Abstract
Distress tolerance is defined behaviorally as the ability to maintain goal directed behavior while experiencing physical or psychological distress. Distress tolerance is closely related to emotion regulation, and is a clinically relevant construct contributing to psychopathology across adults and adolescents, yet limited research has examined the development of this construct. A number of studies suggest the importance of parenting in the emergence of emotion regulation capacities in childhood and adolescence. In the current study, we utilize a behavioral measure of distress tolerance to examine whether maternal distress tolerance is related to adolescent distress tolerance, and if this association differs as a function of gender. We also examine the influence of family emotional climate, namely maternal response to adolescent distress and adolescent attachment. Results indicate a significant maternal distress tolerance by adolescent gender interaction, such that maternal distress tolerance predicts adolescent distress tolerance in daughters, but not sons. The family emotional climate variables were unrelated to maternal or adolescent distress tolerance. Taken together, data indicate that maternal distress tolerance is significantly related to the distress tolerance of adolescent daughters, and indicates the potential utility of addressing maternal distress tolerance in clinical work with adolescents.
Keywords: distress tolerance, adolescence, parent, gender
Introduction
Distress tolerance is defined behaviorally as the ability to maintain goal directed behavior while experiencing physical or psychological distress. Low distress tolerance appears central to the emergence and maintenance of a number of clinical disorders (Leyro, Zvolensky, & Bernstein, 2010). However, there is a paucity of empirical research examining the development of distress tolerance (Zvolensky, Vujanovic, Bernstein, & Leyro, 2010), which is surprising given the value of identifying the mechanisms underlying distress tolerance to intervention and treatment efforts. This research is especially critical during middle adolescence, an important maturational period where internalizing and externalizing symptoms may begin to emerge, impairing current adolescent functioning and increasing the likelihood of future psychopathology in adulthood (Colman, Wadsworth, Croudace, & Jones, 2007; McGue & Iacono, 2005).
Distress tolerance is a construct that is closely related emotion regulation (Linehan, 1993; Zvolensky et al., 2010). Converging studies suggest that the socialization of emotion and emotion regulation is influenced by family context (Bridges, Denham, & Ganiban, 2004; Kopp, 1989; Morris, Silk, Steinberg, Myers, & Robinson, 2007; Thompson, 1994; Zeman, Cassano, Perry-Parrish, & Stegall, 2006), identifying the need to consider the contribution of parents to the developing mechanisms that underscore distress tolerance in adolescence. Concurrently, there is an emerging literature reporting the impact of gender on how adolescents regulate and respond to distress (Daughters et al., 2009; Neumann, van Lier, Gratz, & Koot, 2010), identifying gender as an important variable to consider. Therefore the purpose of the current study was to investigate the relationship between maternal and adolescent distress tolerance and the role of adolescent gender as a moderating factor.
Distress Tolerance and Emerging Psychopathology
Distress tolerance is widely accepted to be a clinically relevant capacity to both internalizing and externalizing symptoms (Leyro et al., 2010). Consequently, a negative reinforcement approach has been adopted to understand the commonality of distress tolerance to this broader scope of psychopathology (Baker, Piper, McCarthy, Majeskie, & Fiore, 2004). Negative reinforcement refers to the motivation to avoid or escape negative affective states, and has typically been applied within an addiction framework, wherein repeated substance use alleviates distress associated with withdrawal (Baker et al., 2004). In studies of adults, substance-dependent individuals are reported to have lower tolerance of distress (Quinn, Brandon, & Copeland, 1996), and distress tolerance is related to recent abstinence duration and treatment retention among residential treatment-seeking substance abusers (Daughters, Lejuez, Bornovalova, et al., 2005; Daughters, Lejuez, Kahler, Strong, & Brown, 2005). Outside of an addiction setting, distress tolerance has been found to be associated with antisocial (Daughters, Sargeant, Bornovalova, Gratz, & Lejuez, 2008) and borderline (Bornovalova et al., 2008) personality disorders, depression (Buckner, Keough, & Schmidt, 2007), anxiety disorder symptoms (Danielson et al., 2010; Keough et al., 2010), and eating disorders (Anestis, Selby, Fink, & Joiner, 2007).
Although self-report measures to assess distress tolerance exist, a number of computer-based paradigms have been developed to capture the negative reinforcement element of distress tolerance (Lejuez, Daughters, Danielson, & Ruggiero, 2006; Lejuez, Kahler, & Brown, 2003). These paradigms typically engage participants in a task that requires persistence and becomes increasingly difficult and thus, increasingly distressing. These tasks offer rewards for continued persistence but critically include a termination option that affords the participant the opportunity to escape the source of distress. Thus these tasks may be highly sensitive in their measurement of distress tolerance, embodying the measurement of negative reinforcement mechanisms in a manner that is more ecologically valid than self-report measures alone.
