SUMMARY
Several surgical solutions have been proposed for reconstruction of the auricle in patients whose ear is missing as a result of a traumatic accident, cancer resection, or a congenital condition. These include insertion of an autogenous rib cartilage framework or a porous polymeric material into an expanded postauricular pocket. Reconstruction with rib cartilage has given good results, but requires more than one surgical step and adverse events can occur at both the donor and acceptor site, while cases of prosthesis rejection have been described following application of polymeric prostheses with the expanded postauricular pocket technique. The use of a titanium dowel-retained silicone prosthetic pinna, fixed to temporal bone, has recently been proposed. This surgical technique is particularly indicated after resection of the pinna in cancer patients and in cases of traumatic auricular injury. Bone-anchored titanium implants provided the 15 patients in this study with a safe, reliable, adhesive-free method of anchoring auricular prostheses. The prostheses allowed recovery of normal appearance and all patients were completely satisfied with their reconstructions. No surgical complications, implant failures, or prosthetic failures were encountered.
KEY WORDS: Epithesis, Pinna defects, Osseointegrated implants
RIASSUNTO
Negli anni sono state proposte differenti tecniche chirurgiche per pazienti che presentavano alterazioni del padiglione auricolare in seguito a traumatismi accidentali con amputazione parziale o totale, resezioni per patologia neoplastica e malformazioni congenite. Tali soluzioni tecniche prevedevano l'inserimento di cartilagine costale autologa modellata o di materiali polimerici porosi posizionati in una tasca di espansione retroauricolare. La tecnica ricostruttiva mediante cartilagine costale ha dato buoni risultati, ma richiede più tempi chirurgici e possono inoltre verificarsi effetti collaterali sia a livello del sito di prelievo della cartilagine (sito donatore) sia a livello del sito ricevente. Mentre l'impiego di protesi costituite da materiali polimerici presenta un'alta percentuale di casi di rigetto a livello della tasca retroauricolare. Recentemente è stato proposto l'uso di una protesi del padiglione auricolare in silicone ancorata mediante pilastri in titanio, fissati all'osso temporale. Questa tecnica chirurgica è indicata in particolare dopo la resezione del padiglione auricolare nei casi di lesione traumatica auricolare o in pazienti oncologici. Sono stati trattati con impianti in titanio osteointegrati 15 pazienti. La metodica si è rivelata affidabile e sicura. La applicazione della protesi risulta più gradevole e più stabile perché grazie al sistema di impianti osteointegrati non è necessario l'utilizzo di adesivi di ancoraggio. Le protesi hanno consentito un ottimo risultato estetico e tutti i pazienti si sono dichiarati completamente soddisfatti. Non si sono verificate complicazioni chirurgiche né nella fase di preparazione né di applicazione delle protesi.
Introduction
Absence of the pinna may be a congenital defect (microtia or anotia) or a condition acquired as a result of infection, cancer surgery, or traumatic injury. In the first case, it may be associated with malformations of the auditory canal, middle ear and inner ear. Whatever the cause, absence of the ear is a considerable aesthetic problem, which can often cause the patient severe psychological distress.
The defect can be repaired through reconstructive plastic surgery, which involves insertion, under the skin, of either an autogenous rib cartilage framework or a prosthesis made of synthetic material. Alternatively, it is possible to use an auricular epithesis (prosthetic ear). Initially, these epitheses were held in place by adhesives which, however, gave poor results in terms of stability and were often associated with skin irritations. Now, however, there exists an excellent and innovative surgical technique allowing fixation of ear epitheses by bone-anchored titanium implants. Basically, this approach is an evolution of implants for dental prostheses proposed by Branemark in 1969 – used for 40 years in the field of odontostomatology – which the same author subsequently re-proposed as percutaneous craniofacial implants for use with bone conduction hearing aids 1 2.
The authors of the present paper describe their experience using these pinna prostheses in 15 patients and discuss the technique, also in the light of the most recent scientific literature.
Materials and methods
Case series: Our case series is composed of 15 patients (14 males and 1 female with a mean age of 28.06 years, range 16-56 years) (Table I). The aetiology was congenital in 10 patients (Fig. 1), who were affected by microtia, while the remaing 5 had post-traumatic mutilation (Fig. 2). Three of the patients with microtia (Fig. 3) and two of the patients affected by traumatic mutilation had previously undergone plastic reconstructive surgery with rib cartilage grafting and were not satisfied with the results. These patients wanted their previously reconstructed ear removed and replaced with an epithesis. One patient had previously undergone canaloplasty of the right external auditory meatus. None of the patients had comorbidities.
