Abstract
Background: To assess the diagnostic value of decreased parathyroid hormone (PTH) in hypoparathyroidism after unilateral operation. Methods: A study was conducted on patients with PTC undergoing total or near-total thyroidectomy plus central neck dissection (CND). Results: Postoperative hypocalcemia was found in 42 patients (51.2%). For patients undergoing bilateral CND, those whose tumor invasion proceeded beyond the thyroid capsule have a higher rate of postoperative hypoparathyroidism (P<0.05). PTH level of hypoparathyroidism patients was lower than that of non-hypoparathyroidism patients from surgery to 6 months later (P<0.05). When unilateral thyroidectomy and central region dissection were completed, PTH level decreased by 47.06% in hypoparathyroidism patients, which was significantly higher than non-hypoparathyroidism patients (28.35%) (P<0.001). PTH level (AUC 0.806) and its decreasing degree (AUC 0.736) played predicting roles in assessing postoperative hypoparathyroidism (P<0.001). Conclusions: For PTC surgery, PTH level and its decreasing degree played predicting roles in assessing postoperative hypoparathyroidism.
Keywords: Papillary thyroid carcinoma, parathyroid hormone, hypoparathyroidism, operation, predictor
Introduction
Management of papillary thyroid carcinoma (PTC) varies in different parts of the world with quite different approaches. The extent of surgery for patients with PTC has been actively debated for decades, fueled by the prolonged long-term survival and the possibility of higher complication rates with more extensive operations. Total or near-total thyroidectomy is the main surgical method in most western countries [1]. In Asian countries, however, total or near-total thyroidectomy is not the prior choice [2]. For example, ATA guideline recommended total or near-total thyroidectomy for >1 cm unilateral thyroid carcinoma. In China, however, the guideline recommended total or near-total thyroidectomy for >4 cm unilateral thyroid carcinoma, and lobectomy for <1 cm unilateral thyroid carcinoma; if tumor size was between 1 cm-4 cm, both the surgical methods above could be applied [3]. Similarly, it is also controversy regarding to the indications for central neck dissection (CND). Some researchers thought that preventive CND could clear concealed metastasis, which would benefit the tumor classification and the follow-up of tumor markers. However, others argued that no long-term prospective studies confirming the impact of CND on recurrence and death rate [4].
Undoubtedly, large extent surgery will get the tumor resected more, but it may increase the complication rate. A study of over 50,000 patients with PTC found that total thyroidectomy significantly improved recurrence and survival rate for tumors >1.0 cm on multivariate analysis, so they suggested total thyroidectomy for >1 cm. however, the 10-year survival rate was 98.4% for total thyroidectomy and 97.1% for lobectomy, so they also pointed out that the modest outcome benefit must be weighed cautiously against the potential complications after total thyroidectomy [5]. Additionally, surgeon’s experience was highly correlated with the complications, but 86% PTC surgeries were not operated by experts [6]. For patients undergoing thyroid surgery in the United States, 50% of them were operated by surgeons who performed fewer than five thyroidectomies every year [7]. Thus, it is important to emphasize that the extent of thyroidectomy should be tailored not only to the patient’s risk group and operative findings, but also to the progress of the specific surgery, particularly if the contralateral lobe is not involved by cancer. If unilateral thyroidectomy was completed without injuring recurrent laryngeal nerves and parathyroid glands, then contralateral thyroid surgery can be safely contemplated. If the first side has not gone well, elective contralateral lobe resection and CND should be deferred because of the potential occurrence of recurrent laryngeal nerve paralysis and permanent hypothyroidism. Intraoperative nerve lesions can be detected by monitoring instruments, but intraoperative assessment of hypoparathyroidism is a great challenge [8].
Most of studies predicted postoperative hypocalcemia by detecting PTH level, because half-life period of PTH was only 2-6 minutes and it was convenient to detect [9]. PTH levels can be used to implement early treatment with calcium and/or vitamin D supplements to reduce the incidence and severity of hypocalcemia [10]. Progressive and severe hypocalcemia is unlikely in the setting of a normal PTH level and hence PTH can be used cautiously to facilitate discharge early for many patients [11]. It is worth mentioning that intraoperative PTH monitoring is a useful surgical adjunct during parathyroidectomy for the treatment of sporadic primary hyperparathyroidism [12]. If PTH decreases by over 50% after parathyroid gland resection, the operation is deemed a success without detecting other parathyroid glands. This surgical adjunct has helped to change the operative approach to parathyroidectomy from the traditional bilateral neck exploration with visualization of all parathyroids to a minimally invasive uniglandular parathyroidectomy with removal of only the hypersecreting gland (s), preserving all normally functioning tissue [13].