There is an emerging literature examining the relation between adolescent distress tolerance and internalizing and externalizing symptoms. In an early adolescent sample, low distress tolerance is associated with increased internalizing symptoms in female adolescents, increased past year alcohol use in Caucasian adolescents, and increased past year delinquent behaviors in African American adolescents (Daughters et al., 2009). In middle to older adolescents, a moderating effect of gender is also observed, such that females with low DT, but not males, display significantly greater affective problems (Daughters et al., in press). Finally, a 4-year longitudinal study reports that distress tolerance is relatively stable from childhood to adolescence, with no significant mean-level or individual-level change (Cummings et al., 2013). In addition to these studies, distress tolerance is associated with adolescent self-injury (Nock & Mendes, 2008), and moderates the relationship between adolescent risk taking propensity and risk taking behavior (MacPherson et al., 2010). Taken together, distress tolerance appears to be clinically relevant across adults and adolescents, highlighting the importance of examining the etiology of this core construct.
Parental Influences on the Development of Emotion Regulation
Despite its clinical relevance, little is known regarding the developmental trajectory of distress tolerance. Given the close relationship between distress tolerance and emotion regulation (Zvolensky et al., 2010), this literature may provide valuable insight into the evolution of this critical capacity. Morris and colleagues (2007) have proposed a tripartite model of how parent and family context may contribute to the emergence of child and adolescent emotion regulation. First, children learn how to regulate emotions through observation of parents and other family members. This may include learning through modeling reactivity and responding to emotional events they have observed, social referencing and emotional contagion. Second, emotion-relevant parenting practices may impact emotion regulation development in children and adolescents. Indeed, there is some evidence to suggest that parental beliefs related to their own and their child’s emotions predict self-reported and physiological markers of regulatory capacity in children (Gottman, Katz, & Hooven, 1996). Third, the emotional climate of the family is also believed important in contributing to the development of emotion regulation. For instance, the early attachment relationship between parent and child has been shown to be a significant predictor of the child’s emotion regulation functioning (Gilliom, Shaw, Beck, Schonberg, & Lukon, 2002) as well as sensitivity to the perception and recognition of emotion more generally (Fonagy, Gergely, Jurist, & Target, 2006).
Notably, a number of gender differences have emerged in studies examining parental influence on child and adolescent emotion regulation. In regard to the gender of the parent, data indicate that mothers may play more of a role in the development of their offspring’s emotion regulation capabilities (Fivush, Brotman, Buckner, & Goodman,2000; McDowell, Kim, O’neil, & Parke, 2002), especially in adolescence (Lamb, 2004; Pleck, 1997). For instance, maternal expressive suppression predicts adolescent expressive suppression, while there is no relationship between paternal and adolescent emotion regulation strategies (Bariola, Hughes, & Gullone, 2012). One potential process that may contribute to this relationship is that mothers often spend more time with their offspring than fathers during early childhood throughout adolescence (Craig, 2006).
Closely related to this literature, recent data suggest that maternal distress tolerance may significantly impact mothers’ parenting behaviors. Using a behavioral task designed to assess distress tolerance in response to an inconsolable infant, findings indicate that low maternal distress tolerance is related to lower interest and curiosity in their infant’s mental well-being (Rutherford, Goldberg, Luyten, Bridgett, & Mayes, in press). Therefore, similar to individual differences in emotion regulation, maternal distress tolerance may be an important capacity that influences the way mothers interact and respond to their child, which consequently influences individual differences in child emotional development.
Evidence also indicates the existence of gender specific socialization of emotion regulation, such as greater relationship-oriented strategies for girls and more active and instrumental strategies for boys (Eisenberg et al., 1998; Hops, 1995; Nolen-Hoeksema & Girgus, 1995; Sheeber, Davis, & Hops, 2002). Parents preferentially reinforce the display of sadness in girls and anger in boys (Block, 1983; Eisenberg et al., 1998; Fuchs & Thelen, 1988), and encourage distraction and problem-solving strategies more for boys than for girls (Eisenberg et al., 1998). A few studies have examined how parental emotion regulation influences adolescent emotion regulation as a function of adolescent gender. For instance, offspring of depressed mothers, especially daughters, show early impairments in cognitive and behavioral domains of emotion regulation, including more passive and less active strategies for regulation relative to daughters of non-depressed mothers (Silk, Shaw, Skuban, Oland, & Kovacs, 2006). Notably, in one study, compared to adolescent males, adolescent females reported less access to emotion regulation strategies, lower emotional clarity and more difficulty in completing goal-directed behaviors when under distress (Neumann et al., 2010). This latter gender difference finding is of interest to the present study, as their self-report assessment of goal completion under distress mirrors the definition of behavioral assessments of distress tolerance. Taken together, findings suggest that it is important to take in to consideration gender differences when examining parental influence on adolescent distress tolerance.
