Abstract
Objective
To examine whether overweight social network members and normative influence for obesity are associated with weight loss outcomes during obesity treatment.
Design and Methods
Participants (N=214) in a behavioral weight loss trial reported (a) the weight status of various members of their social network and (b) level of obesogenic normative influence within their social network. Weight was objectively assessed before and after treatment.
Results
At baseline, participants with partners and best friends who were overweight and those with more children and relatives who were overweight had higher BMIs (p’s<.03). However, social norms for obesity were not associated with baseline BMI. During treatment, participants lost an average of 4.4% of initial body weight, and social influence factors were adversely associated with weight loss outcomes. Having more casual friends who were overweight at baseline and being part of a social network with stronger social norms for unhealthy eating predicted poorer weight losses (p’s<.023). Remaining social influence factors and changes in social influence were not associated with treatment outcomes.
Conclusions
Whereas weight status may “cluster” in social networks, only weight status of casual friends and normative influence for unhealthy eating were associated with obesity treatment outcomes.
Keywords: Social networks, social norms, obesity, weight loss
Introduction
Social networks (i.e. the web-like relations among social ties of different types and strengths) have been shown to impact a variety of health outcomes,(1-3) including obesity.(4) Christakis and colleagues demonstrated that a person’s chance of becoming obese increases 57% if a close friend becomes obese, 40% if a sibling becomes obese, and 37% if a spouse becomes obese.(4)
Social norms, or beliefs about what is socially acceptable within a social network, are thought to at least partially account for the “clustering” of health behaviors in social networks.(2-4) Laboratory studies with college women show that norm inductions for overeating (e.g., “previous participants have consumed large amounts of food”) lead to greater caloric consumption.(5-7) Similarly, cross-sectional studies with young adults show that social norms for healthy eating, physical activity, and weight loss are associated with self-reported dietary intake, exercise behaviors, and weight loss intentions.(8-11)
To our knowledge, no one has examined whether social networks or social norms are associated with BMI in adults presenting for obesity treatment. Moreover, while some studies have shown that psychosocial factors impact weight loss outcomes (e.g., self-efficacy, social support, dietary restraint, and depression) and our previous work showed that social influence factors are associated with weight loss intentions, (11-15) no one has examined whether overweight social contacts (e.g., family, friends) or social norms for unhealthy eating and inactivity impact actual weight loss. Understanding the impact of social influence processes on obesity treatment outcomes could inform the development of a social network intervention for weight loss. Thus, given findings from community samples and young adults,(4, 11) we aimed to determine whether (a) treatment seeking adults with more social contacts who are overweight and stronger social norms for obesity have higher BMIs at baseline, (b) baseline social influence for overweight predicts poorer weight losses during treatment, and (c) decreases in number of social network members who are overweight and decreases in social norms for obesity during treatment are associated with better weight loss outcomes. Also, given previous research suggesting that emotionally close social ties (e.g., partners, best friends) have more social influence,(4, 11) we explored the differential associations of various types of social contacts (e.g., partners, best friends, colleagues) on weight.
Methods and Procedures
Data reported herein were collected during a randomized trial testing the effects of adding behavioral weight loss strategies to the Shape Up Rhode Island (SURI) 2011 campaign, an annual community-based weight loss initiative open to all adult residents of Rhode Island.(16) At the beginning of the trial, participants were randomized to one of three treatment conditions: (a) SURI alone, (b) SURI + an Internet-based behavioral weight loss program based on the Diabetes Prevention Program, or (c) SURI + the Internet behavioral weight loss program + access to optional group sessions. Throughout the 3 month SURI program, all participants reported their weight, diet, and activity into the SURI website, received regular newsletters, and had access to community events focused on healthy eating and physical activity. Participants also received a paper booklet to track their weight, diet, and activity; a pedometer to monitor their steps; and regular prizes and recognition for reaching weight and activity goals. Those participants assigned to the Internet behavioral weight loss arms had access to a website with weekly multimedia lessons focused on behavioral weight loss strategies and a self-monitoring platform where they submitted their weight, diet, and activity information and received weekly, automated feedback. Individuals assigned to the arm that involved optional group sessions were also given access to 12 weekly group meetings led by a dietitian or exercise physiologist. Group sessions included a private weigh-in and presentation of material that supplemented the Internet program. Results from this trial have been published; there were significant differences in weight loss among all three groups at post-treatment with SURI + Internet + group yielding the most weight loss, SURI + Internet yielding the next largest weight losses, and SURI alone producing the smallest weight loss.(16)
Measures
All measures were completed before the SURI program and at the end of the SURI program unless noted otherwise.
