Abstract
Background & objectives:
The information on multidrug resistant tuberculosis (MDR-TB) situation amongst Saharia, one of the Particularly Vulnerable Tribal Groups (PVTGs) in Madhya Pradesh, India, is not available. Hence, this study was undertaken to find the situation of MDR-TB amongst Saharia PVTG in two districts of Madhya Pradesh.
Methods:
Community based cross-sectional TB prevalence surveys were conducted among Saharia PVTG in Gwalior and Shivpuri districts of Madhya Pradesh. Chest symptomatics were identified from the individual registered for the study. Two sputum samples were collected from each of the eligible individuals, transported to the laboratory, and were examined by Ziehl-Neelsen (Z-N) smear microscopy and solid medium culture methods. Drug susceptibility testing of the isolates was done by indirect proportion method on solid medium.
Results:
MDR rate was 2.2 per cent of new cases and 8.2 per cent among the previously treated cases of TB in Gwalior while it was two per cent among the previously treated cases in Shivpuri district.
Interpretation & conclusions:
Though the prevalence of tuberculosis in these districts was alarmingly high, the MDR rates were more or less similar to national average. However, the findings of this study highlight the need for active intervention so that the MDR-TB is kept under control.
Keywords: Drug susceptibility, MDR, Saharia, tribal, tuberculosis
Multidrug resistant tuberculosis (MDR-TB) is a challenge to TB control programmes worldwide. Moreover, MDR patients can turn to extensively drug resistant TB (XDR-TB) which has much limited options for treatment1. Globally, 3.7 per cent (2.1-5.2%) of new cases and 20 per cent (13-26%) of previously treated cases are estimated to have MDR-TB. India accounts for an estimated 64,000 patients out of 3,10,000 cases of drug resistant TB estimated to have occurred amongst the notified cases of TB across the globe in a year1. In the early studies undertaken during 1965-1967, resistance to isoniazid ranged from 11-20 per cent, to streptomycin 8-20 per cent and to both drugs 4-11 per cent2. Another study showed resistance to isoniazid 15-69 per cent, to streptomycin 12-63 per cent and to both drugs 5-58 per cent3. Further, the level of drug resistance was proportionate to the duration of previous treatment3. A subsequent study from Chennai, south India, carried out a decade later reported similar results to these two earlier surveys4. This indicated that the prevalence of initial drug resistance has not changed4. The drug resistance survey (DRS) study conducted in 1999 in the two districts of Tamil Nadu reported the MDR in new cases as 2.8 per cent and in previously treated cases between 69-100 per cent5.
The drug resistance surveys conducted in the States of Gujarat and Maharashtra estimated the prevalence of MDR-TB to be about 3 per cent in new cases and 12-17 per cent in re-treatment cases, and also indicated that the prevalence of MDR-TB was not increasing in the country6. India is one of the highest MDR-TB burden countries in the world with an estimated 99,000 incident MDR-TB cases7.
A few studies in the different pockets of the country have been carried out to know the prevalence of TB amongst the tribal population8,9,10,11. However, information about drug resistant tuberculosis among them is lacking. It has been reported that the Saharia - a Particularly Vulnerable Tribal Group (PVTG) in the State of Madhya Pradesh has an alarmingly high prevalence of tuberculosis12.
The present study was conducted in Saharia PVTG in the two districts of Gwalior and Shivpuri in Madhya Pradesh to know the prevalence of TB and to assess the situation of drug resistance, particularly MDR-TB among them.
Material & Method
Study area: Cross-sectional surveys were carried out among Saharia PVTG in Gwalior and Shivpuri districts of Madhya Pradesh during December 2012 to August 2013. These districts were selected considering the operational feasibility, rapport with community and willingness to support by district authorities. The terrain was difficult, with most of the villages located in remote jungle areas having poor connectivity by road, and remained cut-off from the surrounding areas during the rainy season
Sampling and sputum collection: Both male and female individuals aged ≥15 yr were included. The required sample size for estimation of prevalence was 9200 from each district. Samples were selected by arranging all the villages in descending order of the tribal population and those villages having more than 80 per cent of tribal population were selected. A village was considered as a sampling unit and required number of villages was selected using probability proportional to the size of each block in the district to cover the estimated sample size. Sputum was collected from all chest symptomatic individuals. (individuals who had symptoms of TB like cough, fever and chest pain), identified by using a questionnaire. This was done by house to house survey.
