Abstract
Pharmacy practice is still in the initial stages of development in India, but launching of Doctor of Pharmacy (PharmD) study program has brought serious discussions about clinical pharmacy in the country. As the profession is in budding stage in the country, the patients, physicians, nurses, other healthcare providers, recruiters in pharmaceutical industries, prospective students, and their parents have numerous questions about this profession and study course. The objective of this article is to create awareness about clinical pharmacy services (CPS) and to introduce the role of clinical pharmacists (CPs). After reading this article, one will know about the usefulness of CPs in the Indian healthcare system against the current flaws in the system. The article describes the role of CPs in the hospitals, in research, in pharmaceutical/contract research companies, in community service and it also tells about the related myths and facts. Prospective job opportunities for CPs, present challenges and the possible solutions are elaborated as well. In conclusion, CPs are going to be the major support to the Indian healthcare system in near future; the reasons being (1) CPS are beneficial in many ways to improve healthcare; CPS have already proved their importance in western countries (2) India was never officially and efficiently exposed to CPS; so launching of CPS shall revolutionize the country's healthcare scenario.
KEY WORDS: Clinical pharmacists, clinical pharmacy services, Doctor of Pharmacy, India, Master of Pharmacy (Pharmacy Practice)
India has launched Doctor of Pharmacy (PharmD) study program in the year 2008, and it has sprouted huge discussions about both, the program and the role of clinical pharmacists (CPs) in the country. Before launching of the study program (i.e. PharmD), the role of a pharmacist in the nation was mostly considered to be “dispensing/manufacturing/marketing of the drugs” and clinical pharmacy education was mostly given under the study program of Master of Pharmacy (M. Pharm) (Pharmacy Practice/Clinical Pharmacy). Furthermore, there had been “almost no” professional clinical pharmacy services (CPS) provided in the country. As a consequence, the concepts of CP and PharmD are quite new in India.[1] Here, we have predicted the benefits of CPs and CPS in Indian healthcare system on the grounds of current healthcare scenario. The article reveals few things about Indian healthcare system that might not be easily acceptable to many healthcare providers in India or they may be totally new to many. However, as far as the Indian healthcare scenario is considered, these conditions stand true and factual. At first, it is important to understand the role of CPs in Indian healthcare system.
Role of Clinical Pharmacists in Hospital
Clinical pharmacists have a valuable role in the hospital. Table 1 gives details of different CPS:
Table 1.
CPS and their comparison to the current Indian healthcare system
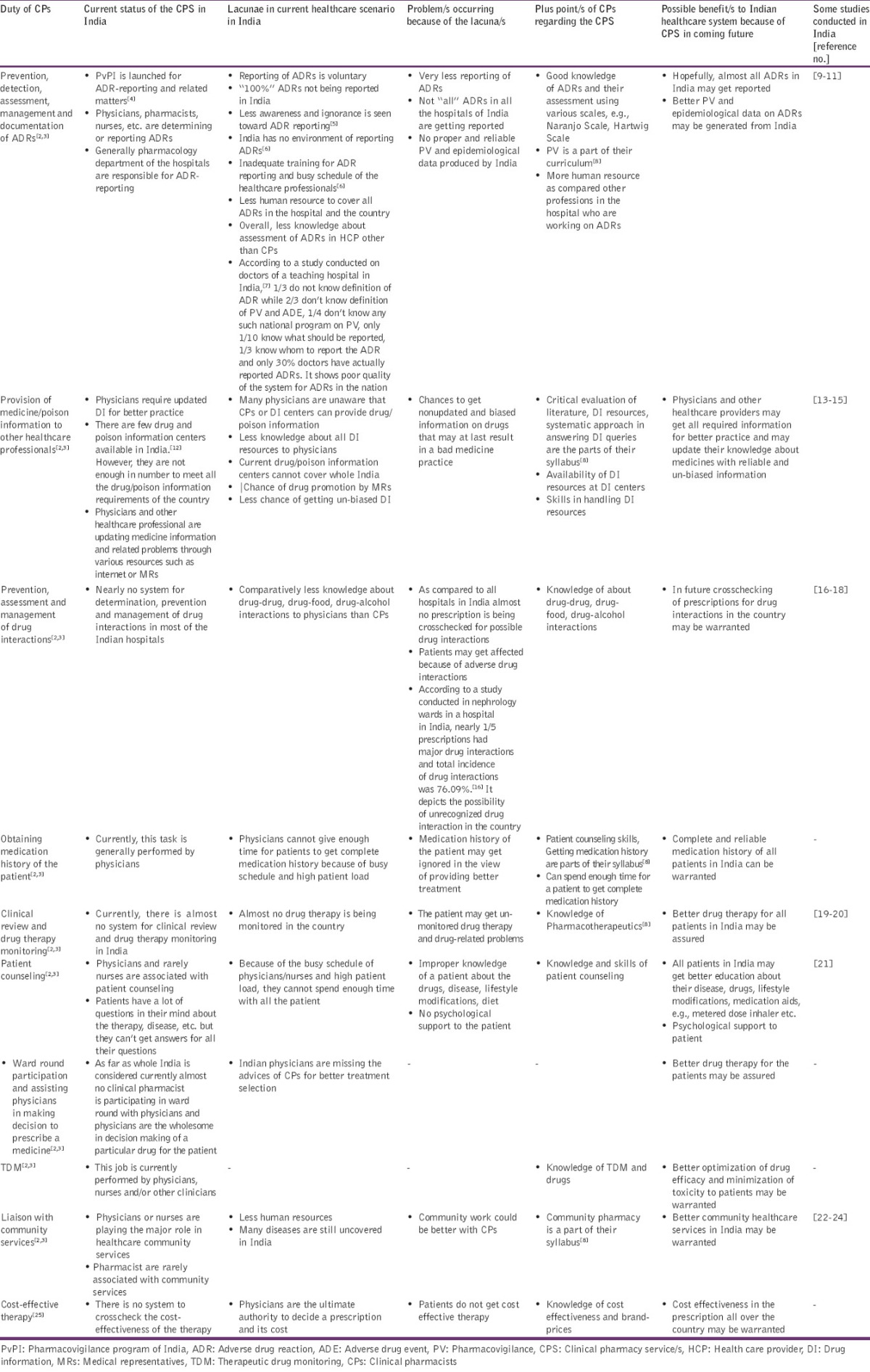
Current status of that particular CPS
Lacunae in current healthcare scenario
Problems occurring because of the lacunae
Plus points of CPs associated with the CPS
Possible benefits of CPS to Indian healthcare system in near future
Evidences of research conducted from India.
We have given the evidences of the research work in the last column of the table; through this we just want to say that such research work is “possible” in India. There are many such research works conducted in India. The remaining points relevant to CPS that are not covered in Table 1 are discussed below; so readers are kindly requested to go through the table before reading further. Unfortunately, there is no nationwide official system for the provision of CPS at present.