Current Study
In reviewing the present literature, little is known regarding the developmental trajectory of distress tolerance. However, a number of studies suggest the importance of mothers in the emergence of emotion regulation capacity in childhood and adolescence. In this study, mother-adolescent dyads completed a computer-based behavioral distress tolerance task. We incorporated three family emotional climate variables as potential mediators in our analysis. Given theory indicating the importance of modeling, social referencing and emotional contagion to the emergence of emotion regulation in development (Morris et al., 2007), we examined maternal internalizing symptoms, maternal responses to adolescent distress and adolescent-maternal attachment as mechanisms underlying the relation between maternal and adolescent distress tolerance. We hypothesized that maternal distress tolerance would be associated with adolescent distress tolerance, and these family emotional climate variables would account for this relationship. Noting the aforementioned gender differences emerging in the parent and adolescent emotion regulation and distress tolerance literature, we included adolescent self-identified gender as a moderator in this investigation. Specifically, we hypothesized that maternal distress tolerance would be more likely to predict distress tolerance in adolescent daughters compared to their adolescent sons.
Method
Participants
A total of 161 adolescents and their primary caregiver were recruited via newspaper advertisements and letters sent to guardians of all high school students in the local community. Given the study aims and the relatively small sample size of adolescent-father (n = 14) and adolescent-legal guardian dyads (n = 2), only adolescent-biological mother dyads were included in the present study. An additional six dyads were excluded due to missing self-report data. Therefore, the final sample included 139 adolescents (46.8% female, n = 65) and their biological mothers. There were no siblings included in the final sample. Adolescents and mothers ranged in age from 14 to 18 years (M = 16.1, SD = 0.9) and 32 to 58 years (M = 45.8, SD = 5.9), respectively. The racial/ethnic background of families were in line with the US Census Bureau in the surrounding county (U.S. Bureau of the Census, 2010), and included 62.6% (n = 87) African American, 29.5% (n = 41) White, 5.0% (n = 7) Hispanic/Latino, 2.9% (n = 4) Native American, 5.8% (n = 8) Asian, and 6.5% (n = 9) ‘Other’. Percentages total over 100% because participants had the option of selecting more than one ethnic category. Approximately half (53.2%, n = 74) of the adolescents lived in a home with both biological parents, with a mean annual household income of $86,500 (SD = 48,200) a year. Of the mothers, 95.7% (n = 133) reported graduating high school and 38.8% (n = 54) received a college degree (i.e., BA or BS) or higher.
Procedure
Adolescents and mothers provided written informed assent and consent, respectively. All aspects of the study and the consent form were approved by the University Institutional Review Board. Following informed consent, participants completed a battery of self-report measures and a computerized behavioral distress tolerance (DT) task. Mothers were provided cash and adolescents were given gift cards as payment for participation.
Measures
Potential covariates
In addition to demographic variables, adolescent internalizing symptoms were examined as potential covariates given their relationship to distress tolerance (Daughters et al., 2009; Leyro et al., 2010). Specifically, adolescent internalizing symptoms were assessed using the Youth Self-Report (YSR; Achenbach & Rescorla, 2001). The YSR is a 118-item checklist of behavioral and emotional problems that adolescents rate as either (0) ‘not true’, (1) ‘somewhat or sometimes true’, or (2) ‘often true’. For the current study, the normalized T-score was calculated for the broadband Internalizing Scale, which is comprised of three Problem Scales (Withdrawn/Depressed, Anxious/Depressed, and Somatic Complaints). Cronbach’s alpha for the Internalizing Scale was α = .77.
Family emotional climate
Family emotional climate variables included maternal internalizing symptoms, adolescent maternal attachment, and maternal response to adolescent distress.
