Abstract
Background and purpose
Data from the national joint registries in Australia and England and Wales have revealed inferior medium-term survivorship for metal-on-metal (MoM) total hip arthroplasty (THA) than for metal-on-polyethylene (MoP) THA. Based on data from the Nordic Arthroplasty Register Association (NARA), we compared the revision risk of cementless stemmed THA with MoM and MoP bearings and we also compared MoM THA to each other.
Patients and methods
We identified 32,678 patients who were operated from 2002 through 2010 with cementless stemmed THA with either MoM bearings (11,567 patients, 35%) or MoP bearings (21,111 patients, 65%). The patients were followed until revision, death, emigration, or the end of the study period (December 31, 2011), and median follow-up was 3.6 (interquartile range (IQR): 2.4–4.8) years for MoM bearings and 3.4 (IQR: 2.0–5.8) years for MoP bearings. Multivariable regression in the presence of competing risk of death was used to assess the relative risk (RR) of revision for any reason (with 95% confidence interval (CI)).
Results
The cumulative incidence of revision at 8 years of follow-up was 7.0% (CI: 6.0–8.1) for MoM bearings and 5.1% (CI: 4.7–5.6) for MoP bearings. At 6 years of follow-up, the RR of revision for any reason was 1.5 (CI: 1.3–1.7) for MoM bearings compared to MoP bearings. The RR of revision for any reason was higher for the ASR (adjusted RR = 6.4, CI: 5.0–8.1), the Conserve Plus (adjusted RR = 1.7, CI: 1.1–2.5) and “other” acetabular components (adjusted RR = 2.4, CI: 1.5–3.9) than for MoP THA at 6 years of follow-up.
Interpretation
At medium-term follow-up, the survivorship for cementless stemmed MoM THA was inferior to that for MoP THA, and metal-related problems may cause higher revision rates for MoM bearings with longer follow-up.
Wear particles from the polyethylene liner in metal-on-polyethylene (MoP) bearings in total hip arthroplasty (THA) are associated with osteolysis and aseptic loosening of the implant (Jacobs et al. 1994). Surgeons therefore became interested in alternatives such as metal-on-metal (MoM) bearings. The main justification for using large-diameter-head (LDH) MoM bearings in THA was less wear and the hope of lower revision rates. However, a lower risk of revision has only been found for revision due to dislocation (Kostensalo et al. 2013), whereas the total risk of revision has been found to be increased in some studies (Smith et al. 2012, Huang et al. 2013). In addition, LDH MoM was introduced in order to achieve increased range of motion and better function (Burroughs et al. 2005, Davis et al. 2007), but that has not been shown clinically (Penny et al. 2013).
Several concerns about the use of MoM bearings in hip surgery have been voiced in recent years: excessive failure rates for certain brands and implant combinations used with MoM components have been reported (Langton et al. 2011, Australian Orthopaedic Association 2013). Some designs are associated with increased frequency of aseptic loosening (Australian Orthopaedic Association 2013), and large head sizes placed on conventional stems may cause taper junction failure (Langton et al. 2012). Exposure to chromium and cobalt may cause adverse reactions to metal debris (ARMD) (Langton et al. 2010) such as pseudotumors (Pandit et al. 2008) and hypersensivity reactions (Willert et al. 2005) locally in the hip joint. Furthermore, metal ions may be genotoxic (Daley et al. 2004).
Only a few population-based studies on MoM bearings in stemmed THAs from hip arthroplasty registries have been published (Smith et al. 2012, Mokka et al. 2013b, Furnes et al. 2014), with only 1 population-based study focusing on causes of revision resulting from specific combinations of acetabular and femoral components (Mokka et al. 2013b). We compared the 6-year revision risk for MoM bearings with that for MoP bearings in cementless stemmed THA. In addition, we studied different designs of stemmed MoM THAs and the causes of revision in a population-based follow-up study using data from the Nordic Arthroplasty Register Association (NARA).
Patients and methods
The background population included approximately 26 million inhabitants of Denmark (5.6 million), Norway (5.0 million), Sweden (9.5 million), and Finland (5.4 million).
Sources of data
Individual anonymized data relating to each patient who underwent THA as recorded in the arthroplasty registries of Denmark, Norway, Sweden, and Finland were merged into the NARA database (Herberts et al. 1989, Havelin et al. 2000, Lucht 2000, Puolakka et al. 2001). The data provided by each registry were transformed according to common definitions of minimal datasets required for this study (Havelin et al. 2009). Nationally, the primary THA data were linked to potential revision data for each patient and de-identified, including deletion of the national civil registration number, before inclusion in the NARA database. Data were treated with full confidentiality, and identification of patients at the individual level is not possible in this database.
Study population
The study population consisted of patients who received stemmed THA with cementless stem and cementless cup with either MoM or MoP bearings, and with one of the following diagnoses: primary osteoarthritis (OA), femoral head osteonecrosis, inflammatory arthritis, or sequelae from childhood hip disorder. In MoP bearings, the polyethylene liner could be made of either ultra-high-molecular-weight polyethylene or (highly) cross-linked polyethylene.