Table I.
Characteristics of patients in the present study.
| Name | Age | Sex | Side | Disease | Previous Surgery | |
|---|---|---|---|---|---|---|
| 1 | BG | 17 | M | Left | Traumatic mutilation | None |
| 2 | LC | 25 | M | Right | Grade III microtia | Plastic reconstruction |
| 3 | MI | 17 | M | Right | Grade III microtia | None |
| 4 | JA | 34 | M | Left | Traumatic mutilation | Plastic reconstruction |
| 5 | AB | 44 | M | Left | Grade III microtia | Plastic reconstruction |
| 6 | NM | 38 | M | Right | Grade III microtia | None |
| 7 | SM | 16 | M | Right | Grade III microtia | None |
| 8 | DM | 37 | M | Right | Grade III microtia | Plastic reconstruction |
| 9 | LVS | 19 | M | Left | Grade III microtia | None |
| 10 | MB | 22 | F | Right | Grade III microtia | None |
| 11 | CN | 19 | M | Right | Grade III microtia | None |
| 12 | RG | 26 | M | Left | Traumatic mutilation | Vistafix implant |
| 13 | VS | 56 | M | Right | Traumatic mutilation | None |
| 14 | FA | 27 | M | Right | Traumatic mutilation | Plastic reconstruction |
| 15 | GC | 24 | M | Right | Grade III microtia | Canaloplasty |
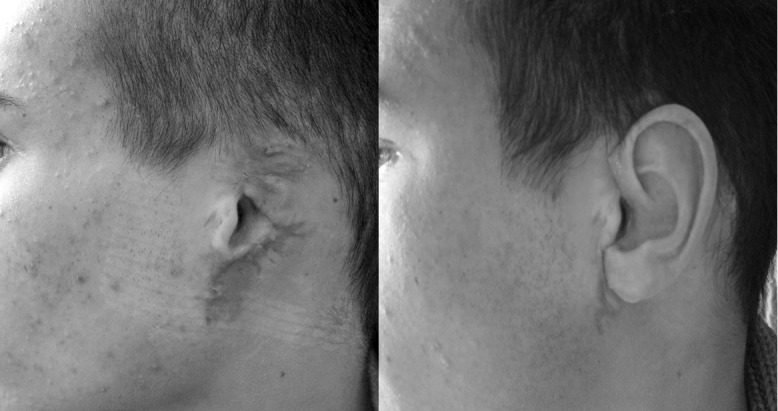
Fig. 1.

Grade III microtia, right ear: preoperative image in 3/4 right projection (left); postoperative image with prosthesis secured in position (right).
Fig. 2.
Mutilation of the left auricular pinna caused by a traumatic accident. On the right: episthesis attached to a gold-platinum cylinder-and-bar system.
Fig. 3.
Auricular rehabilitation (rib cartilage reconstruction performed elsewhere) in a patient with microtia. The patient was not satisfied with the previous reconstruction, which was removed and replaced with an episthesis (right).
The follow-up period ranged from 5 months to 2 years. After 6 weeks, all implants were osseointegrated and a retentive bar was fixed to the abutments.
The patients with microtia were offered the option of undergoing bone-anchored hearing aid (BAHA) implantation at the same time as the auricular rehabilitation with bone-anchored epitheses, but all declined, preferring to keep this as a possible option for a later stage.
Surgical procedure: Before the surgical field is prepared, and with the patient's face still fully and easily visible, the implant sites should be carefully marked, using methylene blue, down to the bone.
Two implants are normally sufficient for satisfactory retention. These are ideally placed approximately 20 mm from the centre of the external auditory canal opening or anticipated opening. They are positioned at 8 o'clock and 10:30 on the right side, and at 4 o'clock and 1:30 on the left side. In the presence of a complete malformation, the supposed location of the external auditory canal is determined by considering a triangle traced on the contralateral hemiface using the following references: the line between the lateral canthus and the auditory canal, the line between the auditory canal and the labial commissure, and the angle formed by these two lines (Figs. 1-5).