Therefore, we assumed that PTH changes could predict the ipsilateral parathyroid gland function after unilateral thyroidectomy. The presented prospective study aimed to investigate the correlations of hypoparathyroidism with intraoperative PTH change and its decreased extent.
Materials and methods
General information
Eighty-eight patients pathologically diagnosed as PTC were initially enrolled in Department of Head and Neck Surgery of Zhejiang cancer hospital from Jan to Dec 2013. We conducted total or near-total thyroidectomy based on CTA guideline. Patients with clinical evidence of parathyroid disease or a history of neck surgery were excluded. Preoperative PTH, serum calcium, and magnesium were in normal ranges. 2 cases were excluded because of wrong blood extraction time; another 3 cases did not complete the laboratory examinations; 1 case was lost in the follow-up; and finally 82 cases were included in the study. The study was approved by our institutional review board, and informed consent was obtained from all participants.
Surgical methods
All participants underwent total or near-total thyroidectomy; if patients were found unilateral thyroid carcinoma, they would underwent ipsilateral CND, and if they were found contralateral suspected lymph nodes, whey would underwent bilateral CND; FNAC-confirmed lateral neck metastases underwent lateral neck dissection; The parathyroid glands were carefully preserved, and the devascularized parathyroid glands were transplanted into the sternocleidomastoid muscle. Autotransplantation of the parathyroid glands was not routinely performed.
Laboratory examinations
In all patients, peripheral blood was drawn intraoperatively from at the following time points: 1) before the skin incision is made (PTH0); 2) 10 minutes after lobectomy and ipsilateral CND (PTHi); 3) 10 minutes after the end of bilateral operation (PTHb). Contralateral thyroidectomy was conducted only after PTHi blood samples were extracted.
Serum calcium, magnesium, inorganic phosphorus, albumin, and PTH levels were assayed daily until patients were discharged. To perform all required blood tests, this study protocol required hospitalization of all patients for a minimum of 4 days after surgery. All patients were followed up at 1, 3, 6 months after surgery, at which time serum calcium and iPTH levels were measured.
Normal values in our laboratory ranged from 15 to 65 ng/L for PTH, 2.00 to 2.60 mmol/L (8.0 to 10.5 mg/dl) for calcium, 0.70 to 1.10 mmol/L for magnesium, 0.80 to 1.45 mmol/L for inorganic phosphorus, and 3.5 to 5.0 g/dl for albumin. The serum calcium value was corrected for albumin levels with the use of the following formula: corrected calcium = serum calcium + 0.8 (4.0-serum albumin). Postoperative hypoparathyroidism was defined by postoperative albumin-adjusted sCa levels of less than 1.9 mmol/L with or without clinical symptoms of hypocalcemia (such as perioralnumbness, paraesthesias of the extremities, or a positive Trousseau sign) or subnormal sCa levels (1.9-2.0 mmol/L) with neuromuscular symptoms during the first 4 postoperative days. Permanent hypocalcemia is defined as those who require continued calcium and vitamin D supplementation at 6 months postoperatively.
Hypocalcemic patients started replacement therapy with intravenous or oral calcium combined with oral vitamin D, depending on the severity of hypocalcemia. Abnormal magnesium levels were corrected immediately upon detection.
Statistical analysis
Statistical analysis was performed using SPSS 13.0 (SPSS Inc, Chicago, IL, USA). Student’s t test was used to compare continuous variables with normal distribution. Tests of association of categorical variables were performed using chi-square test or Fisher’s exact test. Statistical tests were two-sided at the 5% level of significance. Sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV) were calculated by a 2×2 contingency table. ROC was used to assess the diagnostic value of PTH in predicting hypoparathyroidism.