Provision of drug and poison information
Nowadays, various electronic databases and drug information softwares are used for the provision of unbiased and latest medicine/poison information in the western world. Such softwares/databases give easy, quick and updated information about drugs/poisons. Some good examples include - MICROMEDEX™, Clinical Pharmacology™ (by Elsevier), Medscape™, etc. Further to add, their mobile and apps are also available for quick information related to medicine.[26,27] There is much scope to use such drug information tools in Indian set-up. The tools can also be used to check drug interactions. The government authorities are advised to take initiative for providing such tools to educational institutes and drug information centers.
Medication history interview
Accurate medication history of the patient is important to assess − the medical concordance, rationale for the drugs prescribed previously, patient understanding toward medicines, evidence for drug abuse, patient acceptance for the treatment, documenting allergies and adverse drug reactions (ADRs), etc.[2]
Clinical review
In clinical review, pharmacists have to check the drug therapy to ensure that the patient is getting the most appropriate dose, dosage, dosage form, duration of therapy for their medical/disease state. Also, he has to correlate the signs and symptoms of the patient, laboratory results, medical diagnoses and therapeutic goals with the medication history for better patient care.[2] According to Jain et al. study, medication errors are common even in neonatology.[28] The CPs can play a significant role to solve such serious issues.
Patient counseling
Patient counseling can be considered as the most important CPS from the patient's point of view. The pharmacists may provide the information about current clinical condition/proceedings of the patient and educate him about the safe and appropriate use of medicines, thereby enhancing his therapeutic outcomes.[2] Generally, there are many questions in patient's mind about disease, drugs, lifestyle modifications, diet, treatment, duration of therapy and medical devices, e.g., metered dose inhalers for asthma patients or insulin pen for diabetics. Here, the pharmacists can educate the patients about all such areas as a part of CPS.
A CP may provide information on ongoing care to the patient to ensure continuity of supply of drugs, continuity of medication concordance aids, communication of special problems, appropriate monitoring of the dosages and for minimal disruption.[2]
The patient may be counseled/educated for the following points about the drugs by the pharmacists.[2,29]
Generic name, brand name of the drug
Dosage
Indications/benefits of the medicine and expected action
Proper storage
How to take the medication?
When and how long to take medication?
Information about ceased/new medication
Special precautions about the drug
Common ADRs
Action to be taken when a dose is missed
Drugs and/or foods to be avoided.
Benefits of patient counseling include patient satisfaction, prevention of medication errors, better clinical outcomes and psychological support to the patient. Patient education especially plays an important role in chronic diseases.[24,30] The major problems in front of India include diabetes, hypertension, dyslipidemia, breast cancer etc. and patient education/counseling does matter in all such disease conditions.
Ward round participation
As a member of healthcare team, the pharmacists can attend ward rounds. The goals are improved understanding of patient's history, progress, clinical details, to provide the information on clinical aspects of patient's therapy and to improve discharge planning. The pharmacists can also help in decision-making to select the quality low-cost medicine; optimize the quality of patient care and clinical outcomes; ensure medicine selection as per formulary and local guidelines.[2]
Community pharmacy
Community pharmacy services generally involve dispensing of drugs, promotion of healthy lifestyles, support for self-care, provision of practice leaflets to the patients, medicines use review, smoking/alcohol cessation programs etc. CPs can participate in various community service programs such as smoking cessation, alcohol consumption cessation, health promotion, health nutrition, etc.[31] As community pharmacy services are not common in India or are being provided by other professionals, after implementing, it will be very much helpful for the common man of India. There is lot of scope for research in community pharmacy in India. As per Basak and Sathyanarayana, there are 30 articles available on community pharmacy based research in different journals from 1998 to 2008 from India.[32] At present, some associations are working in the area of community pharmacy.[33] Better community pharmacy services and research may be warranted in future.
Role of clinical pharmacists in research
Despite of being a highly populated country (ranking 2nd on the globe) with numerous hospitals, contribution of clinical and epidemiological research by India is not remarkable in the world. For the current contribution, Indian physicians, nurses and other healthcare providers are playing more or less roles. As the concept of clinical pharmacy is still in the initial stages of development, contribution of CPs toward the research is negligible at this point of time. On the other hand, because of the busy schedules and high patient load, physicians can’t contribute to the full of their capacity for research. As a result of this scenario, less data from the hospitals are getting published; the country lags behind other developed countries in producing quality data and research; and tremendous data from the hospitals remain unpublished in journals, e.g., rare case reports/case studies, retrospective studies etc.
Meanwhile, qualities of CPs toward the research include-presence of thesis work as a part of the syllabus, enough exposure to hospital and knowledge of subjects such as pharmacotherapeutics, clinical pharmacy, hospital pharmacy, clinical toxicology, biostatistics, research methodology, clinical pharmacokinetics, pharmacoeconomics, etc.[8] With the assistance of CPs physicians, nurses and other healthcare providers, India may come up with tremendous data published (which is now unpublished) and apart from this, presence of CPs will open new research opportunities in the country for pharmacoeconomics, clinical research, patient-reported outcomes, quality of life, pharmacovigilance, clinical pharmacokinetics etc.
The diagrammatic presentation of the hospital activities of CPs is shown in Figure 1.
Figure 1.
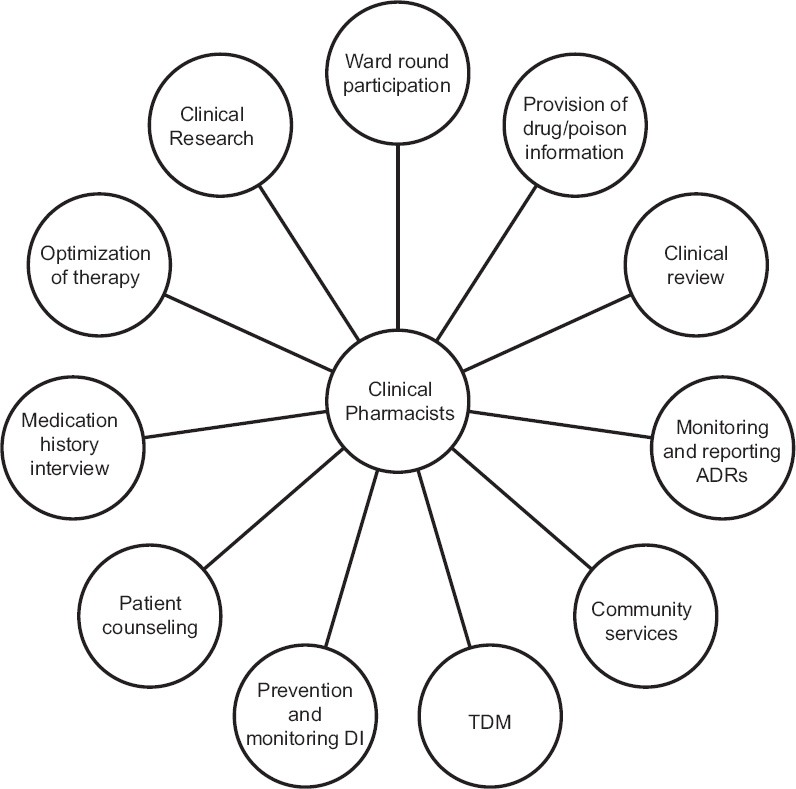
Hospital activities of clinical pharmacists (ADR: Adverse drug reactions; DI: Drug interactions; TDM: Therapeutic drug monitoring)
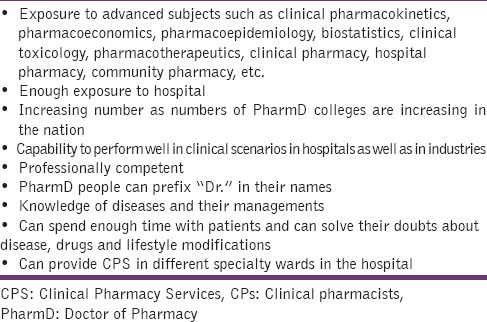
Plus points of clinical pharmacists
So, if we analyze the role of CPs, we can prognosticate the plus points of CPs as shown in Table 2.