Demographics
At baseline, participants reported basic demographic information.
Weight & height
Weight was measured to the nearest 0.1kg using a digital scale. Height was measured using a wall-mounted stadiometer at baseline. Body Mass Index (BMI) was calculated using the formula weight in kg / height in m2.
Overweight social network members
Participants were asked to indicate whether various members of their social network were overweight. Specifically, they reported whether their partner / significant other was overweight (“Yes” = 1; “No” = 0), whether their best friend was overweight (“Yes” = 1; “No” = 0), and, for those with children, number of overweight children. Those without a partner, a best friend, or children checked a box indicating that the relationship was “not applicable.” Participants were also asked number of casual friends, relatives, and colleagues / classmates that are overweight on a scale ranging from “None” (0) to “All” (4). This social network measure has been used in previous studies and has demonstrated excellent validity, with greater number of overweight social contacts associated with higher BMI and weight-related social influence measures.(11)
Social norms for unhealthy eating and inactivity
Unhealthy eating norms were measured by having participants indicate (a) how socially acceptable it is in their social network to eat unhealthy foods / large portions (“Very Unacceptable”=0; “Very Acceptable”=4), (b) how often people in their social circle encourage them to eat large portions, unhealthy foods, or have second helpings (“Never”=0; “Very Often”=4), and (c) how often members of their social circle bring home unhealthy foods or actually give them larger portions or second helpings (“Never”=0; “Very Often”=4). Items were averaged. Higher scores indicate stronger social norms for unhealthy eating. This measure has excellent reliability and validity metrics.(11)
To measure social norms for inactivity, participants reported (a) how acceptable it is in their social circle to be inactive (“Very Unacceptable”=0; “Very Acceptable”=4) and (b) how often people in their social circle discourage them from engaging in physical activity (“Never”=0; “Very Often”=4). Items were averaged. Higher scores indicate stronger social norms for inactivity. This measure has demonstrated good to excellent psychometric properties.(11)
Statistical Analyses
Participant characteristics were summarized using descriptive statistics. Correlations (continuous variables) or t-tests (dichotomous variables) were conducted to examine the association between social influence factors (i.e. network members and norms) and baseline BMI. Controlling for treatment arm, regression analyses examined whether baseline overweight social contacts or baseline social norms predicted percent weight loss during treatment. Changes in social influence from pre- to post-treatment were tested using within subjects t-tests, and, controlling for treatment arm, correlations were conducted to examine whether change in overweight network members and norms for unhealthy eating and inactivity were associated with weight loss outcomes during treatment. Statistical significance was indicated by P<.05.
Results
Participant characteristics
A total of 214 participants with overweight or obesity (BMI>=25kg/m2) enrolled in the weight loss trial and completed all measures at baseline and post-treatment (see Table 1 for participant characteristics). At baseline, participants’ mean BMI was 34.6 ± 6.9 kg/m2. Number of overweight social network members was was high. Over half of participants had a partner or best friend who was overweight (54.2% and 51.2%, respectively). Among participants with children (N=165), 37.0% had at least one child who was overweight. On a scale ranging from 0 (“Nobody”) to 4 (“All”), participants’ indicated that approximately half of their casual friends (1.9±0.8), relatives (2.0±1.1), and coworkers or classmates (2.0±1.0) were overweight. Social norms for eating an obesogenic diet and being inactive were rated as 1.7±0.9 and 1.5±0.6, respectively, on a scale from 0 to 4, with higher scores indicative of stronger normative influence for obesity.
Table 1.
Participant demographics.
| Total Sample (N = 214) | |
|---|---|
| Gender (Female n, %) | 179 (83.6) |
|
| |
| Age (years; M ± SD) | 47.2 ± 11.0 |
|
| |
| Ethnicity n (%) | |
| Not Hispanic / Latino | 202 (94.4) |
| Hispanic Latino | 10 (4.7) |
| Declined | 2 (0.9) |
|
| |
| Race n (%) | |
| White | 187 (87.4) |
| Non-white | 27 (12.6) |
|
| |
| Education n (%) | |
| Less than college | 73 (34.1) |
| College or beyond | 140 (65.4) |
| Declined | 1 (0.5) |
Associations between baseline social networks and social norms with baseline BMI
At baseline, participants with more close social contacts who were overweight had higher BMIs. Specifically, participants with partners or best friends who were overweight had significantly higher BMIs than participants with normal weight partners or best friends (p’s<.04; see Figure 1). In addition, having more children and more relatives who were overweight was associated with a higher BMI (p’s<.03; see Figure 1). In contrast, number of casual friends and number of colleagues who were overweight was not associated with baseline BMI (p’s>.52). Social norms for unhealthy eating and inactivity were not associated with BMI (p’s≥.59).