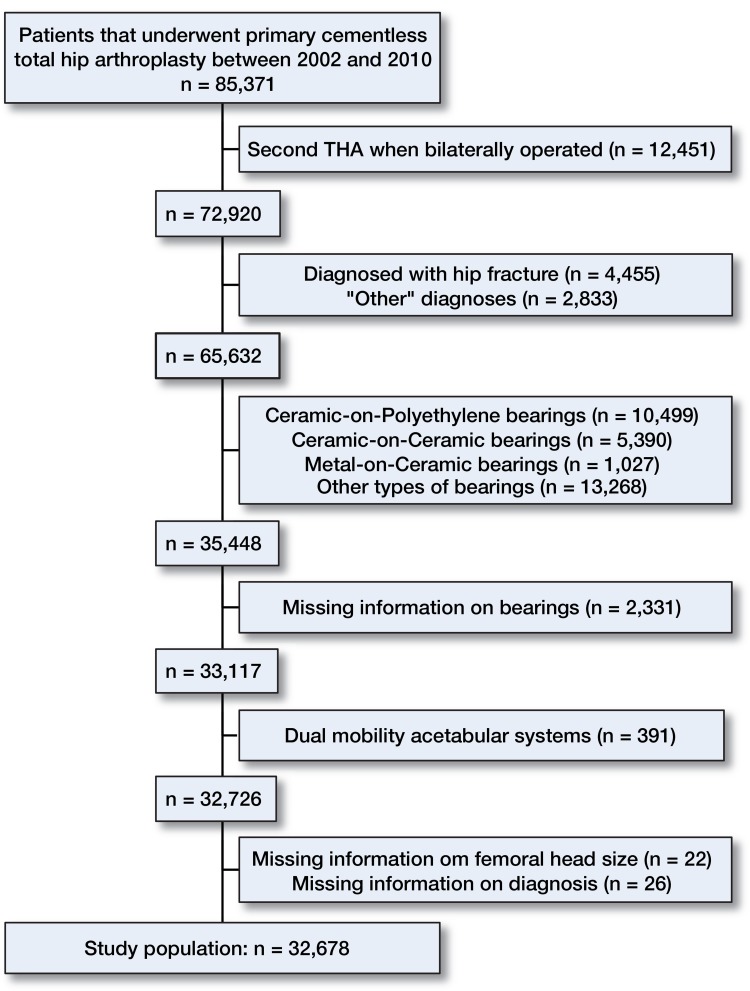
Since the registration of THA bearings was common for all databases in 2002, our study population consisted of patients who underwent primary THA surgery between January 1, 2002 and December 31, 2010 (Figure 1). When a patient received bilateral THA operations, only the first was included in the study due to the statistical assumption of independent observations (Ranstam et al. 2011). Of the 2,331 patients excluded with unregistered pairs of bearings, 505 of these had a ceramic head and 114 had a ceramic liner, eliminating the possibility of having MoM or MoP bearings. Thus, 1,712 patients with an unambiguous couple of bearings could potentially have either MoM or MoP bearings.
Figure 1.
Inclusion of patients in the study population.
Of the 309,944 primary stemmed THAs in the NARA database performed from 2002 through 2010, 32,678 primary cementless stemmed THAs (11,567 MoM and 21,111 MoP) with complete information on sex, age group, diagnosis, year of surgery, and femoral head size were included in the study.
Statistics
Patients entered the study on the date of primary surgery and were followed until revision, death, emigration, or the end of study period (December 31, 2011), whichever came first. Revision was defined as a new surgical intervention including partial or complete removal or exchange of the implant. Revision for any reason was considered to be the primary endpoint and aseptic loosening, dislocation, and all other causes of revision were considered to be secondary endpoints. Time since operation was chosen as the underlying time scale in the time-to-event analysis, and death was considered to be a competing risk.
For the presentation of demographic data and procedure characteristics, descriptive statistics were used. The chi-square test was used to compare proportions, and the 2-sample Wilcoxon rank-sum test was used to compare ages and follow-up times between groups because of skewness. For ages and follow-up times, medians and interquartile ranges (IQRs) are presented. Revision rates (per 100 person-years) were assessed for each group of bearings or specific components as the number of revisions divided by the total risk time. Cumulative incidence curves were computed using the Aalen-Johansen estimator to allow for competing risk. Competing risk analyses were used, as the Kaplan-Meier estimator is known to overestimate revision rates (Gillam et al. 2010, National Joint Registry for England and Wales 2011). The cumulative incidence curves were ended when the number of patients at risk was below 50, due to the expected statistical uncertainty in the estimates.
Pseudo-values based on the Aalen-Johansen estimator were calculated at the prespecified time points 1, 2, 3, 4, 5, and 6 years. The pseudo-observation is a transformation of the time-to-event data in which each time-to-event observation is represented by the amount of information it contains when the observation is deleted from the dataset. Once the pseudo-observations have been computed, a model for relative risk (RR) for the uncensored data was applied via a generalized estimating equation. In practice, the generalized estimating equation can be obtained in a generalized linear model for the pseudo-values with normal distribution and robust variance estimation (Klein et al. 2007, Parner and Andersen 2010). Adjustments were made for sex, age, and diagnosis for primary THA when comparing MoM bearings and MoP bearings.
Subanalyses were performed for postoperative follow-up at 1 to 6 years. We performed stratified analyses on sex and age, on OA as diagnosis, and on different component designs focusing on the most prevalent cups and the most prevalent pairs of cups and stems. We also performed stratified analyses on component designs within the MoM group, with the most frequently used acetabular component and combination of acetabular and femoral components as reference. The stratified analyses within the MoM group were adjusted for sex, age, diagnosis for primary THA, and femoral head size (categorized as ≤ 37 mm, 38–39 mm, 40–43 mm, 44–47 mm, 48–51 mm, and ≥ 52 mm). Furthermore, a stratified analysis on femoral head size was performed within the MoM group. All analyses were stopped at 6 years of follow-up as one acetabular component (Conserve Plus) had a maximum follow-up period of 6 years. When performing stratified analyses, each stratum had at least 10 registered revisions.
In August 2010, DePuy Orthopaedics voluntarily recalled the Articular Surface Replacement (ASR) acetabular component used in both hip resurfacing arthroplasty and THA, due to a 5-year revision rate of approximately 12% for the ASR Hip Resurfacing System and approximately 13% for the ASR XL Acetabular System (DePuy Companies 2013). Thus, after exclusion of patients with the ASR acetabular component, additional regression analysis as described above was performed to determine the RR of any revision for MoM THA compared to MoP THA at 6 years of follow-up, with adjustment for sex, age, and diagnosis for primary THA. Also, stratified analysis on femoral head size was performed after exclusion of ASR patients, comparing risk of any revision at 6 years of follow-up within the MoM group.
Any p-value < 0.05 was considered significant, and 95% confidence intervals (CIs) were computed. Statistical analyses were carried out using Stata statistical software, release 13.1.
Results
Description of the study population
The characteristics of the study population are presented in Table 1. Of the whole population, 35% had MoM THAs and 65% had MoP THAs. The proportion of males who had MoM THAs was higher than the proportion who had MoP THAs. The median patient ages in the 2 groups were 62 (56–69) years for MoM and 62 (56–68) years for MoP (p < 0.001). The most common diagnosis for THA was OA accounting for 92% of all MoM bearings and 89% of all MoP bearings (p < 0.001). In the MoM group, 3% were diagnosed with sequelae from childhood hip disorders. The corresponding figure in the MoP group was 6% (p < 0.001). Regarding femoral head size, 92% of MoM THAs had 38-mm or larger femoral heads, and 97% of MoP THAs had head sizes smaller than 38 mm (p < 0.001). From 2002 through 2006, 23% received MoM bearings and 35% received MoP bearings, whereas from 2007 through 2010 77% received MoM bearings and 65% received MoP bearings (p < 0.001). The 3 most frequently used design combinations of acetabular and femoral components in the MoM group were Recap/Bi-Metric (43%), M2a/Bi-Metric (21%), and Pinnacle/Corail (8%), and they were Trilogy/Bi-Metric (17%), Trilogy/CLS Spotorno (13%), and Mallory-Head/Bi-Metric (8%) in the MoP group. Most MoM THAs were performed in Finland (72%) and Denmark (23%), whereas MoP THAs were mainly performed in Denmark (57%) and Sweden (36%) (Table 1). The median follow-up was 3.6 (2.4–4.8) years for MoM bearings and 3.4 (2.0–5.8) years for MoP bearings (p < 0.001).