Table 2.
Career Prospectuses and Job Opportunities for Clinical Pharmacists
A PharmD person is eligible work in all areas where a Bachelor of Pharmacy (B. Pharm) qualified student can work. Apart from this, a CP (both PharmD and M. Pharm Pharmacy Practice) can work in several other areas after completion of the course. Here, we are predicting the career prospectuses and job opportunities of CPs according to the international scenario. Though all these areas are not well-established at present in India for CPs, we believe that these areas would be open for them in near future.
In a hospital, academics and further education
As a surgeon is known for surgery, a physician is known for diagnosis and treatment of a disease; a CP would be known/recognized for providing CPs in India. Providing CPS is the first and foremost responsibility of a CP. CPs can work as a faculty member in an academic institute. They may also join a suitable teaching position in a Diploma/Degree/Postgraduate Pharmacy Institute such as lecturer, assistant professor, associate professor, professor, head of the department, head of the institution, principal or director with suitable experience.[35] At this point of time, numerous PharmD colleges are getting established in India, so both M. Pharm (Pharmacy Practice) and PharmD people have large job prospectuses in academics. As far as nonteaching hospitals are considered, currently, some elite and US-based hospitals in India are recruiting CPs. Practicing pharmacists are expected to be recruited by the government hospitals too in near future. Furthermore, CPs may have role in hospital administration team, pharmacy/therapeutic committees in hospital etc.
Higher education
The person who has completed PharmD/M. Pharm (Pharmacy Practice/Clinical Pharmacy) can register for PhD in India/abroad. After PharmD, some western countries offer specialty programs such as oncology, pharmacotherapy, nuclear pharmacy, nutrition support, psychiatry, ambulatory care, etc. Such specialty courses are not yet available in India but would be obtainable in far future.
Medical writing
This is also known as “scientific writing” or “medical communications”. Medical writing involves writing different types of healthcare documents for different purpose and for different audiences. Different types of medical literatures, their purposes and target audiences are mentioned in Figure 2. The medical writers are required in pharmaceutical/healthcare companies, contract research organizations (CROs), Business Process Outsourcing/Knowledge Process Outsourcing companies (BPOs/KPOs), healthcare communication companies, media and publishing companies, medical journals, medical societies etc., The skills needed to become a competent medical writer are: Domain knowledge, language and grammar skills, quick interpretation of medical data etc.[36] At present, there are numerous CROs, BPOs, KPOs and pharmaceutical companies in India who are hiring medical writers.
Figure 2.
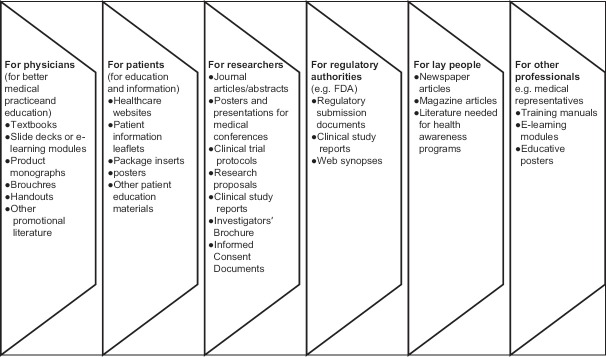
Types of medical literature with target audiences (adapted from Sharma study, 2010)[36]
Medical coding
Medical coding (also known as medical classification) is nothing but transformation of descriptions of medical diagnoses and procedures into universally acceptable codes. The codes are used in a variety of fields such as medicine, public health and medical informatics for statistical analysis, reimbursement schemes, etc.,[37] Currently, there are numerous medical coding companies in India.
Medical billing
Medical billing is different from medical coding. It is the process of translation of healthcare service into billing claim.[38] There are many health insurance companies in the nation but, to the best our knowledge, recruitment of CPs is very much rare at present. However, we project the role of CPs in medical billing as well.
Medical transcription
In simple language, medical transcription is transcribing (typing) the doctor's reports from dictated audio files. In developed countries, the health practitioner dictates what he has done after performing procedures on patient and the medical transcriptionist (MT) (also known as medical language specialist) transcribes the oral dictations and/or edits the reports. Such patient-specific health information is converted in written text document and maintained in printed, E-version or kept in patient record files. Nowadays, speech recognition softwares are used for better practice of medical transcriptions.[39]
Medical transcriptionists may be hired by the hospital or the work may be outsourced. At present, countless medical transcription companies are available in India. In current scenario, there are limited hospitals in India recruiting MTs. Skills needed to become a MT include: Sound knowledge of medical terminologies, disease conditions, anatomy, physiology, pharmacology; medical language and grammar; typing skills; effective communication skills, etc.
Pharmacovigilance
World Health Organization defines pharmacovigilance as, “the science and activities relating to the detection, assessment, understanding and prevention of adverse effects or any other drug-related problem”.[40]
Documentation, analysis and prevention of ADRs are needed for epidemiological studies and patient safety. Presently, some hospitals in India are recruiting peoples in pharmacovigilance. Various BPOs/KPOs in India are recruiting people for pharmacovigilance. Skills needed to work in the area of pharmacovigilance are: Sound knowledge of pharmacology and ADRs, laboratory results, clinical research etc.
Clinical research and drug development
Both these things are related to clinical trials. There are countless clinical research organizations present in the country. Clinical research coordinator, clinical research associate (CRAs), research statisticians and higher positions (with optimum experience) are suitable posts for CPs in clinical research organizations. CPs can even work as principal investigators[41] and patient educators in clinical trials. Pharmacists can play a role in enhancing patient participation in clinical trial research.[42] Skills needed to work clinical research organization include knowledge of statistical, medical and pharmacologic terms, pharmacovigilance, sincerity in documentation, ability to travel extensively (especially for CRAs) etc.