Fig. 5.
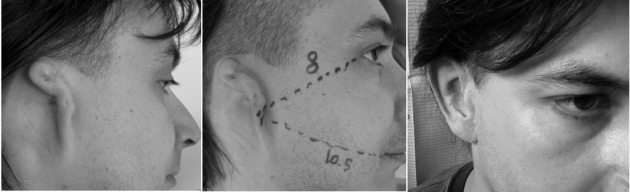
Grade III microtia, right ear. The central image shows preoperative identification of the position of the external acoustic meatus on the basis of the distance of the contralateral meatus from, respectively, the lateral canthus and the labial commissure. On the right, the patient after treatment.
We usually perform one-stage surgery, removing tags and remnants in cases of microtia and performing the necessary subcutaneous tissue reduction.
The one-stage surgical procedure can be used in adults to treat auricular defects involving non-irradiated tissue; the two-stage technique should usually be chosen for paediatric patients, and for the treatment of orbital and midface defects, and auricular defects in patients with poor bone quality 3.
An incision is made 10 mm behind the anticipated implant site. Dissection is performed down to the periosteum. A cruciate incision is then performed at each implant site. The edges are raised with a raspatory.
Drilling begins using the guide drill with the spacer kept on 3 mm. Irrigation should be used during drilling. The bottom of the hole is repeatedly checked for bone at the base of the site. If there is adequate bone thickness drilling continues to a depth of 4 mm. The drill indicator will facilitate correct drill orientation. The next step is to widen the hole to the exact diameter using a 3 or 4 mm drill countersink. Irrigation should be guaranteed.
At this point, implant installation is performed. The low speed setting should be used for implant insertion. In compact cortical bone a torque setting of 40 Ncm is recommended, whereas, in soft bone a lower torque setting of 20 N-cm should be used.
The self-tapping fixture with the premounted fixture mount is seated inside the plastic ampoule in a titanium cylinder. It is then picked up with the connection to the handpiece, which is placed into the drill handpiece.
The implant is installed without cooling irrigation until the small grooves at the distal end of the implant are well within the canal. When the flange of the implant has seated, the handpiece will automatically stop.
The mount is removed using the Unigrip screwdriver and surgical wrench. The titanium standard abutment is picked up with the abutment holder and placed into the implant. We perform manual tightening, using the abutment screw, to 25 N-cm.
The skin is then repositioned over the implants. Holes are punched through the skin exactly over abutments with a biopsy punch. The skin is then sutured. Healing caps are positioned on the abutments.
A gauze dressing is applied in a figure of 8 (foam dressing, soft silicone wound contact layer or antiseptic dressing). The healing caps are thus held in place. All patients were discharged the day after surgery and were revised for the first dressing after 7 days. The patients underwent dressings every 7 days for a month.
It is important to wait 6 weeks before loading the implants. Following healing and stabilisation of the surgical site, the patient is sent to the anaplastology technician who will prepare the epithesis, modelling it on the contralateral ear and carefully matching the skin colour (Fig. 4, right). The silicone ephitesis is created using a wax pattern. The definitive one has two sides: the inner one in an acrylic plate with clips that allow the attachment to a gold-platinum bar fixed to the abutments; the external one is made of soft silicone. Patients receive two epitheses of different colours: a pale one for winter and a tanned one for summer.
Fig. 4.

A. Preoperative image of grade III microtia, right ear (left). Gold bar attached to two titanium implants (middle). Prosthetic pinna in place, clipped onto the gold bar (right).
When the process of osseointegration is complete, the prosthesis, which has clips, is easily and securely attached to or removed from the gold-platinum cylinder-and-bar system (Fig. 4, middle).
Patients were evaluated for quality of life in the week before pinna reconstruction (T0) with the Short Form Health Survey (SF-12) 4. Assessments were repeated after 3 months (T1). Statistical analysis was performed with Pearson correlations and the results were considered significant when p ≤ 0.05.