Results
Of 82 patients, there were 67 (81.7%) women and 15 (18.3%) men with a mean age of 44.7 years (range 10-70 years). All participants underwent total or near-total thyroidectomy, among which 36 cases (43.9%) underwent unilateral CND; 46 cases (56.1%) underwent bilateral CND, 23 cases (28.0%) underwent lateral neck dissection (11 unilateral cases, 12 bilateral cases). A total of 11 single-gland and 4 two-gland autotransplantation were performed. Based on TNM classification, there were 58 (70.7%) cases in stage I, 1 case in stage II (1.2%), 14 cases in stage III (17.1%), and 9 cases in stage IV (11.0%). Postoperative pathological biopsy showed 33 cases of unilateral PTC (40.2%), 49 cases bilateral PTC (59.8%), 45 cases (54.9%) with central area metastasis (unilateral metastasis 29 cases, bilateral metastasis 16 cases), 11 cases (13.4%) with invasion beyond capsule, 23 cases of ipsilateral cervical lymph node metastasis (28.0%). Postoperative hypocalcemia developed in 42 patients (51.2%). Symptomatic hypocalcemia occurred in 32 (39.0%) cases, and another 2 cases (2.4%) were found permanent hypoparathyroidism. The correlations of postoperative hypoparathyroidism with clinical factors were presented in Table 1. Over 60% patients who underwent bilateral CND were found hypoparathyroidism, and 38.9% patients who underwent unilateral CND were found hypoparathyroidism (P=0.048). There were no correlations of hypoparathyroidism rate with ipsilateral cervical dissection and parathyroid gland autotransplantation. Over 80% patients with invasion beyond capsule were found hypoparathyroidism, which was higher than 46.5% of non-invasion beyond capsule (P=0.029). There were no correlations of hypoparathyroidism with age, gender, tumor size, lymph metastasis and TNM classifications. Two cases of permanent hypoparathyroidism were bilateral PTC, and they underwent total thyroidectomy + bilateral CND. One of the two cases was found evident invasion beyond the capsule, and underwent ipsilateral central lymph node dissection.
Table 1.
Correlation of postoperative hypoparathyroidism with clinical factors in 82 PTC patients
| Number | Hypocalcemia (%) | P | |
|---|---|---|---|
| Gender | |||
| Male | 15 | 7 (46.7) | 0.696 |
| Female | 67 | 35 (52.2) | |
| Age | |||
| ≥45 y | 37 | 17 (45.9) | 0.386 |
| <45 y | 45 | 25 (55.6) | |
| Autotransplantation | |||
| Yes | 15 | 9 (60.0) | 0.452 |
| No | 67 | 33 (49.3) | |
| CND | |||
| Ipsilateral | 36 | 14 (38.9) | 0.048 |
| Bilateral | 46 | 28 (60.9) | |
| Lateral neck dissection | |||
| Yes | 23 | 9 (39.1) | 0.171 |
| No | 59 | 33 (55.9) | |
| Tumor size | |||
| ≤1 cm | 48 | 23 (47.9) | 0.477 |
| >1 cm | 34 | 19 (55.9) | |
| Tumor invasion beyond the thyroid capsule | |||
| No | 71 | 33 (46.5) | 0.029 |
| Yes | 11 | 9 (81.8) | |
| Lymph nodes metastasis | |||
| Yes | 47 | 23 (48.9) | 0.632 |
| No | 35 | 19 (54.3) | |
| TNM classification | |||
| I, II | 59 | 30 (50.8) | 0.914 |
| III, IV | 23 | 12 (52.2) |
There was no significant difference of preoperative corrected serum calcium between hypoparathyroidism group and non-hypoparathyroidism group. There was significant difference of postoperative corrected serum calcium between hypoparathyroidism group (1.75 mmol/L) and non-hypoparathyroidism (2.12 mmol/L) (P<0.001). One month later, serum calcium returned normal in hypoparathyroidism group, which was similar to that in non-hypoparathyroidism group. However, two permanent hypoparathyroidism patients (1.82 mmol/L and 1.74 mmol/L) did not return to normal.
The detailed comparisons of hypoparathyroidism group and non-hypoparathyroidism group were summarized in Table 2. PTH levels reduced 37.93% in all patients underwent unilateral surgeries, and decreased 67.21% in those with bilateral surgeries (Figure 1). Six months later, they did not return to preoperative level.
Table 2.