Forensic pharmacy
Forensic pharmacy is the field where there is application of drug-sciences to medico-legal issues. In western countries, a pharmacist can engage in legal cases related to malpractice, ADRs, drunk driving, drug abuse, healthcare fraudulence, poisoning/toxicity, and various other types of civil and criminal cases.[43] Though India has very few pharmacists working in these areas at this point of time, we believe that CPs will have future in these areas too.
Medical/clinical science liaison
Medical science liaison (MSL) is a healthcare consulting professional employed by pharmaceutical, biotechnology, medical device and managed care companies to provide unbiased (nonpromotional) information about the product. MSL:[44]
Ensures that products are utilized effectively
Serves as scientific peers and resources within the medical community
Serves as scientific experts to internal colleagues at companies.
The professionals are also known as medical liaisons/medical science managers/regional medical scientists/regional medical advisors/directors. MSL is different from medical sales representative as shown in Table 3.[45]
Table 3.
Medical sales representative vs. Medical science liaison (adapted from Bhambri et al. study, 2014)[45]
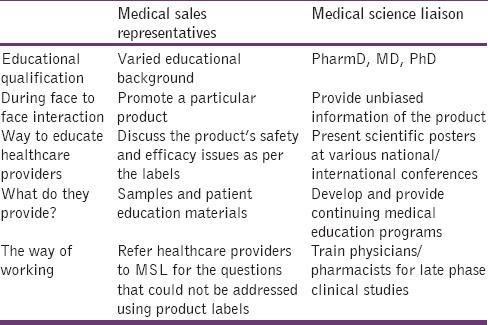
In India, MSL is an evolving, highly paid field for CPs. Important skills needed to become MSL include excellent communication and presentation skills, related therapeutic expertise, relationship building skills, ability to travel extensively, ability to train, etc.[46]
Contract research organizations
Contract research organizations are an organization that provides support to the product/device (pharmaceutical/biotechnological/medical) in the form of research services on contract basis. CPs may get absorbed in CROs working in the following fields – pharmacoeconomics, patient-reported outcomes, health technology assessment, literature reviews, systematic reviews, quality of life studies etc. All these areas are new in India but such CROs do exist in the country. Skill needed to work in CROs is excellent analytical skills, thorough knowledge of therapeutics and statistics, excellent grasping capacity, handling of databases (e.g., PubMed), etc.
Business opportunities and market research
With proper market knowledge, experience and investment, a CP can start a business with any of the ideas mentioned above. As they can analyze the comparative efficacy and unique selling property of the drugs, CPs also have a role in product management team, market research, and medico marketing.
Bioavailability/bioequivalence studies
In simple words, bioavailability (BA) is the fraction of the administered drug available in the blood circulation while bioequivalence (BE) is the comparison bioavailabilities of two pharmaceutical products with same drug and dosage. BA/BE studies are conducted for following important purposes (1) development and determination of dose and dosage form of a drug (2) quality control of drug products (3) development of new formulation of the existing drugs. The companies working in the area of BA/BE exist in India. To enter in the field of BA/BE studies, knowledge of pharmacotherapeutics, clinical pharmacokinetics and clinical research is necessary.
Public health, government sector and nongovernmental organization
Apart from community pharmacy, the pharmacists do have a role in public health. The areas and the role of pharmacists are as follows:[47]
Immunization programs: Administration and promotion of immunization
Disaster preparedness and response, e.g., natural disaster: Education of public, planning of emergency response, surveillance of notifiable syndromic conditions, communication with public, provision of mass medications, etc
Contraceptive services: Distribution of contraceptive measures and education about their use
Prevention and control of disease and injury: Promotion of healthy lifestyles, reduce hospitalizations.
In government sector and nongovernmental organizations, CPs may have a role in policy framing, drug/poison information centers, health camps, awareness programs, pharmacovigilance center, patient counseling center, etc.
Challenges and Future Directions for Clinical Pharmacists
At present, there are some challenges to CPs.
PharmD degree is “not” the basic educational requirement in India for pharmacists
PharmD is the basic educational requirement in many developed countries for pharmacists in the world but not in India E.g. USA, Pakistan etc.. Moreover, many countries are upgrading their pharmacy education from ‘industrial’ to ‘clinical’. Selected countries focusing on clinical pharmacy education are, Australia, Thailand, Tunisia, Japan etc.
Current pharmacy education system in India has many drawbacks in it such as no clinical/hospital exposure for pharmacists, entry of nonmeritorious students into the course, different syllabi for different universities, nonfocused way of learning, outdated curriculum, lack of industrial and clinical exposure, unskilled ways of practical and laboratory training, noncommercialized and poor research etc.[48,49] Futhermore, students in the institutes offering both B. Pharm and PharmD may suffer from superiority-inferiority complexes which is unhealthy.[48] India has been lacking the CPS and we feel launching of the CPs is the need of the hour in the nation. India is in great need of CPS and PharmD’fication of the country can solve this issue. PharmD’fication of all pharmacy colleges in India shall solve most of the problems in the pharmacy education system as mentioned above. PharmD’fication is the easiest, the most useful and the most appropriate solution to overcome the flaws in Indian pharmacy education. Benefits of PharmD’fication of the country are as follows:
Indian population may officially receive all CPS which India was lacking
Administration of CPS will revolutionize Indian healthcare system
PharmD offers complete knowledge of all aspects of pharmacy so PharmD degree shall help Indian pharmacists to provide professional competence
PharmD’fication may provide uniform syllabus to the pharmacists in the nation; this will minimize the judgmental approach for the quality of pharmacists based upon the institute/university
Exposure to advanced syllabus
PharmD’fication will provide global exposure for the pharmacists
Huge job opportunities may be created with PharmD’fication in the hospitals and in companies.
How to PharmD’fy the country?
Here are some strategies to PharmD’fy the country:
First and the most important thing is, making the policies. All state governments and the central government of India are requested to make the strategies to convert all B. Pharm/Diploma in Pharmacy (D. Pharm) institutes to PharmD; many countries in the world have done it
All state governments, central government, politicians, heads of the educational institutes, managing directors of the colleges are encouraged to initiate PharmD program at all colleges and universities in India
Students should demand PharmD course in the respective institute/university
Students interested to choose pharmacy as a career after 12th are encouraged to prefer PharmD over B. Pharm/D. Pharm
Huge awareness needs to be created about PharmD by all the possible ways such as distributing pamphlets, TV/radio programs, etc
Students who have completed B. Pharm and wish to pursue postgraduation after pharmacy may pursue PharmD (post baccalaureate)
The government/s or leaders who wish to establish a new pharmacy institute may be encouraged to have PharmD as the only pharmacy study program to offer
Intake capacity for PharmD may be increased
Students who have completed M. Pharm in non clinical subjects but are interested to become CPs may be encouraged to purse PharmD (PB).