Discussion
Absence of the ear (congenital or resulting from trauma or surgery) is a defect that can be resolved through reconstructive plastic surgery. This involves the insertion of either an autogenous rib cartilage framework or a prosthesis made from synthetic material into a subcutaneous pocket behind the ear, obtained through tissue expansion. A more recent technique is the use of epitheses made from synthetic material and secured by adhesives to the patient's skin. However, auricular reconstruction using rib cartilage has several disadvantages: it requires more than one surgical procedure, complications are very frequent, both at the implant site (infections, bleeding, haematoma, necrosis and skin graft or cartilage graft exposure) and at the graft site (infections, haematoma, scarring). Moreover, patients are very often dissatisfied with the final outcome because the new ear looks considerably different from the contralateral one 5 6.
The use of prostheses made from porous polymer material (Medpore) inserted in subcutaneous pockets, proposed by Wellisz in 1993, is frequently complicated by partial or total rejection and further scarring problems 7.
Conventional facial prosthetics has previously relied on the use of adhesives for retention. Pitfalls of the adhesive-retained prosthesis include skin irritation from the adhesives, unpredictability of retention, variability of positioning of the prosthesis and poor hygiene attributable to the tackiness of the adhesive as well as decreased life span of the prosthesis resulting in an increased number of remakes 7.
A valid and excellent alternative is that of bone-anchored implants and application of an auricular epithesis. In this regard, titanium implant systems for bone-anchored hearing aids have shown how such prostheses can be attached safely, securely, reproducibly and without the need for adhesives 3 8-10. This procedure is suitable for patients who are unwilling to undergo plastic reconstructive surgery with rib cartilage, a challenging surgical procedure that involves more than one surgical step and is associated with a risk of complications at the donor (throracic) site and/or the acceptor (implant) site 11. The use of osseointegrated implants is also the only possible solution in oncology patients who have previously undergone several surgical procedures and/or radiotherapy 12. Radiotherapy does not constitute a contraindication for this procedure, although implant loss is higher in irradiated sites than in non-irradiated sites. Granstrom reported that the adjunctive use of hyperbaric oxygen could reduce implant loss 13. It is important to note the low cost of the vistafix implant (€ 1900) and epithesis (€ 2000). Above all, patients expressed their satisfaction regarding the short hospitalisation and reduced invasiveness compared to alternative therapies. Complications associated with this surgical technique are rare (10-15% of cases). Local skin infection around the fixture can occur, as can the formation of granulation tissue and keloids. These are complications that can be avoided or resolved using appropriate medication and topical treatments without loss of the fixture 14.
Absolute contraindications to the use of titanium bone implants in prosthetic reconstruction of the auricle are exceptional and may be local or general conditions (respectively, osteitis and terminal illness or the presence of psychological disorders). Contraindications for general anaesthesia need not preclude use of these implants, since they can be positioned under local anaesthesia. This surgical technique is contraindicated in patients under 14 years of age, whose skull thickness is not sufficient to support the osseointegrated implant. Preoperative evaluation of bone thickness on CT scans should nevertheless be a mandatory part of the surgical planning in adults 15-17.
All the patients in our series underwent one-stage surgery. As mentioned earlier, indications for one-stage surgery are auricular defects, adult patients and non-irradiated tissue, while a two-stage technique should be used in paediatric patients, and to treat orbital and midface defects, as well as auricular defects in patients with poor bone quality 3.
None of the patients we treated experienced problems related to the implants (osseointegration failure or wound healing problems).
Conductive hearing loss due to malformations of the external and middle ear, present in all subjects affected by microtia, can be corrected by combining the placement of titanium implants for auricular rehabilitation with implantation of the fixture and abutment for a BAHA. In this way, both the sensory and the aesthetic problems can be resolved in a single operation. However, it should be pointed out that all the patients in our series refused to undergo BAHA implantation after testing the device prior to surgery; these patients, being well accustomed to hearing on only one side, found the increased auditory perception provided by the BAHA disorienting and irritating.
Conclusions
The pinna epithesis fixed with bone-anchored titanium implants technique is characterised by excellent aesthetic outcome and lasting results. All our patients expressed satisfaction with their prosthesis. Statistical analysis between T0 and T1 SF-12 score suggests a significant role in quality of life of patients who underwent pinna reconstruction. They had no adverse psychological reactions and were able to resume their usual physical activities without problems; indeed, thanks to the effectiveness of the anchoring system, the epithesis does not move when the patient exercises.