Comparisons of serum test values (Mean ± SD) among different group
| Hypothyroidism (n=42) | Non-hypothyroidism (n=40) | P value | Patient 1 with permanent hypothyroidism | Patient 2 with permanent hypothyroidism | All patients | |
|---|---|---|---|---|---|---|
| Corrected serum calcium (mmol/L) (Range: 2.00 to 2.60) | ||||||
| Preoperation | 2.31±0.08 | 2.30±0.08 | 0.394 | 2.22 | 2.35 | 2.31±0.08 |
| Lowest value post operation | 1.75±0.14 | 2.12±0.16 | <0.001 | 1.61 | 1.70 | 1.93±0.24 |
| 1 month after operation | 2.30±0.17 | 2.31±0.12 | 0.795 | 1.88 | 1.80 | 2.31±0.15 |
| 6 month after operation | 2.28±0.18 | 2.28±0.09 | 0.981 | 1.82 | 1.74 | 2.28±0.18 |
| PTH (ng/L) | ||||||
| PTH0 | 39.69±10.80 | 45.0±14.08 | 0.058 | 64.56 | 20.97 | 42.28±12.71 |
| PTHi | 20.26±9.41 | 31.50±11.31 | <0.001 | 11.23 | 7.21 | 25.75±11.76 |
| PTHb | 8.29±4.0 | 19.30±12.71 | <0.001 | 4.58 | 3.87 | 13.66±10.79 |
| PTHday 1 | 9.90±6.52 | 20.02±12.30 | <0.001 | 5.92 | 1.20 | 14.83±10.96 |
| PTHday 3 | 10.08±7.75 | 21.01±12.57 | <0.001 | 5.01 | 1.90 | 15.41±11.69 |
| PTH1 month | 21.83±7.37 | 30.45±11.15 | <0.001 | 4.66 | 1.25 | 26.04±10.30 |
| PTH6 month | 27.41±8.08 | 34.38±11.72 | 0.002 | 5.93 | 2.40 | 30.81±10.55 |
| PTH reduction (%) | ||||||
| PTHi | 47.06±23.42 | 28.35±17.62 | <0.001 | 82.61 | 65.61 | 37.93±22.71 |
| PTHb | 78.05±10.57 | 55.82±25.29 | <0.001 | 92.91 | 81.55 | 67.21±22.13 |
| PTHday 1 | 72.68±20.00 | 53.29±26.34 | <0.001 | 90.83 | 94.28 | 63.22±25.13 |
| PTHday 3 | 72.07±25.02 | 49.14±30.32 | <0.001 | 92.24 | 90.94 | 60.88±29.87 |
| PTH1 month | 41.04±26.30 | 28.20±27.35 | 0.033 | 92.78 | 94.04 | 34.78±27.43 |
| PTH6 month | 28.04±22.93 | 19.35±27.51 | 0.124 | 90.81 | 88.56 | 23.80±25.49 |
Footnotes: PTH0: PTH lever before the skin incision; PTHi: PTH lever at 10 minutes after lobectomy and ipsilateral CND; PTHb: PTH lever at 10 minutes after the end of bilateral operation; PTHday 1: PTH level one day after operation; PTHday 3: PTH level three days after operation; PTH1 month: PTH level one month after operation; PTH6 month: PTH level six months after operation.
Figure 1.
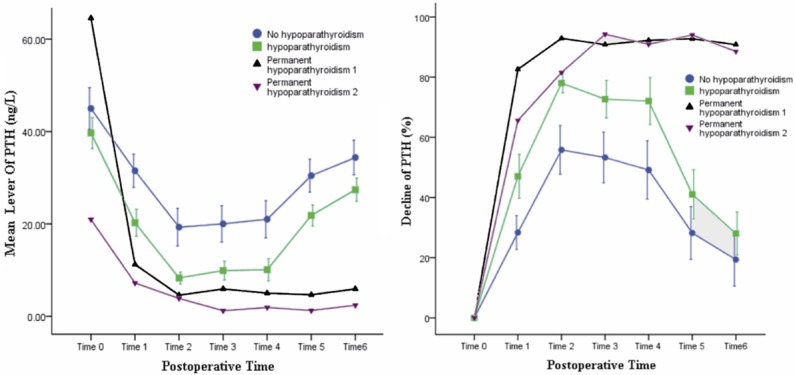
PTH changes in 82 cases of PTC patients (Time0: before the skin incision; Time1: 10 minutes after lobectomy and ipsilateral CND; Time2: 10 minutes after the end of bilateral operation; Time3: one day after operation; Time4: three days after operation; Time5: one month after operation; Time6: six months after operation).