Table 1.
Patient- and surgery-related characteristics for the patients who received cementless total hip arthroplasty with metal-on-metal (MoM) bearings or metal-on-polyethylene (MoP) bearings. Values are numbers of patients and percentages (%) within each group
| MoM n = 11,567 | MoP n = 21,111 | p-value | |
|---|---|---|---|
| Sex | < 0.001 | ||
| Female | 5,227 (45) | 10,689 (51) | |
| Male | 6,340 (55) | 10,422 (49) | |
| Age groups (years) | < 0.001 | ||
| < 40 | 282 (2) | 576 (3) | |
| 40–49 | 969 (8) | 1,768 (8) | |
| 50–59 | 3,188 (28) | 5,578 (27) | |
| 60–69 | 4,712 (41) | 8,249 (39) | |
| 70–79 | 2,200 (19) | 4,007 (19) | |
| ≥ 80 | 216 (2) | 933 (4) | |
| Diagnosis | < 0.001 | ||
| Primary OA | 10,595 (92) | 18,694 (89) | |
| Femoral head osteonecrosis | 232 (2) | 631 (3) | |
| Arthritis | 404 (3) | 427 (2) | |
| Childhood hip disorders | 336 (3) | 1,359 (6) | |
| Femoral head size (mm) | < 0.001 | ||
| ≤ 27 | 7 (0) | 221 (1) | |
| 28–31 | 118 (1) | 10,374 (49) | |
| 32–35 | 117 (1) | 5,842 (28) | |
| 36–37 | 707 (6) | 4,068 (19) | |
| 38–39 | 2,317 (20) | 17 (0) | |
| 40–43 | 679 (6) | 403 (2) | |
| 44–47 | 2,431 (21) | 44 (0) | |
| 48–51 | 3,124 (27) | 38 (0) | |
| ≥ 52 | 2,067 (18) | 104 (1) | |
| Year of surgery | < 0.001 | ||
| 2002 | 17 (0) | 484 (2) | |
| 2003 | 39 (0) | 1,394 (7) | |
| 2004 | 109 (1) | 1,647 (8) | |
| 2005 | 887 (8) | 1,867 (9) | |
| 2006 | 1,641 (14) | 2,097 (10) | |
| 2007 | 2,305 (20) | 2,385 (11) | |
| 2008 | 2,691 (23) | 2,837 (13) | |
| 2009 | 2,357 (21) | 3,661 (17) | |
| 2010 | 1,521 (13) | 4,739 (23) | |
| Country | < 0.001 | ||
| Denmark | 2,636 (23) | 12,103 (57) | |
| Norway | 88 (1) | 1,141 (6) | |
| Sweden | 454 (4) | 7,597 (36) | |
| Finland | 8,389 (72) | 270 (1) |
Risk of revision for any reason
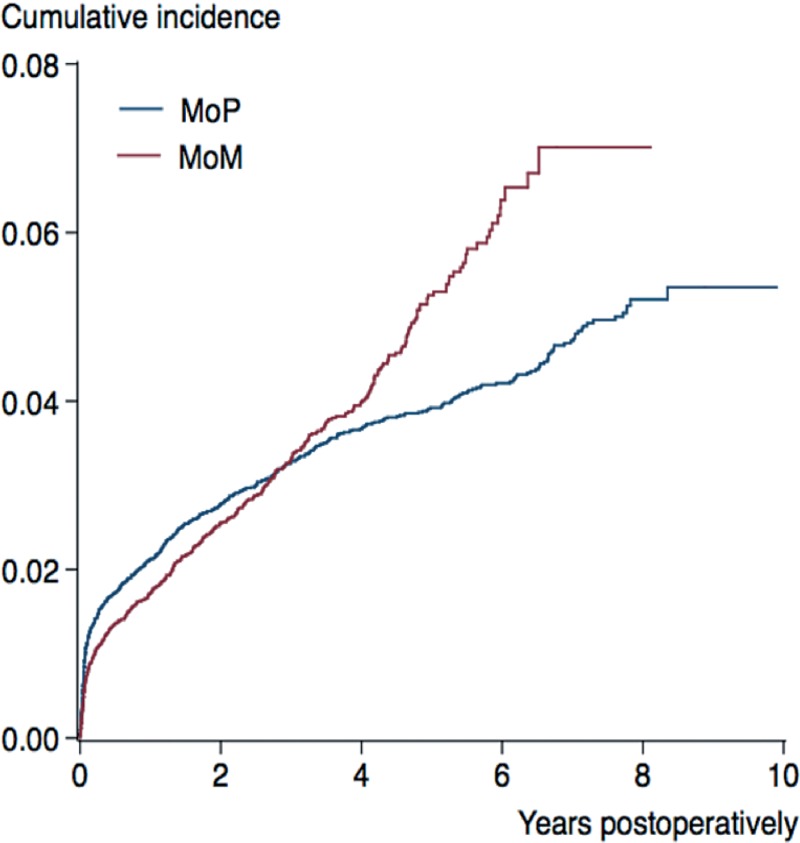
During the study period, we registered 1,236 first-time revisions following primary THA (3.8% of 32,678 patients): 4.1% for MoM bearings (470 of 11,567 patients) and 3.6% for MoP bearings (766 of 21,111 patients), corresponding to revision rates of 1.11 (CI: 1.0–1.2) per 100 person-years for MoM THA and 0.91 (CI: 0.85–0.97) per 100 person-years for MoP THA. The cumulative incidence of any revision was 7.0% (CI: 6.0–8.1) for MoM and 5.1% (CI: 4.7–5.6) for MoP at 8 years of follow-up (Figure 2). The RR of revision for any reason was statistically significantly higher for MoM after 5 and 6 years of follow-up (Table 2, see Supplementary data).
Figure 2.
