialling methodology for data collection and the use of case-weights to adjust for disproportionate sampling and non-response bias. However, similar to most surveys, we cannot exclude the potential of socially desirable responses, which is the tendency of respondents to reply in a manner that will be viewed favourably by others. The survey was conducted only in French; however, <1% of the contacted households did not participate due to a language barrier. We used a telephone survey, which resulted in a recruitment bias toward more educated individuals and against the young and new residents of a community with no household telephone number (43). However, it is known that in Quebec most families with young children are residents of the same community for several years and most of them have a household telephone number. In 2013, 89% of Quebecers households with children reported using a landline telephone (45). Finally, because of the gap between intention and behaviour (46,47), our findings are limited by the fact that our survey was conducted at the beginning of the campaign. To conclude, the first phase of the present study has indicated high acceptance of the new 4CMenB vaccine at the beginning of the mass campaign in Saguenay–Lac-St-Jean. Intention to receive the vaccine was high, as was perceived severity and susceptibility of the disease. The second phase of the study, which will be conducted in March and April 2015, after the end of the campaign, will provide additional information on the determinants of acceptance of the vaccine. It will then be possible to describe the determinants for having received one, all or none of the recommended doses of the 4CMenB vaccine. We will also be able to assess the potential impact of adverse events after the first dose (real or perceived) on the acceptability of the subsequent doses and of other scheduled vaccines.
Acknowledgments
This study was financially supported by Quebec Ministry of Health. The authors thank Zhou Zhou and Laurie Costa, CHU de Québec Research Center, for their assistance with data analysis.
REFERENCES
- 1.Sadarangani M, Scheifele DW, Halperin SA, et al. The impact of the meningococcal serogroup C conjugate vaccine in Canada between 2002 and 2012. Clin Infect Dis. 2014;59:1208–15. doi: 10.1093/cid/ciu597. [DOI] [PubMed] [Google Scholar]
- 2.Bettinger JA, Scheifele DW, Halperin SA, et al. Evaluation of meningococcal serogroup C conjugate vaccine programs in Canadian children: Interim analysis. Vaccine. 2012;30:4023–7. doi: 10.1016/j.vaccine.2012.04.034. [DOI] [PubMed] [Google Scholar]
- 3.Halperin SA, Bettinger JA, Greenwood B, et al. The changing and dynamic epidemiology of meningococcal disease. Vaccine. 2012;30(Suppl 2):B26–36. doi: 10.1016/j.vaccine.2011.12.032. [DOI] [PubMed] [Google Scholar]
- 4.De Wals P. Analysis of mortality following a mass immunization campaign with serogroup C meningococcal conjugate vaccine. Vaccine. 2009;27:5730. doi: 10.1016/j.vaccine.2009.07.041. [DOI] [PubMed] [Google Scholar]
- 5.De Wals P, Deceuninck G, Dubé E, et al. Avis sur la pertinence d’une intervention visant à contrôler une incidence élevée d’infections invasives à méningocoque de sérogroupe B dans l’Est du Québec. Québec: Institut national de santé publique du Québec; Mar, 2014. [Google Scholar]
- 6.Zhou J, Lefebvre B, Deng S, et al. Invasive serogroup B Neisseria meningitidis in Quebec, Canada, 2003–2010: Persistence of the ST-269 clone since it first emerged in 2003. J Clin Microbiol. 2012;50:1545–51. doi: 10.1128/JCM.06835-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Novartis Pharmaceutical Canada Inc. BEXSERO® Multicomponent Meningococcal B Vaccine (recombinant, absorbed). Québec: Novartis Pharmaceutical Canada Inc; Dec 6, 2013. [Google Scholar]
- 8.Brick JM. Random-digit dialing (RDD) In: Lavrakas P, editor. Encyclopedia of Survey Research Methods. Thousand Oaks: SAGE Publications Inc; 2008. pp. 676–9. [Google Scholar]
- 9.Canadian Institute of Health Research, Natural Sciences and Engineering Research Council of Canada and Social Sciences and Humanities Research Ethics Special Working Committee. Tri-Council Policy Statement: Ethical Conduct for Research Involving Humans. Dec, 2014.