Less Number of People in PharmD as Compared to Other Pharmacy Courses
At present, numbers of PharmD students are very less as compared to B. Pharm or D. Pharm in India. This comparative less number of PharmD students is surely not enough to provide CPS to the whole country.
Possible solution
We further strongly recommend the same-PharmD’fication of the country. Making PharmD as the basic educational requirement for pharmacists will automatically increase the number of PharmD qualified pharmacists in the country which in turn can come up with CPS for more and more people.
Limitations associated with M. Pharm (Pharmacy Practice/Clinical Pharmacy)
Previously clinical pharmacy education was given under the study course of M. Pharm (Pharmacy Practice/Clinical Pharmacy) but when we compare it with PharmD or PharmD (PB), PharmD has got following advantages:
PharmD has got better learning and practicing opportunities than the M. Pharm for clinical subjects
PharmD has got more hospital exposure as mentioned in the syllabus than the M. Pharm
After PharmD one can prefix “Dr.” in his name, where the M. Pharm cannot
PharmD has got one year internship while the M. Pharm hasn’t
PharmD has got better professional competence
PharmD has got uniform syllabus over the country but for the M. Pharm it is not so.
Therefore, if PharmD has got more advantages as compared to M. Pharm (Pharmacy Practice/Clinical Pharmacy), the question arises, why keep 2 study programs with similar subjects and different competence?
Possible solutions
As we know, PharmD’fication of the country is essential, PharmD (PB) may be preferred and promoted over M. Pharm (Pharmacy Practice/Clinical Pharmacy) and PharmD (PB) should be offered as the only option for the students who wish to pursue M. Pharm (Pharmacy Practice/Clinical Pharmacy). Also, it is recommended that the present M. Pharm (Pharmacy Practice/Clinical Pharmacy) passed out students who are practicing in the hospitals or working as a faculty in the institutes, may be converted to PharmD with optimum training and internship.
Benefits because of the solution
This will allow:
Help M. Pharm people to improve professional competence
Privilege to prefix “Dr.”
It will help to increase the number of PharmD's and pharmacy practitioners in the nation
They will have equal opportunities as that of PharmD people
They will not be underestimated by the recruiters.
Poor awareness about clinical pharmacy services
There is no or very poor awareness for CPS and PharmD in the country.[1,48] Presently, the common man of India does not know anything about the CPS or role of the pharmacist in the hospitals.
Possible solution
Huge awareness needs to be made about CPS in the nation by pharmacy colleges, regulatory authorities and government bodies. Present CPs need to prove the importance of CPS by practice.
No recognition by government regulatory bodies/recruiters in pharmaceutical companies
Until now, the central and several state governments have not considered them to work in hospitals as CPs.[48] The clinical pharmacy profession is restricted only to hospitals linked to pharmacy practice and PharmD schools.[50] The regulatory framework has not recognized the need of CPs at national level and there are almost no opportunities for CPs in hospital settings in India.[50] The recruiters in private pharmaceutical companies are not completely aware of the role of CPs.
Possible solution
Central and all state governments should recognize the importance of CPS and make the strategies accordingly. All the state pharmacy councils and related regulatory authorities are advised to convince the importance of CPS to the governments. At institute/university level, the information leaflets containing the role of CPs in (respective) companies can be made and circulated among pharmaceutical companies.
Lack of government/government aided institutes for PharmD
Currently, almost all institutes providing PharmD degree belong to private set-up. The common man of India takes treatment in government hospitals, but government institutes running PharmD courses attached to government hospitals are very rare in the country.
Possible solution
The number of government institutes offering PharmD should be tremendously increased. The governments need to take initiative for the same. This will lead more middle-class students to take PharmD education.
Poor quantity of quality research publications
The world share of output and citation impact of India in different related fields is as shown in Table 4.[51]
Table 4.
World share of output and citation impact of India in related fields[51]
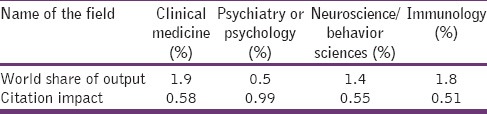
The research numbers as shown in Table 4 are definitely poor as far as population and numbers of educational institutes in India are considered. In the clinical pharmacy field, the basic problem we feel is “no publication of the research work”. Already the research conducted in the clinical pharmacy is poor in both quality and quantity in India. CPs are doing research work but, unfortunately, those research works are not equal to number of publications.
For this, all thesis works (in PharmD/M. Pharm/PhD) should be made of publishable quality and all thesis works should be encouraged to publish. The students need to be properly trained about the ways of publishing research works and the related ethical issues. A topic may be added in the syllabi on research ethics and ways of publishing the research. Salary increments for faculties and PhDs being awarded must be strictly based upon number of quality publications. E.g. a rule may be framed as 1 PhD = 5 or 3 PubMed indexed research publications.
Publishing the research work has following advantages:
It gives new ideas to other researchers
It avoids repetition and decreases the efforts and time of other researchers in the same field
It gives royalty to the researchers regarding their research work
It causes development of a particular research field
It further improves the quality of the research conducted
It provides a reference material to other researchers
Publication of the work gives a quick access to other researchers about a particular research
Publication may also give access to other similar works previously conducted in the same area
Publications help in decision making for other researches that is, to select a particular area for further research or not?
Research publications indirectly contribute to the development of the country
It improves the curriculum vitae and career of the researcher.
Poor research quality
The research conducted in clinical and/or community pharmacy in India is very poor in overall quality as well as quantity because clinical pharmacy is a newer concept in the country and international quality publications are found rarely in the literature by Indian researchers (in clinical pharmacy).
Possible solution
To solve this problem:
Providing proper research guidance to students
Only quality journals should be persuaded for publication of the research. There are several factors to select and evaluate a particular journal for publication but roughly and in short, the journals indexed with PubMed are considered to be good
CPs need to develop better skills for research
The regulatory network needs to make useful strategies regarding this problem
Research-related topics may be added in the syllabi of CPs. E.g. importance of research in clinical pharmacy
Motivation of students for research
The clinical pharmacy related journals from India must be upgraded to international standards.
No competitive stipend as compared to other doctoral programs
Speaking academically, in general, interns in various other healthcare professions in India such as MBBS, MD, BAMS (Bachelor of Ayurveda Medicine and Surgery), and veterinary sciences students receive stipend during their internship. But PharmDs are receiving noncompetent or no stipend during internship at present.
Possible solution
Strong and effective policies should be framed by concerned regulatory authorities to meet the optimum requirements of the stipend.