Cumulative incidence for any revision of cementless total hip arthroplasty with metal-on-metal (MoM) bearings and metal-on-polyethylene (MoP) bearings.
Stratified analyses: risk of revision for any reason
Compared to MoP THA, at 6-year follow-up MoM THA had a higher risk of revision for any reason in women less than 60 years of age (1.8, CI: 1.3–2.4) and women who were 60 years old or more (1.9, CI: 1.5–2.4), in men less than 60 years old (1.4, CI: 1.1–1.9), and in patients who were diagnosed with OA of the hip (1.5, CI: 1.3–1.8). The revision risk was similar for MoM THA and MoP THA in men who were 60 years old or more.
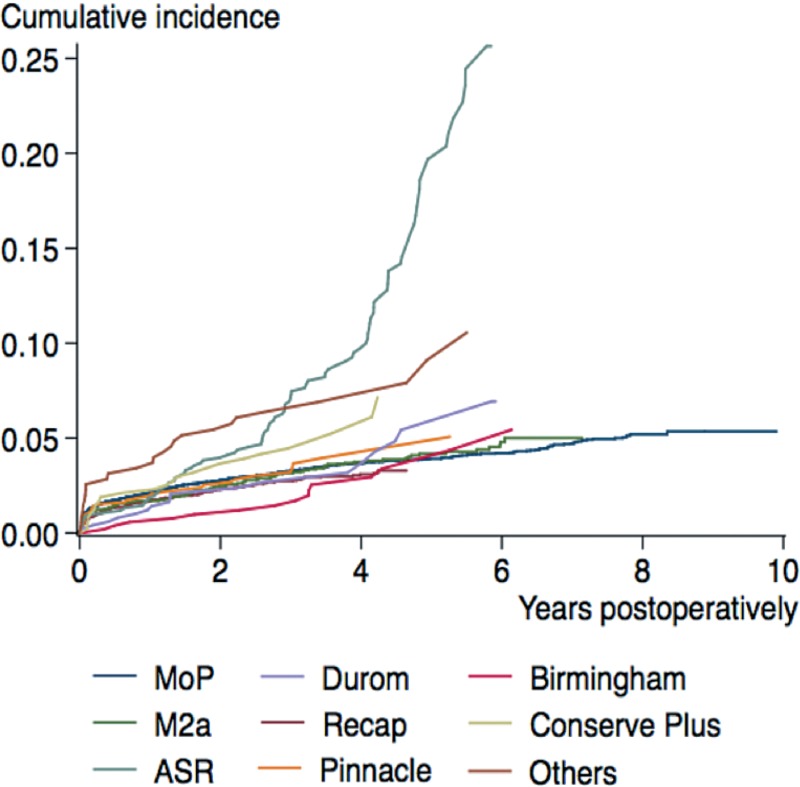
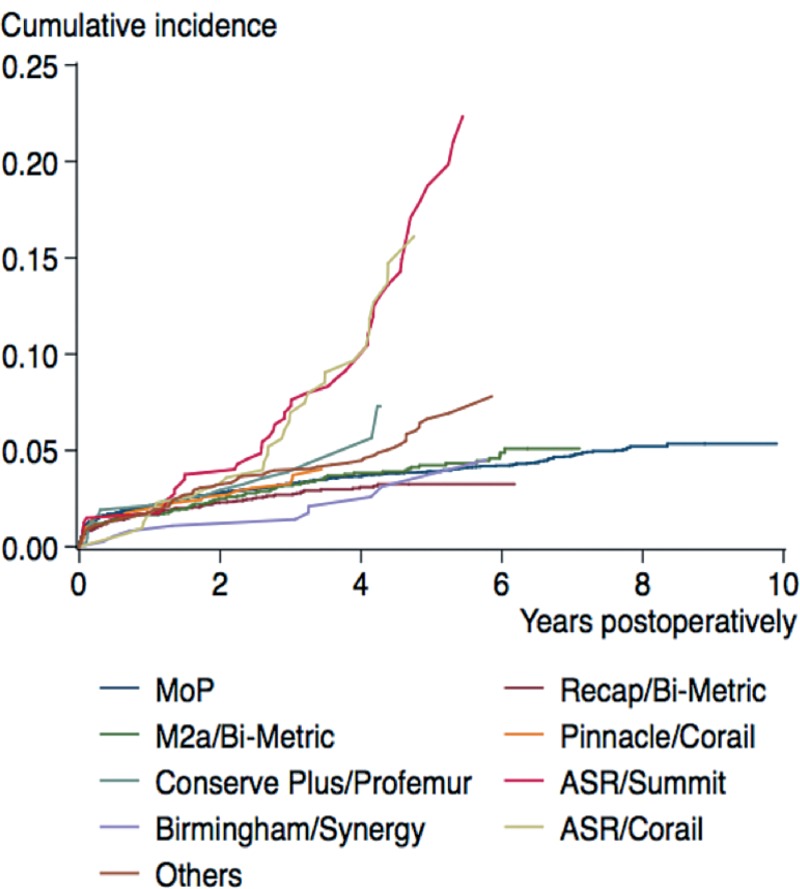
For different designs of acetabular components in MoM THAs at 6-year follow-up, the RR of revision for any reason was higher for the ASR cup, for the Conserve Plus cup, and for “other” designs of cups than for the cups used in all the MoP THAs (Figure 3 and Table 3, see Supplementary data). The MoM cup/stem combinations of ASR/Summit, ASR/Corail, and “other” had statistically significantly higher RR of revision for any reason than MoP THAs in general (Figure 4 and Table 3, see Supplementary data). When comparing acetabular components in the MoM group with the most frequently used as reference (Recap), the ASR, Conserve Plus, and “other” cups had significantly higher revision risk at 6-year follow-up (Table 4, see Supplementary data). In the cementless stemmed MoM THAs, the cup and stem combinations of M2a/Bi-Metric, ASR/Summit, ASR/Corail, and other combinations of components had significantly higher RR of revision for any reason than the Recap/Bi-Metric combination (Table 4, see Supplementary data).
Figure 3.
Cumulative incidence for revision (for any reason) of metal-on-polyethylene (MoP) total hip arthroplasty (THA) and specific designs of cementless acetabular components in stemmed THA with metal-on-metal bearings.
Figure 4.
Cumulative incidence for revision (for any reason) of metal-on-polyethylene (MoP) total hip arthroplasty (THA) and combinations of specific designs of cementless acetabular and femoral components in stemmed THA with metal-on-metal bearings.
