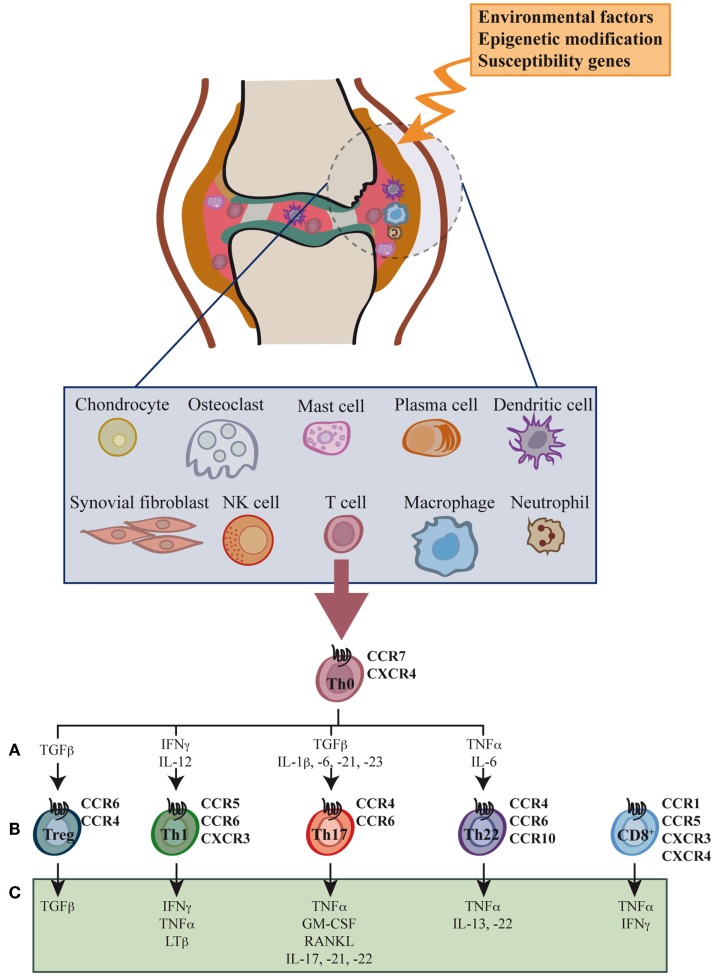
Figure 1.
Cell types, cytokines, and chemokine receptors involved in rheumatoid arthritis development. Environmental factors and susceptibility gene interactions promote loss of tolerance to citrullinated self proteins generated by post-translational modifications. Co-stimulation-dependent interactions among DCs, T cells, and B cells generate an autoimmune response to these self proteins. This inflammatory process occurs primarily in the lymph node, but also in the inflamed joint. Adaptive and innate immune cells are attracted to the joint where immune pathways integrate to promote tissue remodeling and damage. Positive feedback loops mediated by interactions among leukocytes, synovial fibroblasts, chondrocytes, and osteoclasts, together with the molecular products of damage, drive the chronic phase in rheumatoid arthritis (RA) pathogenesis. High levels of activated memory CD4+ and CD8+ T cells differentiated through cytokine stimulation of naïve cells infiltrate the synovia (A). RA was classically considered a type 1 T helper (Th1)-mediated disease, but today data indicate that type 17 T helper cells (Th17) are more important in its promotion. Evidence shows that type 22 T helper cells (Th22) also contribute to RA pathogenesis. Function of regulatory T cells (Treg) is also reduced and effector cell resistance to suppression thus helps to alter the immune balance in inflamed joints. The figure shows the chemokine receptor expression pattern (B) and the main secreted cytokines (C) associated with each T cell subtype.