No stipend for Graduate Aptitude Test in Engineering/Graduate Pharmacy Aptitude Test qualified PharmD (postbaccalaureate) students
Graduate Pharmacy Aptitude Test (GPAT) or Graduate Aptitude Test in Engineering (GATE) are the two exams for pharmacy students to pursue post graduate courses in pharmacy like M. Pharm. If a student cracks GPAT/GATE, he gets stipend for 2 years that is, up to completion of his M. Pharm degree. Ironically, there is no provision for a GATE/GPAT qualified PharmD (PB) student to get stipend, in fact, both M. Pharm and PharmD (PB) are postgraduate study programs after completion of B. Pharm and both are pharmacists by profession.
Possible solution
According to us, GATE/GPAT qualified PharmD (PB) students also deserve the stipend. There is pressing need to make regulation for such students to receive the stipend.
Faculty related issues
Scarcity of patient focused work by faculties: This affects the motivation of students to work in wards. But at the same time, faculties of medicine, surgery and nursing are patient focused.
Scarcity of faculties: The current number of faculties in pharmacy practice departments are definitely not enough to cover whole hospital.
Lack of skilled staff: As pharmacy practice is not a well established field in India, the faculties are not of international standards.
Payment issues: After completion of PharmD/M. Pharm (Pharmacy Practice), quality students mostly prefer industrial jobs because of higher payments and increments which causes entry of poorer students in academics.
Possible solutions
Faculties need to do patient focused work. They need to work efficiently in the wards. As PharmD curriculum has the highest hospital exposure in its program, so, according to us, as an initiative there “must” be at least one PharmD qualified staff in every PharmD institute with descent salary. Practically efficient quality improvement programs for the staffs may be organized for training of the staffs.
International skilled faculties may be invited for better training of faculties.
Paying more fees than other pharmacy courses
Though worried about future and having less hospital-based jobs at present, PharmD students are paying more fees than other pharmacy courses such as B. Pharm, M. Pharm and D. Pharm in the country.[48] PharmD and PharmD (PB) are paying higher fees than B. Pharm and M. Pharm respectively (The exact fee structures may be obtained from the respective colleges or their websites).
Possible solution
Since there are several benefits, PharmD’fication is essential and must be promoted. Therefore, we strongly recommend that, the fees paid by “B. Pharm and PharmD” and “M. Pharm and PharmD (PB)” should be the same in the respective institutes/universities/colleges. The concerned authorities are encouraged to frame the policies.
Improper strategies of the government toward pharmacists
Recently, Indian cabinet has approved Bachelor of Science course in community health for the betterment of rural healthcare infrastructure.[52] However, instead of that, knowledge and skills of pharmacists may be used.[53]
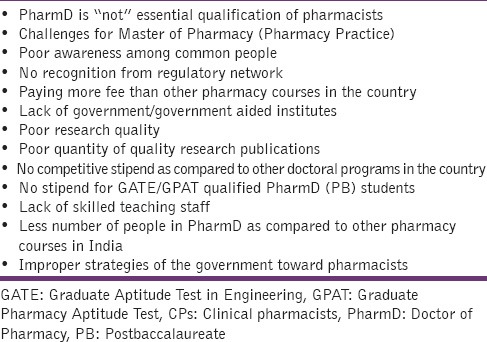
Overall, challenges to CPs in the country are as shown in Table 5.
Table 5.
Challenges to CPs in India
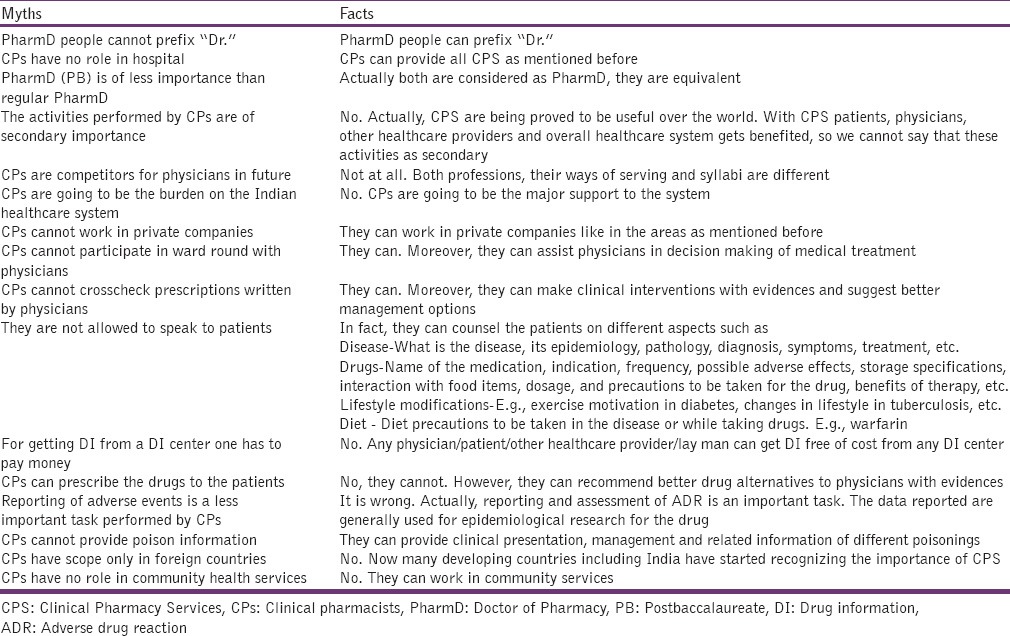
Myths and facts about clinical pharmacists
As the clinical pharmacy profession is new in India, there are many misunderstandings about it. Here, we have tried to cover the myths and the facts about the profession [Table 6].
Table 6.
Myths and facts about clinical pharmacists
Conclusion
Clinical pharmacists are definitely going to be the major support to the Indian healthcare system. Patients, physicians, other healthcare providers, hospitals and different industries will to get a lot of benefits out of CPS [Figure 3]. But at the same time, there is strong requirement to consider various unresolved issues. According to us, the time has come for India, to implement maximum CPS for the welfare of maximum people and also to make PharmD as the basic educational requirement for pharmacists in the country.
Figure 3.