For Pinnacle, 75% had femoral head sizes smaller than 38 mm, and 86% of the M2a cups had femoral head sizes of 38–39 mm. For Recap, ASR, Birmingham, Durom, and Conserve Plus acetabular components, the vast majority had femoral head sizes of 44 mm or larger (95%, 93%, 87%, 87%, and 89% respectively) (Table 5, see Supplementary data). In the MoM group and with femoral head size of 38–39 mm as reference, a significantly higher RR of revision for any reason at 6 years was found for femoral head sizes between 44 and 47 mm. Other head sizes did not reach statistical significance in similar comparisons (Table 6).
Table 6.
Median follow-up and revision rate for different sizes of the femoral head used in cementless stemmed total hip arthroplasty (THA) with metal-on-metal (MoM) bearings. Crude and adjusted relative risk (RR) of revision for any reason with 95% confidence intervals (CIs) at 6-year follow-up
| No.(%) | Median follow-up (IQR) | Any revision (n) | Risk time, years | Revision rate per 100 years (95% CI) | Crude RR >(95% CI) | Adjusted RR (95% CI) | |
|---|---|---|---|---|---|---|---|
| All MoM THAs | |||||||
| ≤ 37 | 949 (8) | 3.3 (2.2–4.3) | 46 | 3,313 | 1.39 (1.04–1.85) | 1.48 (0.98–2.25) | 1.48 (0.95–2.32) |
| 38–39 | 2,317 (20) | 4.9 (3.3–6.1) | 93 | 10,673 | 0.87 (0.71–1.07) | 1 (ref.) | 1 (ref.) |
| 40–43 | 679 (6) | 3.0 (2.1–4.3) | 20 | 2,189 | 0.91 (0.59–1.42) | 1.07 (0.65–1.77) | 1.14 (0.65–2.02) |
| 44–47 | 2,431 (21) | 3.4 (2.3–4.5) | 128 | 8,443 | 1.52 (1.27–1.80) | 1.77 (1.27–2.48) | 1.68 (1.17–2.40) |
| 48–51 | 3,124 (27) | 3.3 (2.3–4.5) | 108 | 10,668 | 1.01 (0.84–1.22) | 1.27 (0.90–1.80) | 1.38 (0.93–2.04) |
| ≥ 52 | 2,067 (18) | 3.2 (2.3–4.4) | 75 | 6,917 | 1.08 (0.86–1.36) | 1.14 (0.79–1.62) | 1.33 (0.92–1.93) |
| MoM THAs after exclusion of patients having the ASR acetabular component | |||||||
| ≤ 37 | 938 (9) | 3.3 (2.2–4.3) | 45 | 3,257 | 1.38 (1.03–1.85) | 1.38 (0.91–2.08) | 1.40 (0.90–2.19) |
| 38–39 | 2,314 (21) | 4.9 (3.3–6.1) | 93 | 10,661 | 0.87 (0.71–1.07) | 1 (ref.) | 1 (ref.) |
| 40–43 | 643 (6) | 3.0 (2.1–4.2) | 15 | 2,049 | 0.73 (0.44–1.21) | 0.74 (0.44–1.26) | 0.75 (0.42–1.32) |
| 44–47 | 2,136 (20) | 3.4 (2.3–4.4) | 83 | 7,302 | 1.14 (0.92–1.41) | 1.06 (0.76–1.49) | 1.00 (0.68–1.48) |
| 48–51 | 2,866 (26) | 3.3 (2.3–4.4) | 75 | 9,696 | 0.77 (0.62–0.97) | 0.83 (0.58–1.18) | 0.90 (0.59–1.39) |
| ≥ 52 | 1,918 (18) | 3.2 (2.2–4.3) | 59 | 6,365 | 0.93 (0.72–1.20) | 0.83 (0.58–1.19) | 0.97 (0.66–1.43) |
Causes of revision
The cementless MoM THAs had a higher proportion of revisions due to aseptic loosening (p < 0.001) and “other” causes (p = 0.03). We found a lower frequency of revision due to dislocation for MoM THA than for MoP THA, irrespective of femoral head size (p < 0.001). At 6-year follow-up, the RR of revision due to dislocation was lower for MoM bearings than for MoP bearings (0.27, CI: 0.19–0.39), but the RR of revision due to aseptic loosening (5.5, CI: 3.8–7.9) and all other causes of revision (1.2, CI: 1.0–1.5) was higher for MoM bearings than for MoP bearings (Table 7, see Supplementary data).
For patients with the ASR acetabular component, 10% (75 of 759 patients) had revision surgery because of aseptic loosening, 1.3% (10 of 759 patients) had revision because of deep infection, and 0.9% (7 of 759 patients) had revision because of pain.
Exclusion of the ASR acetabular component
After exclusion of 759 patients with the ASR acetabular component, the cumulative incidence of revision for MoM THA at 8-year follow-up was 5.0% (CI: 4.3–5.8). Comparing MoM THA with MoP THA, the adjusted RR of revision for any reason at 6-year follow-up was 1.1 (CI: 0.97–1.3). Repeated analysis with different femoral head sizes did not show any significant difference in RR of revision for any reason at 6-year follow-up for any head size compared to 38–39 mm (Table 6).
Discussion
In this population-based study from the NARA database, the RR of revision for any reason at 6 years of follow-up was 49% higher for MoM THA than for MoP THA, whereas the RR of revision for any reason was similar for both after exclusion of ASR acetabular components. There was a high risk of revision with prosthetic design combinations of ASR/Summit and ASR/Corail relative to MoP THA. In all patients with MoM THA, we found a higher risk of revision for femoral head sizes between 44 and 47 mm than for a femoral head size of 38–39 mm.
Risk of revision for any reason
In the Australian Orthopaedic Association National Joint Replacement Registry (AOA NJRR), the cumulative percentage of revision of MoM THA was 9.6 (CI: 9.2–10.0) at 5 years and 15.5 (CI: 14.8–16.2) at 10 years (Australian Orthopaedic Association 2013), which is more than the cumulative incidence of revision at 8 years found in our study. The lower incidence found by us could be due to differences in the use of specific component designs. In the present study, the Recap constituted 47% of all acetabular components in the MoM group and the ASR only 7% of them, whereas the ASR cup was used far more frequently in Australia. In contrast, the Recap cup with the second lowest revision rate at 7 years was used to a lesser extent (Australian Orthopaedic Association 2013). In both the NARA database and the AOA NJRR, the ASR cup had the highest cumulative incidence of revision but was used with different frequency, which could explain the different revision rates in these 2 registries. A study from the National Joint Registry of England and Wales (Smith et al. 2012) excluded the ASR implants from the analysis and found an overall 5-year revision rate of 6.2% (CI: 5.8–6.6) for MoM THA, which was higher than the 8-year cumulative revision rate found in our study after exclusion of the ASR implant. This could also be caused by differences in use of certain component designs and implant combinations, and also differences in follow-up and surgical technique.