- 10.Krawczyk A, Knauper B, Gilca V, et al. Parents’ decision-making about the human papillomavirus vaccine for their daughters: I. Quantitative results. Hum Vaccin Immunother. 2015;11:330–6. doi: 10.1080/21645515.2014.1004030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dube E, Bettinger JA, Halperin B, et al. Determinants of parents’ decision to vaccinate their children against rotavirus: Results of a longitudinal study. Health Educ Res. 2012;27:1069–80. doi: 10.1093/her/cys088. [DOI] [PubMed] [Google Scholar]
- 12.Dube E, De Wals P, Gilca V, et al. New vaccines offering a larger spectrum of protection against acute otitis media: Will parents be willing to have their children immunized? Int J Pediatr Otorhinolaryngol. 2009;73:987–91. doi: 10.1016/j.ijporl.2009.03.022. [DOI] [PubMed] [Google Scholar]
- 13.Thibeault J. Campagne de vaccination massive dans la région. InfoSaguenay. 2014 Apr 23; [Google Scholar]
- 14.La Haye J. La campagne de vaccination contre le méningocoque débutera le 5 mai. Journal L’Étoile du Lac. 2014 Apr 28; [Google Scholar]
- 15.Girard C. Campagne de vaccination contre le méningocoque de type B. Le Courrier du Saguenay. 2014 Apr 22; [Google Scholar]
- 16.Savoie-Soulières M. Vaste campagne de vaccination contre la méningite de type B. Radio Canada. 2014 Apr 22; [Google Scholar]
- 17.Bedford H, Lansley M. More vaccines for children? Parents’ views. Vaccine. 2007;25:7818–23. doi: 10.1016/j.vaccine.2007.08.057. [DOI] [PubMed] [Google Scholar]
- 18.Marshall H, Clarke M, Sullivan T. Parental and community acceptance of the benefits and risks associated with meningococcal B vaccines. Vaccine. 2013;32:338–44. doi: 10.1016/j.vaccine.2013.11.042. [DOI] [PubMed] [Google Scholar]
- 19.CBG Health Research Limited Evaluation of meningococcal B immunisation national roll-out. 2006. < www.health.govt.nz/system/files/documents/publications/menzb-implementation-evaluation-nov06.pdf> (Accessed April 7, 2014).
- 20.Watson PB, Yarwood J, Chenery K. Meningococcal B: Tell me everything you know and everything you don’t know. New Zealanders’ decision-making regarding an immunisation programme. N Z Med J. 2007;120:U2751. [PubMed] [Google Scholar]
- 21.Bland M, Clear GM, Grogan A, Hoare K, Waldock J. Mum’s the word: Factors that influenced young adults’ participation in the New Zealand Meningococcal B immunisation programme. N Z Med J. 2009;122:30–8. [PubMed] [Google Scholar]
- 22.Bakhache P, Rodrigo C, Davie S, et al. Health care providers’ and parents’ attitudes toward administration of new infant vaccines – a multinational survey. Eur J Pediatr. 2013;172:485–92. doi: 10.1007/s00431-012-1904-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dubé E, Defay F, Sauvageau C, Lavoie F, Gilca V. Priorités en vaccination chez les professionnels de la santé du Québec. Données non publiées. 2010.