Figure 1.
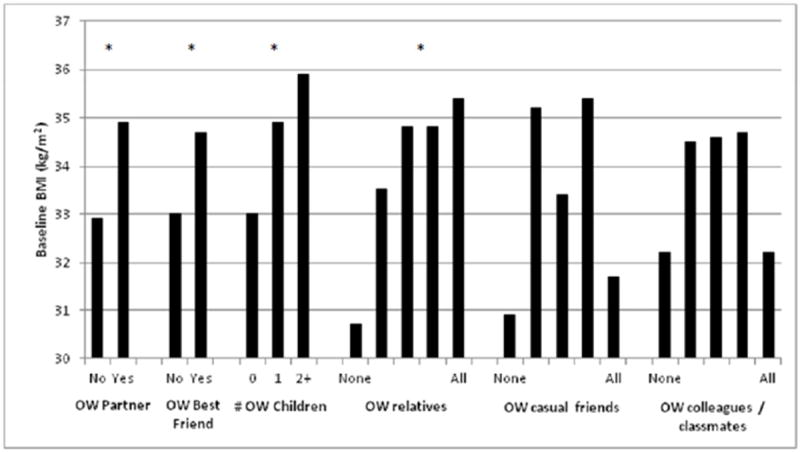
Association between weight status of social network members and BMI of treatment seeking OW/OB.*
OW = overweight
*indicate that social contact weight status was significantly associated with participant BMI (p<.05)
Associations between social networks and social norms and weight loss during obesity treatment
During the weight loss program, participants lost an average of 4.4 ± 5.0 percent of initial body weight. Baseline overweight social network members and social norms for obesity predicted poorer treatment outcomes. Specifically, having more casual friends who were overweight at baseline predicted smaller weight losses (β=-1.2, SE=.44, t=-2.6, p=.009; Figure 2). Baseline social norms for unhealthy eating also predicted outcomes; participants part of a network with greater acceptability for eating unhealthy foods/large portions had poorer weight losses (β=-.83, SE=0.36, t=2.29, p=.023; Figure 3). Remaining associations between baseline overweight social contacts and normative influence on weight loss were not significant (p’s≥.05).
Figure 2.
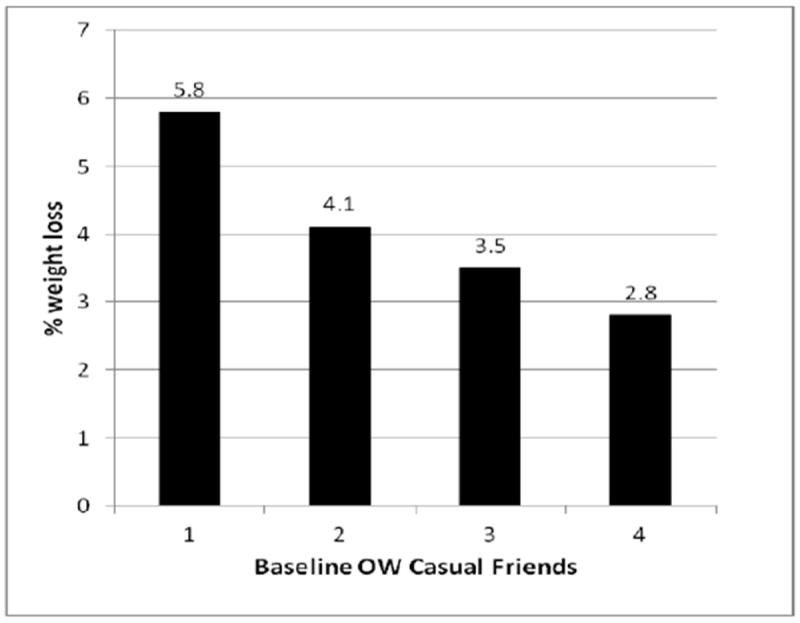
Baseline number of overweight casual friends predict weight loss during obesity treatment (0=none; 4=all).
OW = overweight
Figure 3.