Stratified analyses: risk of revision for any reason
We found that the cumulative incidence of revision of the ASR acetabular component increased to more than 25% at 5.8 years. The ASR cup had similar cumulative incidence of revision in the AOA NJRR, and Langton et al. (2011) found a 6-year failure rate of 48.8% for the ASR cup used with a conventional stem. In a recent study, the cumulative 7-year survivorship was 38% (CI: 33–44) for MoM THA with the ASR cup with femoral head sizes smaller than 50 mm. The most common cause of revision was ARMD, accounting for 86% of revisions, and use of the Corail stem had an increased risk of ARMD (Reito et al. 2013). Although we have no information of the presence of ARMD in our study, patients with the ASR/Summit combination had a much higher cumulative incidence of revision than patients with the ASR/Corail combination, which may be explained by the shorter follow-up for ASR/Corail. In the present study, ASR components were mainly revised due to aseptic loosening.
The acetabular component with the best survivorship in our study was the Recap cup, with a cumulative incidence of revision of 3.4% (CI: 2.8–4.0) at 6-year follow-up. This is slightly better than reported in Australia, where the Recap acetabular component had the lowest cumulative incidence of revision (6.3%, CI: 4.4–8.9) at 7 years among monobloc cups (Australian Orthopaedic Association 2013). In a recent study with a small series of Recap/M2a-magnum LDH MoM THAs including 80 hips with a mean follow-up of 6 years, 11 hips were considered to have definite ARMD, and revision had been performed in 3 of these cases (Mokka et al. 2013a). Another 32 hips were considered to have probable or possible ARMD. This indicates a high prevalence of ARMD in patients with the Recap cup after medium-term follow-up, with the possible consequence of increasing revision rates due to metal-related pathology with longer follow-up.
The Pinnacle acetabular component was the only non-monobloc cup analyzed separately when we performed stratified analyses. The cumulative incidence of revision of the Pinnacle cup of 5.1% (CI: 2.9–8.2) found in our study at 5 years of follow-up was similar to that found in Australia where the 5-year revision risk was 3.9% (CI: 2.2–7.0) for Pinnacle/S-Rom and 4.6% (CI: 3.6–5.8) for Pinnacle/Articul-Eze (Australian Orthopaedic Association 2013). In England and Wales, the 5-year revision rate following Pinnacle/Corail cementless THA with MoM bearings was 4.2% (99% CI: 2.3–6.0) (Jameson et al. 2013). The adjusted hazard rate of revision for this implant combination was 1.9 (99% CI: 1.4–2.7) when compared to MoP bearings (Jameson et al. 2013). In the present study, the RR of revision of the Pinnacle/Corail MoM THA was similar to that of MoP THA.
Femoral head size is a major risk factor for revision of MoM THA, with increasing revision rates with increasing head size (Graves et al. 2011, Smith et al. 2012, Australian Orthopaedic Association 2013). When we compared MoM THA with different femoral head sizes to MoM THA with 38- to 39-mm heads, the RR of revision for any revision was statistically significantly higher for head sizes of 44–47 mm. This femoral head size was the most prevalent with the ASR cup. After exclusion of patients with the ASR implant, only femoral head sizes smaller than 38 mm had higher RR of revision than head sizes of 38–39 mm, and the larger head sizes had similar or even lower RR of revision when compared to 38–39 mm—although the differences were not significant. As the Pinnacle cup had the majority of the smallest head sizes and revision risk changed when the ASR implant was excluded, it appears that component design is an important factor when interpreting revision risk with different femoral head sizes in MoM THA.
Causes of revision
The most common cause of revision of MoM THA at 8 years of follow-up in Australia was metal-related pathology, followed by aseptic loosening and infection for femoral head sizes larger than 32 mm (Australian Orthopaedic Association 2013). It is not possible to identify revisions performed for “metal-related pathology” in the NARA database, but it is possible that some of these MoM-bearing complications are registered as revisions performed for “other” reasons. In the study from the National Joint Registry of England and Wales, the most common reason for revision of cementless stemmed MoM THA was aseptic loosening (Smith et al. 2012). In our study, the frequency of revision due to aseptic loosening and “other” causes was higher for MoM THA than for MoP THA. The frequency and RR of revision due to dislocation was, however, lower for MoM bearings than for MoP bearings. In a recent study from the Finnish Arthroplasty Register, the RR of revision due to dislocation was 0.09 (CI: 0.05–0.17) for head sizes larger than 36 mm compared to 28 mm (Kostensalo et al. 2013). Thus, the low risk of revision of MoM THA due to dislocation might be explained by the fact that MoM THAs in that study mainly had head sizes larger than 37 mm.
Methodological considerations
Some strengths of the present study were the population-based design with prospective collection of data and a large sample size. The complete follow-up of the study population limited possible selection bias. The study also had several limitations that should be considered when interpreting the results. The exclusion of 1,712 patients—who could have had either MoM or MoP bearings but were registered without unambiguous information on bearings—may have led to information bias. We analyzed the 2 worst-case scenarios by assuming that all 1,712 THAs had received either MoM or MoP bearings. Inclusion of all 1,712 THAs in the MoM group gave an adjusted RR of revision for any reason at 6-year follow-up of 1.4 (CI: 1.3–1.6) for MoM THA vs. MoP THA. Inclusion of all 1,712 THAs in the MoP group gave an adjusted RR of revision for any reason at 6-year follow-up of 1.4 (CI: 1.3–1.6) for MoM THA vs. MoP THA. Thus, in both cases, the risk of revision would have been higher for MoM bearings than for MoP bearings, as was found after exclusion of the patients. The exclusion of the 48 patients with unregistered information on diagnosis or femoral head size can be assumed to have had no influence on the results of the study, due to the large study population.