Mean PTHi of all participants was 25.75 ng/L (SD 11.76), and it decreased 37.93% (SD 22.71%) compared to preoperative level. There was significant difference of PTHi reduction between hypoparathyroidism group (47.06%±23.42%) and non-hypoparathyroidism group (28.35%±17.62%) (P<0.001). The reductions of two permanent hypoparathyroidism cases were 83.61% and 65.62%, respectively. ROC curve analysis showed that PTHi (AUC 0.806) and its reduction degree (0.736) played significant roles in predicting hypothyroidism (P<0.001). The optimal cut-off point was between 25 ng/L (24.14) and 40% (41.5%). When we chose 25 ng/L as a cut-off point, the sensitivity was 76.2%, the specificity was 75.0%, PPV was 76.2% and NPV was 75.0%. When we chose 40% as a cut-off point, the sensitivity was 76.14%, the specificity was 72.5%, PPV was 73.2% and NPV was 70.7% (Table 3; Figure 2).
Table 3.
Predictive value of absolute value and decline of PTHi
| Decline of PTHi (%) | Lever of PTHi (ng/L) | |||||||
|---|---|---|---|---|---|---|---|---|
|
|
||||||||
| 20 | 40 | 50 | 60 | 15 | 25 | 30 | 40 | |
| Sensitivity% | 83.3 | 71.4 | 50.0 | 35.7 | 31.0 | 76.2 | 83.3 | 95.2 |
| Specificity% | 35.0 | 72.5 | 87.5 | 97.5 | 95.0 | 75.0 | 52.5 | 20.0 |
| PPV% | 57.4 | 73.2 | 80.8 | 93.8 | 86.7 | 76.2 | 64.8 | 55.6 |
| NPV% | 66.7 | 70.7 | 62.5 | 59.1 | 56.7 | 75.0 | 75.0 | 80.0 |
Footnotes: PTHi: PTH lever at 10 minutes after lobectomy and ipsilateral CND; PPV: positive predictive value; NPV: negative predictive value.
Figure 2.
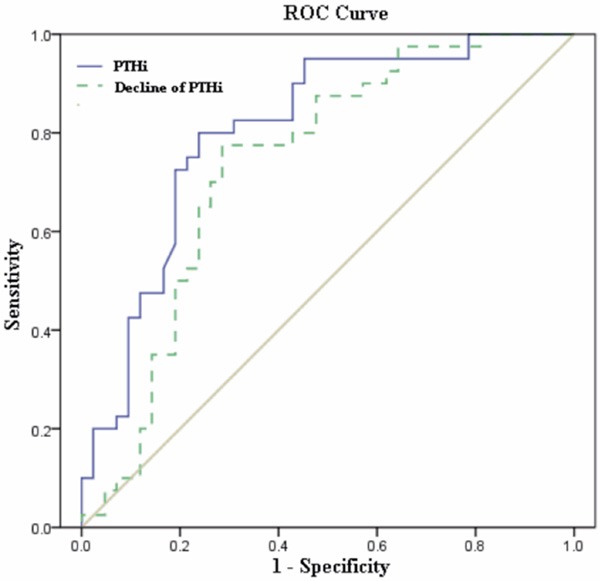
ROC curves of PTHi and decrease of PTHi from preoperative values for predicting hypocalcemia. PTHi: PTH lever at 10 minutes after lobectomy and ipsilateral CND.
Discussion
Postoperative hypocalcemia is the most common and sometimes the most severe complication observed after thyroidectomy. Its incidence varies from 1.7 to 68%, which was correlated with disease type, surgical methods, diagnostic criteria and surgeons’ experience [14-16]. In the presented study, postoperative hypoparathyroidism rate was 51.2%, which was a little higher than that in other studies. This was because all participants underwent total or near-total thyroidectomy plus CND, and 56.1% patients underwent bilateral CND. Higgins et al. reported that 22.1% (23 in 104 cases) patients who underwent total thyroidectomy were found hypocalcemia, in which two cases were permanent. However, only 52 cases were malignant thyroid carcinoma and 28 cases underwent paratracheal lymphadenectomy [17]. Undoubtedly, CND may lead to more risks of vessel damages and unnecessary resection. In our study, the hypocalcemia rate of patients who underwent bilateral CND was 60.9%, which was significantly higher than that of unilateral CND. Permanent hypocalcemia was 2.4%, which was similar to other studies [15,18]. Our study also showed that hypocalcemia rate was correlated with invasion beyond capsule. Invasion beyond capsule was more likely to induce lymph node metastasis, so more patients underwent bilateral CND were observed.