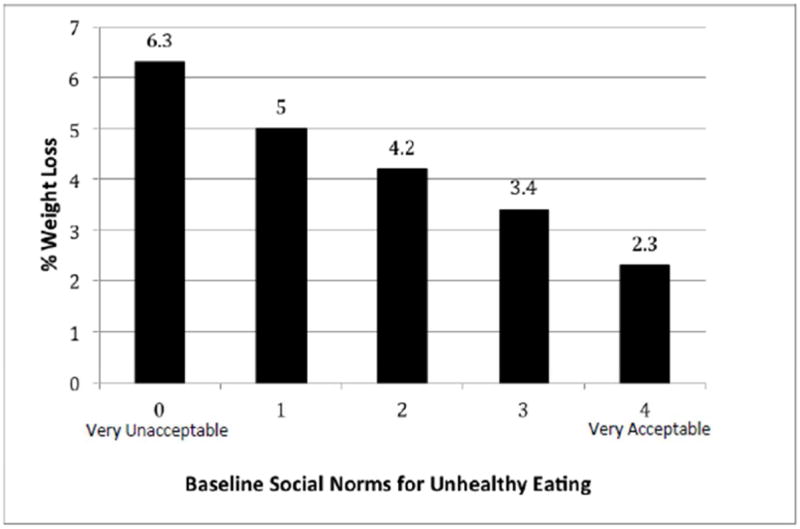
Baseline social norms for unhealthy eating predict weight loss during obesity treatment.
We examined whether social network and social influence factors changed from baseline to post-treatment and whether the changes were associated with intervention outcomes. Even though they were not involved in the intervention, percentage of romantic partners who were overweight declined from 54.2% to 45.9% (p=.009), and percentage of best friends who were overweight decreased from 51.2% to 41.7% (p=.004). Interestingly, these decreases did not affect weight loss outcomes (p’s≥.13). Moreover, despite the changes in weight status of close social ties, there were no significant changes in social norms for unhealthy eating and inactivity during treatment (p’s≥.09). Number of children, relatives, casual friends, or coworkers who were overweight did not change during treatment (p’s≥.17).
Discussion
This study examined whether overweight social network members and social norms for unhealthy eating and inactivity were associated with weight status and obesity treatment outcomes in overweight and obese treatment seeking adults. Results showed that participants reporting more close overweight social ties had higher BMIs at baseline. In addition, overweight social network members and social influence factors predicted obesity treatment outcomes. Specifically, participants who reported more overweight casual friends and those who were part of a social network with greater social acceptability for unhealthy eating had poorer weight losses during treatment.
Our finding demonstrating an association between number of overweight social contacts and BMI in treatment seeking adults is consistent with previous studies of other populations. In a sample of community adults, Christakis and colleagues showed that participant BMI status was associated with number of overweight or obese social ties.(4) Similarly, Leahey and colleagues showed that obesity clusters in young adults’ social networks.(11) We extended this prior work by examining whether different types of social ties (children, colleagues, etc.) were associated with weight. Our data suggest that emotionally close social ties (partners, best friends, children, relatives) have a greater association with obesity status at baseline than social contacts with presumably less emotional valence (e.g., casual friends, colleagues).
This is the first study to examine whether overweight social network members and obesogenic social norms predict obesity treatment outcomes. In contrast to our baseline results, which showed that emotionally close social ties (e.g., partners, best friends) have a relatively greater impact on BMI compared to more distal ties, perceived weight status and changes in weight status of emotionally salient ties (e.g., partners, best friends) did not predict weight loss outcomes during treatment. These results are consistent with previous studies showing that partners or friends have little effect on weight loss outcomes.(17-19) Interestingly, the only type of social contact that affected weight loss outcomes was casual friends; participants with fewer overweight casual friends lost more weight. Most individuals have only one best friend or partner but many casual friends. Perhaps when it comes to facilitating weight loss, having many social contacts that are normal weight is more important than having only one or two strong social ties that are normal weight. Having many normal weight ties may facilitate a broader social network that is more supportive of healthy eating and activity behaviors and, thus, weight loss. These findings are consistent with social network empirical analysis; Bahr and colleagues (20) showed that, in order to effectively harness social ties to promote weight loss, it may be important to target individuals with fewer casual friends who are overweight and are, therefore, not part of a social network with entrenched social norms for obesity.