Processing of sputum specimens: In the field, samples were stored in refrigerators and then brought to the National Institute for Research in Tribal Health (NIRTH), Jabalpur, laboratory in a cold box on every second day. The specimens were processed for culture by modified Petroff's method13, inoculated on Lowenstein-Jensen (L-J) medium and were examined for growth of Mycobacterium tuberculosis once a week for up to eight weeks. Niacin test and growth on para-nitrobenzoic acid was done to confirm the speciation, i.e. growth of M. tuberculosis. Smears were made from the processed specimens and were stained by Ziehl-Neelsen (Z-N) method and examined by trained technical staff for acid-fast bacilli (AFB)13. In addition, all positive smears and 10 per cent random sample from negatives were read once again for quality check. This laboratory is an Intermediate Reference Laboratory (IRL) for Central Tuberculosis Division, Government of India, and participates in External Quality Assurance Programme. Internal quality control procedures were also followed, each batch of drug sensitivity testing (DST) for all drugs tested was accompanied by an H37Rv strain (obtained from National Institute for Research in Tuberculosis, Chennai) which was tested along with one strain with known resistance to each drug.
Isolates were subjected to drug susceptibility testing by indirect proportion method on solid L-J medium as per standard methodology13. The final concentrations used for drugs were isoniazid 0.2 µg/ml, streptomycin 4 µg/ml, (dihydrostreptomycin sulphate, at a concentration corresponding to 4 mg/ml base), rifampicin 40 µg/ml and ethambutol 2 µg/ml. The drugs were procured from Sigma Aldrich, USA. Briefly, the M. tuberculosis isolate was suspended in distilled water and diluted in doubling dilutions. The second and fourth dilutions were used for inoculation on drug containing and drug free medium. The bottles were kept for incubation at 37°C and readings were taken on 28th and 42nd days. Any isolate with one per cent (the critical proportion) of bacilli resistant to any of the four drugs (rifampicin, isoniazid, ethambutol, and streptomycin) was classified as resistant to that drug13. MDR isolates were further processed for DST for ofloxacin (2µg/ml) and kanamycin (30µg/ml).
The detected cases of TB and MDR-TB were referred to the District TB officer for management. The study was approved by Ethics Committee of the NIRTH, Jabalpur.
Results
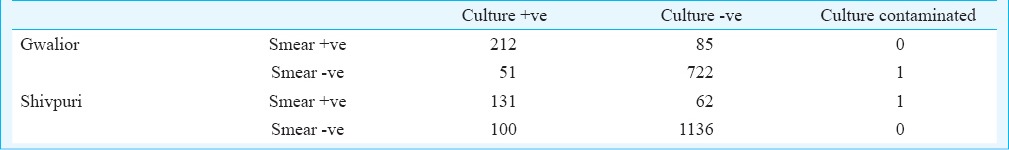
Overall 19,409 individuals were screened and sputum was collected from 2,501 symptomatic individuals. In Shivpuri, 9756 individuals were screened and sputum was collected from 1430 individuals while in Gwalior 9653 individuals were screened and sputum was collected from 1071 individuals. In Gwalior district, 263 of the 1071 individuals were culture positive for M.tuberculosis while in Shivpuri district 231 of 1430 individuals were positive by culture. The contamination rate for both the areas was 0.3 per cent (Table I). Mycobacteria other than tuberculosis (MOTT) were detected in one per cent of the isolates in Shivpuri while it was 1.8 per cent among Gwalior isolates. Prevalence of TB in Gwalior was 3294 per 1,00,000 while it was 3003 per 1,00,000 in Shivpuri district.
Table I.