- 24.Cohen R, Levy C, Bechet S, Elbez A, Corrard F. How pediatricians and GP consider the implementation of meningococal B vaccination in France? Arch Pediatr. 2012;19:1379–85. doi: 10.1016/j.arcped.2012.10.001. [DOI] [PubMed] [Google Scholar]
- 25.Fisher W, Bettinger J, Gilca V, et al. Understanding parental acceptance of a novel meningococcal serogroup B vaccine for infants.. Milan. 31st Annual Meeting of the European Society for Paediatric Infectious Diseases; May 28 to June 1, 2013. [Google Scholar]
- 26.Rodrigo C, Bakhache P, Rose M, et al. Parental awareness and knowledge about invasive meningococcal disease: Results of a multinational survey.. 30th Annual Meeting of the European Society For Paediatric Infectious Diseases;; May 8 to 12; Thessaloniki, Greece. 2012. [Google Scholar]
- 27.Slovic P. Perception of risk. Science. 1987;236:280–5. doi: 10.1126/science.3563507. [DOI] [PubMed] [Google Scholar]
- 28.Lavoie S. Un ado de 16 ans succombe à la méningite. TVA Nouvelles. 2014 Feb 24; [Google Scholar]
- 29.Bégin S. Terassé par la méningite. La Presse. 2014 Feb 24; [Google Scholar]
- 30.Radio Canada. Cas mortel de méningite. Radio Canada; Feb 23, 2014. [Google Scholar]
- 31.Gilca R, Deceuninck G, Lefebvre B, et al. The changing epidemiology of meningococcal disease in Quebec, Canada, 1991–2011: Potential implications of emergence of new strains. PLoS One. 2012;7:e50659. doi: 10.1371/journal.pone.0050659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gust DA, Darling N, Kennedy A, Schwartz B. Parents with doubts about vaccines: Which vaccines and reasons why. Pediatrics. 2008;122:718–25. doi: 10.1542/peds.2007-0538. [DOI] [PubMed] [Google Scholar]
- 33.Freed GL, Clark SJ, Butchart AT, Singer DC, Davis MM. Parental vaccine safety concerns in 2009. Pediatrics. 2010;125:654–9. doi: 10.1542/peds.2009-1962. [DOI] [PubMed] [Google Scholar]
- 34.Ekos Research Associates Inc. Survey of Parents on Key Issues Related to Immunization. Ottawa: Public Health Agency of Canada; Sep, 2011. [Google Scholar]
- 35.Chen RT, DeStefano F, Pless R, et al. Challenges and controversies in immunzation safety. Infect Dis Clin North Am. 2001;15:21–39. doi: 10.1016/s0891-5520(05)70266-x. [DOI] [PubMed] [Google Scholar]
- 36.Chen RT, Rastogi SC, Mullen JR, et al. The Vaccine Adverse Event Reporting System (VAERS) Vaccine. 1994;12:542–50. doi: 10.1016/0264-410x(94)90315-8. [DOI] [PubMed] [Google Scholar]
- 37.Robinson JL. La vaccination contre le méningocoque du sérogroupe B : ce que le praticien doit savoir. Paediatr Child Health. 2014;19:95–8. [Google Scholar]
- 38.European Medicines Agency. European public assessment report for Bexsero. < ema.europa.eu/Find_medicine/Human Medicines/European public assessment reports> (Accessed April 12, 2013).
- 39.Broos N, van Puijenbroek EP, van Grootheest K. Fever following immunization with influenza A(H1N1) vaccine in children. Drug Saf. 2010;33:1109–15. doi: 10.2165/11539280-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 40.Mak DB, Carcione D, Joyce S, Tomlin S, Effler PV. Paediatric influenza vaccination program suspension: Effect on childhood vaccine uptake. Aust N Z J Public Health. 2012;36:494–5. doi: 10.1111/j.1753-6405.2012.00925.x. [DOI] [PubMed] [Google Scholar]
- 41.Parrella A, Gold M, Marshall H, et al. Parental views on vaccine safety and future vaccinations of children who experiences an adverse event following routine of seasonal influenza vaccination in 2010. Hum Vaccin Immunother. 2012;8:662–7. doi: 10.4161/hv.19478. [DOI] [PubMed] [Google Scholar]
- 42.Flood EM, Ryan KJ, Rousculp MD, et al. Parent preferences for pediatric influenza vaccine attributes. Clin Pediatr (Phila) 2011;50:338–47. doi: 10.1177/0009922810391247. [DOI] [PubMed] [Google Scholar]
- 43.Dillman DA, Smyth JD, Christian LM, editors. Internet, mail, and mixed-mode surveys – The tailored design method. 3rd edn. Hoboken: John Wiley & Sons; 2009. [Google Scholar]
- 44.Environics Research Group. Canadian Adult National Immunization Coverage (NICS) Survey – 2010 – Québec. Ottawa: ministère de la Santé et des Services sociaux du Québec; Feb, 2011. [Google Scholar]
- 45.CEFRIO. NETendances 2013 – Les modes de communication au Québec à travers les génération. 2013.
- 46.Webb TL, Sheeran P. Does changing behavioral intentions engender behavior change? A meta-analysis of the experimental evidence. Psychol Bull. 2006;132:249–68. doi: 10.1037/0033-2909.132.2.249. [DOI] [PubMed] [Google Scholar]
- 47.Sheeran P. Intention-behavior relations: A conceptual and empirical review. Eur Rev Soc Psychol. 2002;12:1–36. [Google Scholar]