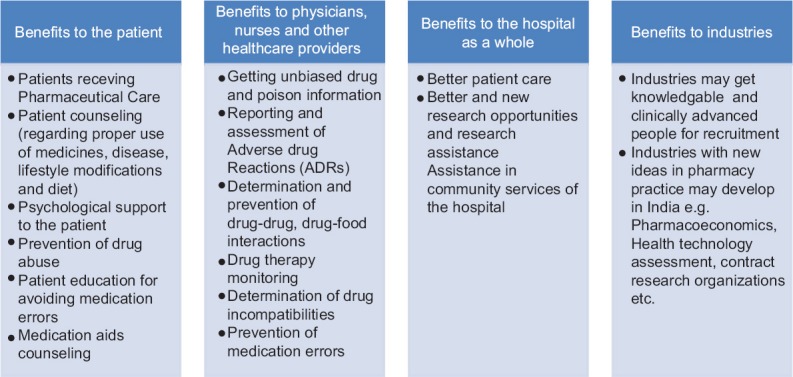
Benefits of clinical pharmacists
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Deshpande PR, Farooq KK, John DM, Rao EJ. PharmD: A new concept in India. J Pharm Bioallied Sci. 2012;4:84–6. doi: 10.4103/0975-7406.92746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dooley M, Bogovic A, Carroll A, Cuell S, Galbraith K, Matthews H. SHPA standards of practice for clinical pharmacy. [Last cited on 2011 Jul 20];J Pharm Pract Res. 2005 35:122–46. Available on: http://www.shpa.org.au/lib/pdf/practice_standards/clinical_pharm_ro.pdf . [Google Scholar]
- 3.Dooley M, Lyall H, Galbriath K, et al. SHPA (The Society of Hospital Pharmacists of Australia) standards of practice for clinical pharmacy. SHPA Practice Standards and Definitions. 1996:2–11. [Google Scholar]
- 4.Pharmacovigilance Program of India (PvPI) [Last accessed on 2013 Oct 14]. Available from: http://www.cdsco.nic.in/pharmacovigilance_intro.htm .
- 5.Geneva (Switzerland): Office of Publications; 2002. World Health Organization. The Importance on Pharmacovigilance. Safety Monitoring on Medicinal Products. [Google Scholar]
- 6.Dikshit RK. Challenges in pharmacovigilance. Indian J Pharmacol. 2010;42:333. doi: 10.4103/0253-7613.71882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chopra D, Wardhan N, Rehan HS. Knowledge, attitude and practices associated with adverse drug reaction reporting amongst doctors in a teaching hospital. Int J Risk Saf Med. 2011;23:227–32. doi: 10.3233/JRS-2011-0543. [DOI] [PubMed] [Google Scholar]
- 8.Pharm D. New Delhi; 10th May: Ministry of Health and Family Welfare (Pharmacy Council of India); 2008. [Last cited on 2013 May 27]. Regulations 2008. The Gazette of India, No. 19, Part III, Sec. 4; pp. 1–97. Available from: http://www.pci.nic.in/PDF-Files/PharmD-Revised-A.pdf . [Google Scholar]
- 9.Arulmani R, Rajendran SD, Suresh B. Adverse drug reaction monitoring in a secondary care hospital in South India. Br J Clin Pharmacol. 2008;65:210–6. doi: 10.1111/j.1365-2125.2007.02993.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Harugeri A, Parthasarathi G, Ramesh M, Guido S, Basavanagowdappa H. Frequency and nature of adverse drug reactions in elderly in-patients of two Indian medical college hospitals. J Postgrad Med. 2011;57:189–95. doi: 10.4103/0022-3859.85201. [DOI] [PubMed] [Google Scholar]
- 11.Ahmad A, Patel I, Balkrishnan R, Mohanta GP, Manna PK. An evaluation of knowledge, attitude and practice of Indian pharmacists towards adverse drug reaction reporting: A pilot study. Perspect Clin Res. 2013;4:204–10. doi: 10.4103/2229-3485.120168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chauhan N, Moin S, Pandey A, Mittal A, Bajaj U. Indian aspects of drug information resources and impact of drug information centre on community. J Adv Pharm Technol Res. 2013;4:84–93. doi: 10.4103/2231-4040.111524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Parthasarathi G, Ramesh M, Nyfort-Hansen K, Nagavi BG. Clinical pharmacy in a South Indian teaching hospital. Ann Pharmacother. 2002;36:927–32. doi: 10.1345/aph.1A223. [DOI] [PubMed] [Google Scholar]
- 14.George B, Rao PG. Assessment and evaluation of drug information services provided in a South Indian teaching hospital. Indian J Pharmacol. 2005;37:315–9. [Google Scholar]
- 15.Prasanna RD, Ahsan FK, Sudeepthi BL, Kazim S, Sonal SM, Manohar B, et al. Assessment of medicine information provided on demand by clinical pharmacists in nephrology wards in a tertiary care hospital. Indian J Pharm Pract. 2013;6:25–9. [Google Scholar]
- 16.Rama M, Viswanathan G, Acharya LD, Attur RP, Reddy PN, Raghavan SV. Assessment of drug-drug interactions among renal failure patients of nephrology ward in a South Indian Tertiary Care Hospital. Indian J Pharm Sci. 2012;74:63–8. doi: 10.4103/0250-474X.102545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kannan G, Anitha R, Rani VN, Thennarasu P, Alosh J, Vasantha J, et al. A study of drug-drug interactions in cancer patients of a south Indian tertiary care teaching hospital. J Postgrad Med. 2011;57:206–10. doi: 10.4103/0022-3859.85207. [DOI] [PubMed] [Google Scholar]
- 18.Patel VK, Acharya LD, Rajakannan T, Surulivelrajan M, Guddattu V, Padmakumar R. Potential drug interactions in patients admitted to cardiology wards of a south Indian teaching hospital. Australas Med J. 2011;4:9–14. doi: 10.4066/AMJ.2011.450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lucca JM, Ramesh M, Narahari GM, Minaz N. Impact of clinical pharmacist interventions on the cost of drug therapy in intensive care units of a tertiary care teaching hospital. J Pharmacol Pharmacother. 2012;3:242–7. doi: 10.4103/0976-500X.99422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pichala PT, Kumar BM, Zachariah S, Thomas D, Saunchez L, Gerardo AU. An interventional study on intensive care unit drug therapy assessment in a rural district hospital in India. J Basic Clin Pharm. 2013;4:64–7. doi: 10.4103/0976-0105.118801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lakshmi R, James E, Kirthivasan R. Study on impact of clinical pharmacist's interventions in the optimal use of oral anticoagulants in stroke patients. Indian J Pharm Sci. 2013;75:53–9. doi: 10.4103/0250-474X.113550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Adepu R, Rasheed A, Nagavi BG. Effect of patient counseling on quality of life in type-2 diabetes mellitus patients in two selected South Indian community pharmacies: A study. Indian J Pharm Sci. 2007;69:519–24. [Google Scholar]
- 23.Venkatesan R, Devi AS, Parasuraman S, Sriram S. Role of community pharmacists in improving knowledge and glycemic control of type 2 diabetes. Perspect Clin Res. 2012;3:26–31. doi: 10.4103/2229-3485.92304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Malathy R, Narmadha M, Ramesh S, Alvin JM, Dinesh BN. Effect of a diabetes counseling programme on knowledge, attitude and practice among diabetic patients in Erode district of South India. J Young Pharm. 2011;3:65–72. doi: 10.4103/0975-1483.76422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Viswanad V, Prabhakar V. The Emergence of the Clinical Pharmacist and the Indian Scenario. Inventi Impact: Pharmacy Practice. 2011;1:4–7. [Google Scholar]
- 26.Medscape Mobile. [Last accessed on 2011 Nov 20]. Available from: http://www.medscape.com/public/mobileapp .