Of particular interest are the social norms findings. Unlike previous studies,(11) we found no association between baseline BMI and social norms for obesity. Restriction of range may account for this discrepancy. Specifically, earlier studies included individuals who were normal weight, overweight, or obese (e.g., 11); however, given that the current study focused on weight loss, only individuals who were overweight or obese were included, which may have attenuated the association between BMI and normative influence for obesity. Interestingly, we did, however, find a significant association between unhealthy eating norms and obesity treatment outcomes. Participants with stronger social norms for unhealthy eating at baseline lost significantly less weight during treatment. Given these significant findings coupled with our results showing that obesogenic norms did not change during a standard treatment program, future obesity treatments targeting social network factors may consider addressing obesogenic normative influence during treatment in order to effectively improve weight loss outcomes.
This study has some limitations and several strengths. The study included a predominantly female and White sample; while these demographic characteristics are consistent with the larger SURI population,(21) lack of diversity limits generalizability. Further, to better understand whether demographic characteristics moderate the relationship between social influence factors and treatment outcomes, additional research is needed. For example, the nature and quality of social relationships may differ between men and women; thus, examining these associations in a large sample of men may yield different effects. Moreover, the majority of individuals who have access to SURI are employed and all had the necessary resources and time to participate; future studies may consider whether these findings replication among individuals who are unemployed / have fewer resources. Another limitation is that participants may have inaccurately reported the weight status of social ties. However, previous research has shown that individuals who are overweight/obese are able to accurately categorize weight information into normal weight vs. overweight or obese.(22) Finally, future studies may consider obtaining a count of total number of social network members who are overweight. This study has several strengths. It is the first study to examine the association between social network and social influence factors and objectively assessed BMI in overweight or obese treatment seeking adults. Moreover, while other areas of health behavior change such as substance abuse and HIV prevention have demonstrated the importance of targeting social norms to improve treatment outcomes,(23, 24) this is the first study to demonstrate that overweight social network members and obesogenic normative influence are associated with weight loss during obesity treatment. These findings underscore the importance of addressing social influence factors in behavioral weight loss treatment and provide explicit treatment targets (e.g., casual friends, social norms) for future social network obesity treatment interventions.
What is already known about this subject
Weight status among social contacts is correlated (e.g., individuals who are overweight are more likely to have partners, friends, and family members who are overweight).
Social norms, or beliefs about what is socially acceptable in a social network, have been shown to influence eating and activity behaviors.
What this study adds
This is the first study to examine whether the weight status of different types of social network members (partners, friends, or co-workers) are associated with weight loss outcomes in obesity treatment.
This is also the first study to show that social norms for unhealthy eating may adversely affect weight loss during treatment.
Footnotes
Conflict of Interest Statement: The authors have no conflicts of interest to report.
References
- 1.Piko BF, Luszczynska A, Gibbons FX, Teközel M. A culture-based study of personal and social influences of adolescent smoking. Eur J Public Health. 2005;15(4):393–398. doi: 10.1093/eurpub/cki008. [DOI] [PubMed] [Google Scholar]
- 2.Rosenquist JN, Murabito J, Fowler JH, Christakis NA. The spread of alcohol consumption behavior in a large social network. Ann Intern Med. 2010;152(7):426–433, W141. doi: 10.1059/0003-4819-152-7-201004060-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Christakis NA, Fowler JH. The collective dynamics of smoking in a large social network. N Engl J Med. 2008;358(21):2249–2258. doi: 10.1056/NEJMsa0706154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Christakis NA, Fowler JH. The spread of obesity in a large social network over 32 years. N Engl J Med. 2007;357(4):370–379. doi: 10.1056/NEJMsa066082. [DOI] [PubMed] [Google Scholar]