The distribution of THAs with MoM and MoP bearings varied between countries. Finland and Denmark contributed the majority of MoM THAs, and Sweden and Denmark contributed the majority of MoP THAs. From previous studies (Havelin et al. 2009, Makela et al. 2014), we know that there is variation in outcome in terms of implant survival between the Nordic countries, which may in part be caused by differences in demography and implant selection. Most of the implants included in this study were, however, used in several countries. We also adjusted for sex, age, and diagnosis, and performed subanalyses on specific implants. Even so, any differences between countries caused by factors that not were captured in the NARA database could have influenced our results, but it was not our aim to evaluate differences between countries. Since the healthcare systems, patient populations, and treatment traditions in the Nordic countries are rather homogenous, we believe that any influence of skewed inclusion of patients from the countries involved in this study would be small.
Although we adjusted for several confounders, there is still the possibility of unidentified confounding. The regression model used to compare MoM THA with MoP THA did not include adjustment for femoral head size, despite the fact that it is a well-documented risk factor (Smith et al. 2012, Australian Orthopaedic Association 2013): As 92% of MoM THAs had femoral head sizes greater than 37 mm and 97% of MoP THAs had head sizes smaller than 38 mm, femoral head size could be considered to be a proxy for the bearings used in THA, and it was therefore not adjusted for in the model. Furthermore, the NARA database does not contain any information on potential confounders such as blood concentrations of chromium and cobalt, comorbidity, height, weight, BMI, or physical activity before or after surgery. In addition, we had no information from any radiographic examinations or magnetic resonance imaging, either for revised or unrevised hips, and we could not account for silent, unrevised metal reactions.
Another limitation was the short follow-up, resulting in a high proportion of revisions due to surgical and technical errors. Registry studies are unable to detect silent, unrevised metal reactions, and with longer follow-up, a change in causes of revision may result in an increased proportion of revisions related to mechanical wear and ARMD. Also, the number of revisions was low, and the sensitivity to random effects of single revision cases could thereby be increased when performing stratified analyses. Furthermore, the revision causes registered have not been validated in the national registries contributing to the NARA database, and revisions due to “metal-related pathology” such as ARMD have not been registered.
Conclusion
We found a higher RR of revision for any reason at 6-year follow-up for MoM THA than for MoP THA, but after exclusion of patients with the ASR acetabular component, the risk of revision was similar between the 2 groups of bearings. At 6-year follow-up, there was a much higher risk of revision with prosthetic design combinations of ASR/Summit and ASR/Corail than for MoP THA, whereas the risk of revision was similar for the Recap/Bi-Metric combination and for MoP THA. In MoM THA, we found a higher risk of revision for femoral head sizes between 44 and 47 mm than for 38–39 mm. After exclusion of patients with the ASR acetabular component, the risk of revision was similar for different femoral head sizes in MoM THA.
We recommend that stemmed LDH MoM bearings should not be used until further studies with longer follow-up are performed to identify the risk of complications.
Supplementary data
Tables 2–5, and 7 are available at Acta’s website (www.actaorthop.org), identification number 7928.
Acknowledgments
The study idea was conceived by CV, ABP, KM, and SO. All the authors contributed to the development and design of the study. ABP collected the data. Analyses were directed by CV, ABP, JK, and SO and were performed by CV. All the authors participated in interpretation and discussion of the results. CV wrote the initial draft of the manuscript. All the authors critically revised the manuscript for intellectual content.
No competing interest declared.
References
- Australian Orthopaedic Association. National Joint Replacement Registry, Metal on Metal Total Conventional Hip Arthroplasty, Supplementary Report 2013. 2013.
- Burroughs BR, Hallstrom B, Golladay GJ, Hoeffel D, Harris WH. Range of motion and stability in total hip arthroplasty with 28-, 32-, 38-, and 44-mm femoral head sizes . J Arthroplasty. 2005;20(1):11–9. doi: 10.1016/j.arth.2004.07.008. [DOI] [PubMed] [Google Scholar]
- Daley B, Doherty AT, Fairman B, Case CP. Wear debris from hip or knee replacements causes chromosomal damage in human cells in tissue culture . J Bone Joint Surg (Br) 2004;86(4):598–606. [PubMed] [Google Scholar]
- Davis KE, Ritter MA, Berend ME, Meding JB. The importance of range of motion after total hip arthroplasty . Clin Orthop Relat Res. 2007;465:180–4. doi: 10.1097/BLO.0b013e31815c5a64. [DOI] [PubMed] [Google Scholar]
- DePuy Companies. DePuy ASR™ Hip Implant Recall Guide. 2013.
- Furnes O, Paxton E, Cafri G, Graves S, Bordini B, Comfort T, Rivas MC, Banerjee S, Sedrakyan A. Distributed analysis of hip implants using six national and regional registries: comparing metal-on-metal with metal-on-highly cross-linked polyethylene bearings in cementless total hip arthroplasty in young patients . J Bone Joint Surg (Am) 2014;96(Suppl 1):25–33. doi: 10.2106/JBJS.N.00459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gillam MH, Ryan P, Graves SE, Miller LN, de Steiger RN, Salter A. Competing risks survival analysis applied to data from the Australian Orthopaedic Association National Joint Replacement Registry . Acta Orthop. 2010;81(5):548–55. doi: 10.3109/17453674.2010.524594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graves SE, Rothwell A, Tucker K, Jacobs JJ, Sedrakyan A. A multinational assessment of metal-on-metal bearings in hip replacement . J Bone Joint Surg (Am) 2011;93(Suppl 3):43–7. doi: 10.2106/JBJS.K.01220. [DOI] [PubMed] [Google Scholar]
- Havelin LI, Engesaeter LB, Espehaug B, Furnes O, Lie SA, Vollset SE. The Norwegian Arthroplasty Register: 11 years and 73,000 arthroplasties . Acta Orthop Scand. 2000;71(4):337–53. doi: 10.1080/000164700317393321. [DOI] [PubMed] [Google Scholar]