Recurrent laryngeal nerve injury and hypoparathyroidism are main complications of PTC surgeries. Recurrent laryngeal nerve injury can be detected by nerve monitoring, but intraoperative parathyroid function is difficult to assess. Serum calcium achieved the lowest point 48 hours later after the operation, so it could not be used to predict postoperative hypoparathyroidism [19]. Previous studies suggested the color of parathyroid gland to predict hypoparathyroidism, but it was not reliable. Kuhel and Carew performed incisional biopsies in 14 consecutive cases. Of the 34 parathyroid glands that were histologically confirmed, 17 appeared nonviable, with either no bleeding or minimal venous oozing. However, only 5 glands were severely discolored (black), with the other 12 having normal coloration. They concluded that the absence of discoloration was not a reliable way to determine whether the parathyroid blood supply was intact [20]. Afterwards, many studies suggested high correlations of PTH level with hypoparathyroidism, and PTH level in perioperative period was considered the most effective parameter to predict postoperative hypocalcemia [11]. If postoperative PTH was normal, the hypocalcemia was more likely to be minor and limited. Some research compared the diagnostic accuracy of hypoparathyroidism in different time phase after the operation. Sywak et al. [21] studied 100 patients who underwent thyroidectomy and measured PTH at 4 and 24 h. They found no difference between 4- and 24-h samples. Roh and Park [22] examined quick PTH levels preoperatively and at 10 min, 1 h, and 24 h postoperatively. Hypocalcemia developed in 34 of 92 patients who had significantly lower 10-min PTH than patients with normocalcemia. They found that the 10-min result was highly correlative with subsequent measurements and could be used to predict hypocalcemia. A comprehensive review concluded that a single PTH measurement taken any time from 10 min postoperative to several hours later would provide equally accurate results for predicting post-thyroidectomy hypocalcemia [9]. Our study also found that PTH was at lowest level after operation, and did not return normal several days later. These studies above suggested that PTH changes could be used to predict parathyroid function after operation.
At present, the detection of PTH is mainly used for guiding patient early hospital discharge or supplementary calcium supplements as early as possible. These testing are usually at the end of the operation, despite testing time is different. However, if PTH was used to guide the choice of PTC surgery, the testing time must be prior to the operation. Intraoperative PTH determination in the application of parathyroid surgery has given us enlightenment. As for sporadic primary hyperparathyroidism, if PTH dropped over 50% after resecting abnormal parathyroid gland, the surgery was considered a success [13]. In our study, the PTH detection time was after unilateral thyroidectomy + ipsilateral central dissection, and we found a significant reduction of PTH. The mean PTH reduction of all patients underwent bilateral thyroidectomy was 67.21%, and it was 37.93% for unilateral thyroidectomy, which was more evident in hypoparathyroidism patients (47.06%). That was to say, PTH level could reflect the real-time function of ipsilateral parathyroidism. The PTH level and its reduction degree had moderate diagnostic value, and the AUC were 0.806 and 0.736, respectively. The diagnostic accuracy of postoperative PTH in predicting hypothyroidism was a bit lower, but it still had an over 70% sensitivity and specificity based on the optimal cut-off of ROC. When PTH was over 25 ng/L, 75% patients would not have hypoparathyroidism; When PTH was under 25 ng/L, 76.2% patients would have hypoparathyroidism. When PTH was under 15 ng/L, 86.7% patients would have hypoparathyroidism, among which 2 cases (13.3%) were permanent hypoparathyroidism. Therefore, we considered that under certain circumstance like no focus in contralateral thyroid lobe, if PTH reduction was significant especially over 60% or its absolute value was lower than 15 ng/L, we should not conduct the contralateral thyroid gland resection and central area dissection. That was because large extent surgery might benefit little at the moment, but the risks of severe complications were increased. If PTH reduction was minor indicating well preserving of ipsilateral parathyroid gland, we can conduct a bit more contralateral surgeries, because the risk of hypoparathyroidism was low, not even to mention the impossibility of permanent hypoparathyroidism.