- 27.Thomson Reuters, Healthcare App Shelf. [Last accessed on 2011 Nov 20]. Available from“ http://www.healthcare.thomsonreuters.com/micromedexMobile .
- 28.Jain S, Basu S, Parmar VR. Medication errors in neonates admitted in intensive care unit and emergency department. Indian J Med Sci. 2009;63:145–51. [PubMed] [Google Scholar]
- 29.Guidelines on Counselling. November, Appendix A. 2005. [Last accessed on 2011 Nov 20]. Available from: http://www.napra.org/Content_Files/Files/PEI/StandardsGuidelines/Guidelines-on-Counseling.pdf .
- 30.Palaian S, Prabhu M, Shankar PR. Patient counseling by pharmacist – A focus on chronic illness. Pak J Pharm Sci. 2006;19:65–72. [PubMed] [Google Scholar]
- 31.Joyce AW, Sunderland VB, Burrows S, McManus A, Howat P, Maycock B. Community pharmacy's role in promoting healthy behaviours. [Last accessed on 2011 Jul 15];J Pharm Pract Res. 2007 37:42–4. Available from: http://www.cbrcc.curtin.edu.au/reports_journal_articles/jppr%2037%2042-44.pdf . [Google Scholar]
- 32.Basak SC, Sathyanarayana D. Community pharmacy based research activity in India: A bibliometric study of the past ten years. South Med Rev. 2010;3:7–10. [PMC free article] [PubMed] [Google Scholar]
- 33.Association of Community Pharmacists of India. [Last accessed on 2014 Apr 26]. Available from: http://www.acpi.in/index.htm .
- 34.Frequently Asked Questions About Pharm D. [Last cited on 2013 Mar 13]. Available from: http://www.pci.nic.in/PDF-Files/question.PDF .
- 35.Gazette Notification on “Minimum Qualification for Teachers in Pharmacy Institutions Regulation. Pharmacy Council of India. 2014. [Last accessed on 2015 Feb 18]. Available from: http://www.pci.nic.in/Circulars/Teachers%20Education%20Regulation.pdf .
- 36.Sharma S. How to become a competent medical writer? Perspect Clin Res. 2010;1:33–7. [PMC free article] [PubMed] [Google Scholar]
- 37.What is Medical Coding? AAPC (American Academy of Professional Coders) [Last accessed on 2015 Feb 18]. Available from: https://www.aapc.com/medical-coding/medical-coding.aspx .
- 38.What is Medical Billing? (American Academy of Professional Coders) [Last accessed on 2015 Feb 18]. Available from: https://www.aapc.com/medical-billing/medical-billing.aspx .
- 39.AHDI Answers Frequently Asked Questions About Medical Transcription. AHDI (Association of Healthcare Documentation Integrity) [Last accessed on 2015 Feb 18]. Available from: http://www.ahdionline.org/VisitorCenter/MTsPartnersInMedicalCommunication/AHDIAnswersFAQsAboutMedicalTranscription/tabid/243/Default.aspx .
- 40.World Health Organization; [Last accessed on 2015 Feb 18]. Pharmacovigilance. Essential Medicines and Health Products. Available from: http://www.who.int/medicines/areas/quality_safety/safety_efficacy/pharmvigi/en . [Google Scholar]
- 41.Burton ME, Munger MA, Bednarczyk EM, Davis LE, Davis GA, Elliot ME, et al. Update: The clinical pharmacist as principal investigator. [Last accessed on 2015 Jan 26];Pharmacotherapy. 2010 30:485e–9. Available from: https://www.accp.com/docs/positions/whitePapers/Pharm3012_ACCP-Burton-PharmD-PI.pdf . [Google Scholar]
- 42.Durrant KL. Florida: University of Florida College of Pharmacy/WPPD Gainesville; 2006. [Last accessed on 2015 Feb 18]. Pharmacist's Role in Enhancing Patient Participation in Clinical Trial Research. Available from: http://www.pharmacy.ufl.edu/files/2013/01/Pharmacist-Role-in-Clinical-Trial-Research.pdf . [Google Scholar]
- 43.Anderson PD. The broad field of forensic pharmacy. J Pharm Pract. 2012;25:7–12. doi: 10.1177/0897190011431144. [DOI] [PubMed] [Google Scholar]
- 44.What is a Medical Science Liaison? MSLS (Medical Science Liaison Society) [Last accessed on 2015 Feb 18]. Available from: http://www.themsls.org/what-is-an-msl .
- 45.Bhambri R, Khan R, Lam A, Abdulsattar Y, Schnell A. Working Outside the Dispensing Box: The Roles of the Medical Information Specialist and Medical Science Liaison. [Last accessed on 2015 Feb 18]. p. 2. Available from: http://www.pharmacytimes.com/publications/career/2014/pharmacycareers_fall2014/working-outside–the-dispensing-box-the-roles-of-themedical-information-specialist-and-medical-science-liaison/P-2 .
- 46.Gupta SK, Nayak RP. An insight into the emerging role of regional medical advisor in the pharmaceutical industry. Perspect Clin Res. 2013;4:186–90. doi: 10.4103/2229-3485.115386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Stergachis A, Lander R, Webb L. Promoting the pharmacist's role in public health. J Am Pharm Assoc (2003) 2006;46:311–2. doi: 10.1331/154434506777069444. 314-6, 318. [DOI] [PubMed] [Google Scholar]
- 48.Deshpande PR. Should the PharmD degree be the basic educational requirement in India for pharmacists? Am J Pharm Educ. 2013;77:132. doi: 10.5688/ajpe776132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Jishnu V, Gilhotra R, Mishra D. Pharmacy education in India: Strategies for a better future. J Young Pharm. 2011;3:334–42. doi: 10.4103/0975-1483.90248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Mangasuli S, Rajan S, Khan SA. A decade of pharmacy practice education in India. Am J Pharm Educ. 2008;72:16. [PMC free article] [PubMed] [Google Scholar]
- 51.Bibliometric Study of India's Scientific Publication Outputs During 2001-10; Department of Science and Technology, Government of India; July. 2012. [Last accessed on 2014 Apr 26]. Available from: http://www.dst.gov.in/whats_new/whats_new12/report.pdf .
- 52.The Hindu; [Last accessed on 2014 Mar 05]. Cabinet Approves B.Sc. Community Health course in State Universities, News on 14 Nov 2013. Available from: http://www.thehindu.com/news/national/cabinet-approves-bsccommunity-health-course-in-state-universities/article5348436.ece . [Google Scholar]
- 53.Bhatt PA. Being a clinical pharmacist: Expectations and outcomes. Indian J Pharmacol. 2014;46:1–2. doi: 10.4103/0253-7613.124882. [DOI] [PMC free article] [PubMed] [Google Scholar]