Smear and culture results of the specimens
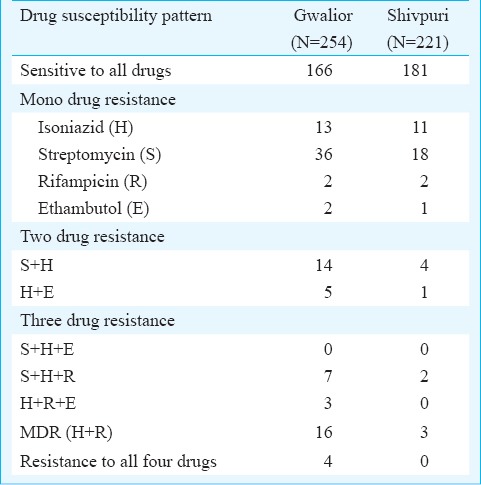
In Gwalior district, 65 per cent of the isolates were sensitive to all the first line drugs while 82 per cent of isolates from Shivpuri were sensitive to all the drugs (Table II). Mono drug resistance was the most common form of resistance. In both the areas, highest resistance was seen for streptomycin followed by isoniazid. Multidrug resistance was more in Gwalior (16 isolates) than Shivpuri (3 isolates). In Gwalior, five MDR isolates were from new cases while remaining 11 were from previously treated cases. Four of these MDR isolates were resistant to all the four drugs. The MDR rate in new cases was 2.2 per cent while it was 8.2 per cent among previously treated cases. All the three MDR isolates from Shivpuri were from previously treated cases making the MDR rate 2 per cent. Of the 19 MDR cases, 15 (79%) were resistant to ofloxacin. None of the isolates was resistant to kanamycin.
Table II.
Results of DST of the isolates
Discussion
Drug resistance in TB bacilli is a big hindrance for TB control programmes all over the world. In spite of this, data on drug resistance are very limited. This study was part of prevalence surveys conducted amongst Saharia tribe in Gwalior and Shivpuri districts of Madhya Pradesh. The prevalence of TB was over 3000 per 1,00, 000 in both these areas which is alarmingly high. The MDR rate amongst this population was more or less similar to national average of 3 per cent in new cases and 12-17 per cent in previously treated cases6. Mono drug resistance was highest for streptomycin followed by isoniazid. Similar findings have been reported earlier14. In a study from Gujarat resistance to streptomycin was highest in new cases while in previously treated cases resistance was higher for isoniazid6. In other studies also mono drug resistance was highest for isoniazid15,16. The high streptomycin resistance in the present study may be because of usage of streptomycin in the area for treatment of other infections.
According to WHO7, more number of MDR cases were detected in 2012 as compared to earlier year and India was one of the three countries which have shown largest increase in MDR-TB detected cases. However, worldwide and in most countries with high burden of MDR-TB, less than one third of the TB patients estimated to have MDR-TB were actually detected in 20127. The situation becomes more complicated in tribal population because of factors like difficult terrain, fewer resources to reach healthcare facility, poverty, ignorance and traditional beliefs, etc. Special efforts need to be made to reach such marginalized population to counter this situation.
The major limitation of this study was that the sample size estimation was not done for drug resistance but was calculated for prevalence of tuberculosis.
Though the prevalence of TB was found to be high amongst the Saharia tribe, the proportion of drug resistant cases was similar to that of other population. Active intervention in the form of active case detection and treatment compliance by patients are needed to interrupt the transmission and to keep a check on MDR rate in the community.
Acknowledgment
The authors acknowledge Dr Neeru Singh, Director, NIRTH, Jabalpur, for her support throughout the study. The contributions of the District Tuberculosis Officer, the WHO/RNTCP consultant, District Tribal Welfare Authorities, Block Medical Officers, Ashram School authorities and peripheral field staff in the district are acknowledged. The assistance provided by the laboratory and field staff is acknowledged. The study was financially supported by the Adim Jati Kalyan Vibhag, through the District Administration, Gwalior, and Indian Council of Medical Research, New Delhi.