- 5.Leone T, Pliner P, Peter Herman C. Influence of clear versus ambiguous normative information on food intake. Appetite. 2007;49(1):58–65. doi: 10.1016/j.appet.2006.11.005. [DOI] [PubMed] [Google Scholar]
- 6.Herman CP, Polivy J. Normative influences on food intake. Physiol Behav. 2005;86(5):762–772. doi: 10.1016/j.physbeh.2005.08.064. [DOI] [PubMed] [Google Scholar]
- 7.Pliner P, Mann N. Influence of social norms and palatability on amount consumed and food choice. Appetite. 2004;4(22):227–237. doi: 10.1016/j.appet.2003.12.001. [DOI] [PubMed] [Google Scholar]
- 8.Everson ES, Daley AJ, Ussher M. Brief report: the theory of planned behaviour applied to physical activity in young people who smoke. J Adolesc. 2007;30(2):347–351. doi: 10.1016/j.adolescence.2006.11.001. [DOI] [PubMed] [Google Scholar]
- 9.Gabriele JM, Walker MS, Gill DL, Harber KD, Fisher EB. Differentiated roles of social encouragement and social constraint on physical activity behavior. Ann Behav Med. 2005;29(3):210–215. doi: 10.1207/s15324796abm2903_7. [DOI] [PubMed] [Google Scholar]
- 10.Oygard L, Klepp KI. Influences of social groups on eating patterns: a study among young adults. J Behav Med. 1996;19(1):1–15. doi: 10.1007/BF01858171. [DOI] [PubMed] [Google Scholar]
- 11.Leahey TM, LaRose JG, Fava JL, Wing RR. Social influences are associated with BMI and weight loss intentions in young adults. Obesity. 2011;19(6):1157–1162. doi: 10.1038/oby.2010.301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Delahanty LM, Peyrot M, Shrader PJ, Williamson DA, Meigs JB, et al. Pretreatment, psychological, and behavioral predctors of weight outcomes among lifestyle interveniton participants in the Diabetes Prevention Program (DPP) Diabetes Care. 2013;36(1):34–40. doi: 10.2337/dc12-0733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Verheijden MW, Bakx JC, van Weel C, Koelen MA, van Staveren WA. Role of social support in lifestyle-focused weight management interventions. Eur J Clin Nutr. 2005;59(S1):S179–86. doi: 10.1038/sj.ejcn.1602194. [DOI] [PubMed] [Google Scholar]
- 14.Kiernan M, Moore SD, Schoffman DE, Lee K, King AC, et al. Social support for healhty behaviors: scale psochometrics and prediction of weight loss among women in a behavioral program. Obesity. 2012;20(4):756–64. doi: 10.1038/oby.2011.293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Anton SD, Martin CK, Redman L, York-Crowe E, Heilbronn LK, et al. Psychosocial and behavioral pre-tretment predctors of weight loss outcomes. Eat Weight Disord. 2008;13(1):30–7. doi: 10.1007/BF03327782. [DOI] [PubMed] [Google Scholar]
- 16.Leahey TM, Thomas G, Fava JL, Subak LL, Schembri M, et al. Adding evidence-based behavioral weight loss strategies to a statewide wellness campaign: A randomized controlled trial. Am J Public Health. doi: 10.2105/AJPH.2014.301870. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gorin AA, Raynor HA, Fava J, Maguire K, Robichaud E, et al. Randomized controlled trial of a comprehensive home environment-focused weight-loss program for adults. Health Psychol. 2013;32(2):128–137. doi: 10.1037/a0026959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Black DR, Gleser LJ, Kooyers KJ. A meta-analytic evaluation of couples weight-loss programs. Health Psychol. 1990;9(3):330–347. doi: 10.1037//0278-6133.9.3.330. [DOI] [PubMed] [Google Scholar]
- 19.Kumanyika SK, Wadden TA, Shults J, Fassbender JE, Brown SD, et al. Trial of family and friend support for weight loss in African American adults. Arch Intern Med. 2009;169(19):1795–1804. doi: 10.1001/archinternmed.2009.337. [DOI] [PubMed] [Google Scholar]
- 20.Bahr DB, Browning RC, Wyatt HR, Hill JO. Exploiting social networks to mitigate the obesity epidemic. Obesity. 2009;17(4):723–728. doi: 10.1038/oby.2008.615. [DOI] [PubMed] [Google Scholar]
- 21.Wing RR, Pinto AM, Crane MM, Kumar R, Weinberg BM, et al. A statewide intervention reduces BMI in adults: SHape Up Rhode Island results. Obesity. 2009;17(5):991–5. doi: 10.1038/oby.2008.655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Squiers L, Renaud J, McCormack L, Tzeng J, Bann C, et al. How accurate are Americans’ perceptions of their own weight? J Health Commun. 2014;19(7):795–812. doi: 10.1080/10810730.2013.864727. [DOI] [PubMed] [Google Scholar]
- 23.Litt MD, Kadden RM, Kabela-Cormier E, Petry NM. Changing network support for drinking: network support project 2-year follow-up. J Consult Clin Psychol. 2009;77(2):229–242. doi: 10.1037/a0015252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chernoff RA, Davison GC. An evaluation of a brief HIV/AIDS prevention intervention for college students using normative feedback and goal setting. AIDS Educ Prev. 2005;17(2):91–104. doi: 10.1521/aeap.17.3.91.62902. [DOI] [PubMed] [Google Scholar]