In conclusion, for PTC surgery, we should carefully balance the benefits and its complication risks. PTH level and its decreasing degree after unilateral operation played predicting roles in assessing hypoparathyroidism, which could be used as a reference for choosing operative methods.
Acknowledgements
The study was supported by the Key Project of Zhejiang Health and Medical Funding Platform (2012RCA010).
Disclosure of conflict of interest
None.
References
- 1.Gharib H, Papini E, Paschke R, Duick DS, Valcavi R, Hegedus L, Vitti P. American Association of Clinical Endocrinologists, Associazione Medici Endocrinologi, and European Thyroid Association medical guidelines for clinical practice for the diagnosis and management of thyroid nodules. J Endocrinol Invest. 2010;33(Suppl 5):1–50. [PubMed] [Google Scholar]
- 2.Noguchi S, Murakami N, Yamashita H, Toda M, Kawamoto H. Papillary thyroid carcinoma: modified radical neck dissection improves prognosis. Arch Surg. 1998;133:276–280. doi: 10.1001/archsurg.133.3.276. [DOI] [PubMed] [Google Scholar]
- 3.Cooper DS, Doherty GM, Haugen BR, Kloos RT, Lee SL, Mandel SJ, Mazzaferri EL, McIver B, Pacini F, Schlumberger M, Sherman SI, Steward DL, Tuttle RM. Revised American Thyroid Association management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid. 2009;19:1167–1214. doi: 10.1089/thy.2009.0110. [DOI] [PubMed] [Google Scholar]
- 4.Brito JP, Hay ID, Morris JC. Low risk papillary thyroid cancer. BMJ. 2014;348:g3045. doi: 10.1136/bmj.g3045. [DOI] [PubMed] [Google Scholar]
- 5.Bilimoria KY, Bentrem DJ, Ko CY, Stewart AK, Winchester DP, Talamonti MS, Sturgeon C. Extent of surgery affects survival for papillary thyroid cancer. Ann Surg. 2007;246:375–381. doi: 10.1097/SLA.0b013e31814697d9. discussion 381-374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sosa JA, Bowman HM, Tielsch JM, Powe NR, Gordon TA, Udelsman R. The importance of surgeon experience for clinical and economic outcomes from thyroidectomy. Ann Surg. 1998;228:320–330. doi: 10.1097/00000658-199809000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Saunders BD, Wainess RM, Dimick JB, Doherty GM, Upchurch GR, Gauger PG. Who performs endocrine operations in the United States? Surgery. 2003;134:924–931. doi: 10.1016/s0039-6060(03)00420-3. discussion 931. [DOI] [PubMed] [Google Scholar]
- 8.Randolph GW, Dralle H, Abdullah H, Barczynski M, Bellantone R, Brauckhoff M, Carnaille B, Cherenko S, Chiang FY, Dionigi G, Finck C, Hartl D, Kamani D, Lorenz K, Miccolli P, Mihai R, Miyauchi A, Orloff L, Perrier N, Poveda MD, Romanchishen A, Serpell J, Sitges-Serra A, Sloan T, Van Slycke S, Snyder S, Takami H, Volpi E, Woodson G. Electrophysiologic recurrent laryngeal nerve monitoring during thyroid and parathyroid surgery: international standards guideline statement. Laryngoscope. 2011;121(Suppl 1):S1–16. doi: 10.1002/lary.21119. [DOI] [PubMed] [Google Scholar]
- 9.Grodski S, Serpell J. Evidence for the role of perioperative PTH measurement after total thyroidectomy as a predictor of hypocalcemia. World J Surg. 2008;32:1367–1373. doi: 10.1007/s00268-008-9545-5. [DOI] [PubMed] [Google Scholar]
- 10.Salinger EM, Moore JT. Perioperative indicators of hypocalcemia in total thyroidectomy: the role of vitamin D and parathyroid hormone. Am J Surg. 2013;206:876–881. doi: 10.1016/j.amjsurg.2013.08.020. discussion 881-872. [DOI] [PubMed] [Google Scholar]