- Havelin LI, Fenstad AM, Salomonsson R, Mehnert F, Furnes O, Overgaard S, Pedersen AB, Herberts P, Karrholm J, Garellick G. The Nordic Arthroplasty Register Association: a unique collaboration between 3 national hip arthroplasty registries with 280,201 THRs . Acta Orthop. 2009;80(4):393–401. doi: 10.3109/17453670903039544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herberts P, Ahnfelt L, Malchau H, Stromberg C, Andersson GB. Multicenter clinical trials and their value in assessing total joint arthroplasty . Clin Orthop Relat Res. 1989;249:48–55. [PubMed] [Google Scholar]
- Huang DC, Tatman P, Mehle S, Gioe TJ. Cumulative revision rate is higher in metal-on-metal THA than metal-on-polyethylene THA: analysis of survival in a community registry . Clin Orthop Relat Res. 2013;471(6):1920–5. doi: 10.1007/s11999-013-2821-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobs JJ, Shanbhag A, Glant TT, Black J, Galante JO. Wear debris in total joint replacements . J Am Acad Orthop Surg. 1994;2(4):212–20. doi: 10.5435/00124635-199407000-00004. [DOI] [PubMed] [Google Scholar]
- Jameson SS, Baker PN, Mason J, Rymaszewska M, Gregg PJ, Deehan DJ, Reed MR. Independent predictors of failure up to 7.5 years after 35 386 single-brand cementless total hip replacements: A retrospective cohort study using National Joint Registry data . Bone Joint J. 2013;95-B(6):747–57. doi: 10.1302/0301-620X.95B6.31378. [DOI] [PubMed] [Google Scholar]
- Klein JP, Logan B, Harhoff M, Andersen PK. Analyzing survival curves at a fixed point in time . Stat Med. 2007;26(24):4505–19. doi: 10.1002/sim.2864. [DOI] [PubMed] [Google Scholar]
- Kostensalo I, Junnila M, Virolainen P, Remes V, Matilainen M, Vahlberg T, Pulkkinen P, Eskelinen A, Makela KT. Effect of femoral head size on risk of revision for dislocation after total hip arthroplasty: a population-based analysis of 42,379 primary procedures from the Finnish Arthroplasty Register . Acta Orthop. 2013;84(4):342–7. doi: 10.3109/17453674.2013.810518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Langton DJ, Jameson SS, Joyce TJ, Hallab NJ, Natu S, Nargol AV. Early failure of metal-on-metal bearings in hip resurfacing and large-diameter total hip replacement: A consequence of excess wear . J Bone Joint Surg (Br) 2010;92(1):38–46. doi: 10.1302/0301-620X.92B1.22770. [DOI] [PubMed] [Google Scholar]
- Langton DJ, Jameson SS, Joyce TJ, Gandhi JN, Sidaginamale R, Mereddy P, Lord J, Nargol AV. Accelerating failure rate of the ASR total hip replacement . J Bone Joint Surg (Br) 2011;93(8):1011–6. doi: 10.1302/0301-620X.93B8.26040. [DOI] [PubMed] [Google Scholar]
- Langton DJ, Sidaginamale R, Lord JK, Nargol AV, Joyce TJ. Taper junction failure in large-diameter metal-on-metal bearings . Bone Joint Res. 2012;1(4):56–63. doi: 10.1302/2046-3758.14.2000047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lucht U. The Danish Hip Arthroplasty Register . Acta Orthop Scand. 2000;71(5):433–9. doi: 10.1080/000164700317381081. [DOI] [PubMed] [Google Scholar]
- Makela KT, Matilainen M, Pulkkinen P, Fenstad AM, Havelin LI, Engesaeter L, Furnes O, Overgaard S, Pedersen AB, Karrholm J, Malchau H, Garellick G, Ranstam J, Eskelinen A. Countrywise results of total hip replacement. An analysis of 438,733 hips based on the Nordic Arthroplasty Register Association database . Acta Orthop. 2014;85(2):107–16. doi: 10.3109/17453674.2014.893498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mokka J, Junnila M, Seppanen M, Virolainen P, Polonen T, Vahlberg T, Mattila K, Tuominen EK, Rantakokko J, Aarimaa V, Kukkonen J, Makela KT. Adverse reaction to metal debris after ReCap-M2A-Magnum large-diameter-head metal-on-metal total hip arthroplasty . Acta Orthop. 2013a;84(6):549–54. doi: 10.3109/17453674.2013.859419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mokka J, Makela KT, Virolainen P, Remes V, Pulkkinen P, Eskelinen A. Cementless Total Hip Arthroplasty with Large Diameter Metal-on-Metal Heads: Short-Term Survivorship of 8059 Hips from the Finnish Arthroplasty Register . Scand J Surg. 2013b;102(2):117–23. doi: 10.1177/1457496913482235. [DOI] [PubMed] [Google Scholar]
- National Joint Registry for England and Wales. 8th annual report. 2011. pp. 133–4.
- Pandit H, Glyn-Jones S, Lardy-Smith P, Gundle R, Whitwell D, Gibbons CL, Ostlere S, Athanasou N, Gill HS, Murray DW. Pseudotumours associated with metal-on-metal hip resurfacings . J Bone Joint Surg (Br) 2008;90(7):847–51. doi: 10.1302/0301-620X.90B7.20213. [DOI] [PubMed] [Google Scholar]
- Parner ET, Andersen PK. Regression analysis of censored data using pseudo-observations. Stata Journal. 2010;10(3):408–22. [Google Scholar]
- Penny JO, Ovesen O, Varmarken JE, Overgaard S. Similar range of motion and function after resurfacing large-head or standard total hip arthroplasty . Acta Orthop. 2013;84(3):246–53. doi: 10.3109/17453674.2013.788435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Puolakka TJ, Pajamaki KJ, Halonen PJ, Pulkkinen PO, Paavolainen P, Nevalainen JK. The Finnish Arthroplasty Register: report of the hip register . Acta Orthop Scand. 2001;72(5):433–41. doi: 10.1080/000164701753532745. [DOI] [PubMed] [Google Scholar]
- Ranstam J, Karrholm J, Pulkkinen P, Makela K, Espehaug B, Pedersen AB, Mehnert F, Furnes O. Statistical analysis of arthroplasty data II. Guidelines . Acta Orthop. 2011;82(3):258–67. doi: 10.3109/17453674.2011.588863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reito A, Puolakka T, Elo P, Pajamaki J, Eskelinen A. High prevalence of adverse reactions to metal debris in small-headed ASR hips . Clin Orthop Relat Res. 2013;471(9):2954–61. doi: 10.1007/s11999-013-3023-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith AJ, Dieppe P, Vernon K, Porter M, Blom AW. Failure rates of stemmed metal-on-metal hip replacements: analysis of data from the National Joint Registry of England and Wales . Lancet. 2012;379(9822):1199–204. doi: 10.1016/S0140-6736(12)60353-5. [DOI] [PubMed] [Google Scholar]
- Willert HG, Buchhorn GH, Fayyazi A, Flury R, Windler M, Koster G, Lohmann CH. Metal-on-metal bearings and hypersensitivity in patients with artificial hip joints. A clinical and histomorphological study . J Bone Joint Surg (Am) 2005;87(1):28–36. doi: 10.2106/JBJS.A.02039pp. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.