References
- 1.Brånemark PI, Adell R, Breine U, et al. Intra-osseous anchorage of dental prostheses. I. Experimental studies. Scand J Plast Reconstr Surg. 1969;3:81–100. doi: 10.3109/02844316909036699. [DOI] [PubMed] [Google Scholar]
- 2.Brånemark PI, Albrektsson T. Titanium implants permanently penetrating human skin. Scand J Plast Reconstr Surg. 1982;16:17–21. doi: 10.3109/02844318209006565. [DOI] [PubMed] [Google Scholar]
- 3.Wazen JJ, Wright R, Hatfield RB, et al. Auricular rehabilitation with bone-anchored titanium implants. Laryngoscope. 1999;109:523–527. doi: 10.1097/00005537-199904000-00001. [DOI] [PubMed] [Google Scholar]
- 4.Ware J, Jr, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34:220–233. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 5.Brent B. Microtia repair with rib cartilage grafts: a review of personal experience with 1000 cases. Clin Plast Surg. 2002;29:257–271. doi: 10.1016/s0094-1298(01)00013-x. [DOI] [PubMed] [Google Scholar]
- 6.Zhao Y, Wang Y, Zhuang H, et al. Clinical evaluation of three total ear reconstruction methods. J Plast Reconstr Aesthet Surg. 2009;62:1550–1554. doi: 10.1016/j.bjps.2008.07.009. [DOI] [PubMed] [Google Scholar]
- 7.Wellisz T. Reconstruction of the burned external ear using a Medpor porous polyethylene pivoting helix framework. Plast Reconstr Surg. 1993;91:811–818. doi: 10.1097/00006534-199304001-00009. [DOI] [PubMed] [Google Scholar]
- 8.Tjellström A, Lindström J, Nylén O, et al. The bone-anchored auricular episthesis. Laryngoscope. 1981;91:811–815. [PubMed] [Google Scholar]
- 9.Westin T, Tjellström A, Hammerlid E, et al. Long-term study of quality and safety of osseointegration for the retention of auricular prostheses. Otolaryngol Head Neck Surg. 1999;121:133–143. doi: 10.1016/S0194-5998(99)70142-7. [DOI] [PubMed] [Google Scholar]
- 10.Federspil PA. Ear epistheses as an alternative to autogenous reconstruction. Facial Plast Surg. 2009;25:190–203. doi: 10.1055/s-0029-1239446. [DOI] [PubMed] [Google Scholar]
- 11.Gentile P, Bottini DJ, Gravante G, et al. The use of bone-anchored implants for absent ear. J Craniofac Surg. 2008;19:744–747. doi: 10.1097/SCS.0b013e31816ae30f. [DOI] [PubMed] [Google Scholar]
- 12.Wright RF, Zemnick C, Wazen JJ, et al. Osseointegrated implants and auricular defects: a case series study. J Prosthodont. 2008;17:468–475. doi: 10.1111/j.1532-849X.2008.00309.x. [DOI] [PubMed] [Google Scholar]
- 13.Granström G. Hyperbaric oxygen therapy decreases the rejection rate of osseointegrated implants after radiotherapy. Strahlenther Onkol. 1996;172(Suppl 2):20–21. [PubMed] [Google Scholar]
- 14.Giot JP, Labbé D, Soubeyrand E, et al. Prosthetic reconstruction of the auricle: indications, techniques, and results. Semin Plast Surg. 2011;25:265–272. doi: 10.1055/s-0031-1288918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gumieiro EH, Dib LL, Jahn RS, et al. Bone-anchored titanium implants for auricular rehabilitation: Case report and review of literature. Sao Paulo Medical Journal. 2009;127:160–165. doi: 10.1590/S1516-31802009000300009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Curi MM, Oliveira MF, Molina G, et al. Extraoral implants in the rehabilitation of craniofacial defects: implant and prosthesis survival rates and peri-implant soft tissue evaluation. J Oral Maxillofac Surg. 2012;70:1551–1557. doi: 10.1016/j.joms.2012.03.011. [DOI] [PubMed] [Google Scholar]
- 17.Korus LJ, Wong JN, Wilkes GH. Long-term follow-up of osseointegrated auricular reconstruction. Plast Reconstr Surg. 2011;127:630–636. doi: 10.1097/PRS.0b013e3181fed595. [DOI] [PubMed] [Google Scholar]



