Figure.
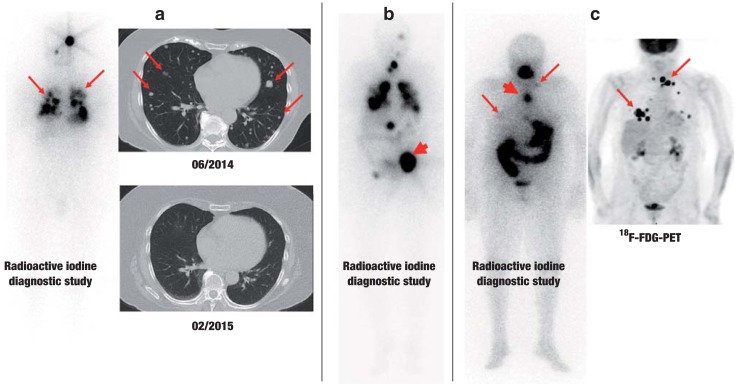
Three illustrative cases of patients with metastatic thyroid carcinoma.
a) Follicular thyroid carcinoma with very good radioactive iodine uptake (left). One year after radioactive iodine therapy, CT reveals only slight evidence of possible residual tumor at the site of the original pulmonary metastases (arrows).
b) Follicular thyroid carcinoma with metastases to bone, lungs, and mediastinum. Scintigraphy after radioactive iodine therapy reveals marked radioactive iodine uptake in all of the metastases. A large, osteolytic metastasis to the pelvis (arrow) was additionally treated with external beam radiotherapy, because, despite marked uptake of radioactive iodine, this form of treatment alone die not yield a sufficient radiation dose.
c) Poorly differentiated thyroid carcinoma. The whole-body radioactive iodine diagnostic study (left) reveals a mediastinal lymph-node metastasis with marked uptake (thick arrow), but without any correlate in the FDG-PET (right). In contrast, the supraclavicular lymph nodes take up large amounts of FDG, but hardly any radioactive iodine (thin arrows).
Standard imaging studies in thyroid carcinoma include ultrasonography of the neck and radioactive iodine scintigraphy (once or twice), and, in some advanced cases, tomographic imaging and FDG-PET.
CT, computerized tomography; FDG, fluorodeoxyglucose; FDG-PET, fluorodeoxyglucose positron emission tomography.