References
- 1.WHO/HTM/TB/2012.6. Geneva: WHO; 2012. World Health Organization (WHO). Global tuberculosis report 2012. [Google Scholar]
- 2.Indian Council of Medical Research. Prevalence of drug resistance in patients with pulmonary tuberculosis presenting for the first time with symptoms at chest clinics in India. I. Findings in urban clinics among patients giving no history of previous chemotherapy. Indian J Med Res. 1968;56:1617–30. [PubMed] [Google Scholar]
- 3.Indian Council of Medical Research. Prevalence of drug resistance in patients with pulmonary tuberculosis presenting for the first time with symptoms at chest clinics in India. Part II. Findings in urban clinics among all patients, with or without history of previous chemotherapy. Indian J Med Res. 1969;57:823–35. [PubMed] [Google Scholar]
- 4.Krishnaswamy KV, Rahim MA. Primary drug resistance in pulmonary tuberculosis. Indian J Chest Dis. 1976;28:233–7. [PubMed] [Google Scholar]
- 5.Paramasivan CN, Venkataraman P, Chandrasekaran V, Bhat S, Narayanan PR. Surveillance of drug resistance in tuberculosis in two districts of South India. Int J Tuberc Lung Dis. 2002;6:479–84. doi: 10.5588/09640569512977. [DOI] [PubMed] [Google Scholar]
- 6.Ramachandran R, Nalini S, Chandrasekar V, Dave PV, Sanghvi AS, Wares F, et al. Surveillance of drug-resistant tuberculosis in the state of Gujarat, India. Int J Tuberc Lung Dis. 2009;13:1154–60. [PubMed] [Google Scholar]
- 7.Global tuberculosis report 2013. Geneva: WHO; 2013. World Health Organization (WHO) WHO/HTM/TB/2013.11. [Google Scholar]
- 8.Narang P, Tyagi NK, Mendiratta DK, Jajoo UN, Bharambhe MS, Nayar S. Prevalence of sputum-positive pulmonary tuberculosis in tribal and non-tribal populations of the Ashti and Karanja tahsils in Wardha district, Maharashtra State, India. Int J Tuberc Lung Dis. 1999;3:478–82. [PubMed] [Google Scholar]
- 9.Murhekar MV, Kolappan C, Gopi PG, Chakraborty AK, Sehgal SC. Tuberculosis situation among tribal population of Car Nicobar, India, 15 years after intensive tuberculosis control project and implementation of a national tuberculosis programme. Bull World Health Organ. 2004;82:836–43. [PMC free article] [PubMed] [Google Scholar]
- 10.Bhat J, Rao VG, Gopi PG, Yadav R, Selvakumar N, Tiwari B, et al. Prevalence of pulmonary tuberculosis amongst the tribal population of Madhya Pradesh, central India. Int J Epidemiol. 2009;38:1026–32. doi: 10.1093/ije/dyp222. [DOI] [PubMed] [Google Scholar]
- 11.Rao VG, Bhat J, Yadav R, Gopi PG, Selvakumar N, Klares DF. Prevalence of pulmonary tuberculosis among the Bharia, a primitive tribe of Madhya Pradesh, central India. Int J Tuberc Lung Dis. 2010;14:368–70. [PubMed] [Google Scholar]
- 12.Rao VG, Gopi PG, Bhat J, Selvakumar N, Yadav R, Tiwari B, et al. Pulmonary tuberculosis: a public health problem amongst the Saharia, a primitive tribe of Madhya Pradesh, central India. Int J Infect Dis. 2010;14:e713–6. doi: 10.1016/j.ijid.2010.02.2243. [DOI] [PubMed] [Google Scholar]
- 13.New Delhi, India: Central TB Division, DGHS; 2009. Central TB Division (CTD), Directorate General of Health Services (DGHS), Ministry of Health & Family Welfare, Government of India. Revised National Tuberculosis Control Programme manual of Standard Operating Procedures (SOPs). Culture of Mycobacterium tuberculosis and drug susceptibility testing on solid medium. [Google Scholar]
- 14.Vijay S, Balasangameshwara VH, Jagannatha PS, Kumar P. Initial drug resistance among tuberculosis patients under DOTS Programme in Bangalore city. Indian J Tuberc. 2004;51:17–21. [Google Scholar]
- 15.Negi SS, Gupta S, Lal S. Drug resistance in tuberculosis in Delhi: a 2 year profile (2001-2002) J Commun Dis. 2003;35:74–81. [PubMed] [Google Scholar]
- 16.Fodor T, Vadász I, Lõrinczi I. Drug-resistant tuberculosis in Budapest. Int J Tuberc Lung Dis. 1998;2:732–5. [PubMed] [Google Scholar]