- 11.AES Guidelines 06/01 Group. Australian Endocrine Surgeons Guidelines AES06/01. Postoperative parathyroid hormone measurement and early discharge after total thyroidectomy: analysis of Australian data and management recommendations. ANZ J Surg. 2007;77:199–202. doi: 10.1111/j.1445-2197.2007.04018.x. [DOI] [PubMed] [Google Scholar]
- 12.Vignali E, Picone A, Materazzi G, Steffe S, Berti P, Cianferotti L, Cetani F, Ambrogini E, Miccoli P, Pinchera A, Marcocci C. A quick intraoperative parathyroid hormone assay in the surgical management of patients with primary hyperparathyroidism: a study of 206 consecutive cases. Eur J Endocrinol. 2002;146:783–788. doi: 10.1530/eje.0.1460783. [DOI] [PubMed] [Google Scholar]
- 13.Greene AB, Butler RS, McIntyre S, Barbosa GF, Mitchell J, Berber E, Siperstein A, Milas M. National trends in parathyroid surgery from 1998 to 2008: a decade of change. J Am Coll Surg. 2009;209:332–343. doi: 10.1016/j.jamcollsurg.2009.05.029. [DOI] [PubMed] [Google Scholar]
- 14.Quiros RM, Pesce CE, Wilhelm SM, Djuricin G, Prinz RA. Intraoperative parathyroid hormone levels in thyroid surgery are predictive of postoperative hypoparathyroidism and need for vitamin D supplementation. Am J Surg. 2005;189:306–309. doi: 10.1016/j.amjsurg.2005.01.006. [DOI] [PubMed] [Google Scholar]
- 15.Alhefdhi A, Mazeh H, Chen H. Role of postoperative vitamin D and/or calcium routine supplementation in preventing hypocalcemia after thyroidectomy: a systematic review and meta-analysis. Oncologist. 2013;18:533–542. doi: 10.1634/theoncologist.2012-0283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cavicchi O, Piccin O, Caliceti U, Fernandez IJ, Bordonaro C, Saggese D, Ceroni AR. Accuracy of PTH assay and corrected calcium in early prediction of hypoparathyroidism after thyroid surgery. Otolaryngol Head Neck Surg. 2008;138:594–600. doi: 10.1016/j.otohns.2008.01.016. [DOI] [PubMed] [Google Scholar]
- 17.Higgins KM, Mandell DL, Govindaraj S, Genden EM, Mechanick JI, Bergman DA, Diamond EJ, Urken ML. The role of intraoperative rapid parathyroid hormone monitoring for predicting thyroidectomy-related hypocalcemia. Arch Otolaryngol Head Neck Surg. 2004;130:63–67. doi: 10.1001/archotol.130.1.63. [DOI] [PubMed] [Google Scholar]
- 18.Rosato L, Avenia N, Bernante P, De Palma M, Gulino G, Nasi PG, Pelizzo MR, Pezzullo L. Complications of thyroid surgery: analysis of a multicentric study on 14,934 patients operated on in Italy over 5 years. World J Surg. 2004;28:271–276. doi: 10.1007/s00268-003-6903-1. [DOI] [PubMed] [Google Scholar]
- 19.Fahmy FF, Gillett D, Lolen Y, Shotton JC. Management of serum calcium levels in post-thyroidectomy patients. Clin Otolaryngol Allied Sci. 2004;29:735–739. doi: 10.1111/j.1365-2273.2004.00895.x. [DOI] [PubMed] [Google Scholar]
- 20.Kuhel WI, Carew JF. Parathyroid biopsy to facilitate the preservation of functional parathyroid tissue during thyroidectomy. Head Neck. 1999;21:442–446. doi: 10.1002/(sici)1097-0347(199908)21:5<442::aid-hed10>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- 21.Sywak MS, Palazzo FF, Yeh M, Wilkinson M, Snook K, Sidhu SB, Delbridge LW. Parathyroid hormone assay predicts hypocalcaemia after total thyroidectomy. ANZ J Surg. 2007;77:667–670. doi: 10.1111/j.1445-2197.2007.04183.x. [DOI] [PubMed] [Google Scholar]
- 22.Roh JL, Park CI. Intraoperative parathyroid hormone assay for management of patients undergoing total thyroidectomy. Head Neck. 2006;28:990–997. doi: 10.1002/hed.20444. [DOI] [PubMed] [Google Scholar]