Maternal internalizing symptoms
Maternal internalizing symptoms were assessed using the Center for Epidemiologic Studies Depression Scale (CES-D; Radloff, 1977) and the State-Trait Anxiety Inventory (STAI; Spielberger, 1983). The CES-D is a 20-item self-report measure of current depressive symptoms. Participants are asked to respond to each item using a 4-point Likert scale, with total scores ranging from 0 to 60. A cutoff point of 16 or above is frequently used to index current depression (Weissman, Sholomskas, Pottenger, Prusoff, & Locke, 1977; Radloff, 1977). Mothers also completed the STAI, which is a validated self-report measure used to assess “state” (i.e., transitory) and “trait” (i.e., stable) levels of anxiety. Participants respond to each item using a 4-point Likert scale and total scores for each scale range from 20 to 80, with higher scores indicating increased levels of anxiety. Internal reliability for the CES-D, STAI-Trait, STAI-State were α = .80, α = .91, and α = .87, respectively.
Adolescent-maternal attachment
The Parent as a Secure Base-Revised (PSB; Cassidy & Woodhouse, 2003) was completed by adolescents to assess the degree to which they consider their biological mother a ‘secure base’ or a person that provides physical and emotional support. The self-report scale includes 13-items and responses are made using a 5-point Likert scale. Importantly, the PSB has been shown to be associated with other measures of parental attachment and perceptions of parental warmth (Cassidy, Ziv, Rodenberg, & Woodhouse, 2003; Woodhouse et al., 2010). Cronbach’s alpha for the PSB for adolescents in the current sample was α = .87.
Maternal responses to adolescent distress
Mothers completed the Coping with Children’s Negative Emotions Scale-Adolescent Version (CCNES-AP; Fabes & Eisenberg, 1998), which is a self-report questionnaire that instructs parents to report their likelihood of responding in different ways to nine hypothetical situations in which their adolescent may experience distress (e.g., adolescent becomes angry at a friend). Parents rate the likelihood of their responses using a 7-point Likert scale, ranging from 1(very unlikely) to 7 (very likely). A total of six response types are assessed, which were grouped into ‘Supportive’ and ‘Unsupportive’ subscales (e.g., Perry, Calkins, Nelson, Leerkes, & Marcovitch, 2012). The Supportive subscale was calculated by summing the scores on emotion focused, problem-focused, and expressive encouragement responses, and the Unsupportive subscale was calculated by summing the scores on minimization, punitive, and distress responses. Internal reliability for the subscales were α = .87 (Supportive) and α = .73 (Unsupportive).
Distress tolerance
The Computerized Paced Auditory Serial Addition Task (PASAT-C) was used to assess distress tolerance. The PASAT-C has been shown to reliably increase affective distress and has repeatedly been used as a behavioral measure of distress tolerance (Daughters et al., 2005; Daughters et al., 2009; Lejuez, Kahler, & Brown, 2003). For this task, numbers are displayed sequentially on a computer screen along with a keyboard of numbers. Participants are instructed to add the current number on the screen to the previously presented number, and use the computer’s mouse to click on the correct response before the subsequent number appears. If participants answer correctly, they hear a pleasant bell sound and a point is added to their score. If they answer incorrectly or do not make a response before the subsequent number appears, no point is added and they hear an aversive explosion sound. The task consists of three levels which increase in difficulty. The latency between number presentations is titrated to the participant’s ability level to control for the effects of skill on the task. Level 1 is the titration phase (5 min) and level 2 is the stress phase (5 min). Following a brief resting period, level 3 is the distress tolerance (DT) phase and lasts up to 7 minutes, with the option to terminate exposure to the task. During the stress phase and the DT phase, the latency between number presentations exceeds the participant’s skill level, thereby forcing task failure and inducing distress. Participants are given the option to terminate the DT phase (final level) at any time by clicking on a “Quit” button in the upper left hand corner of the screen. However, participants are told that their performance on the task determines the magnitude of their payment at the end of the session.
Prior to level 1 and after level 2, participants rate their level of anxiety, frustration, difficulty concentrating, physical discomfort, and irritability on a scale from 1 indicating “none” to 100 indicating “extreme.” Ratings are made after level 2 instead of after termination of the task to prevent any confounds associated with termination latency. Pre-task and post-level 2 ratings are respectively averaged to create broad indices of subjective distress.
Using this task, DT can be conceptualized as either a continuous (i.e., latency to task termination) or dichotomous (i.e., quit the task vs. did not quit the task) variable. However, according to the Shapiro-Wilk test (Shaprio & Wilk, 1965), latency to task termination was not normally distributed in either adolescents (zskew = −1.11, zkurtosis = −0.47, p < .01) or mothers (zskew = −2.15, zkurtosis = 3.08, p < .01). Thus, in the current study, DT was represented as a dichotomous variable, such that individuals who persisted until the end of the task were categorized as “high DT” and those who quit the task were categorized as “low DT.” Notably, numerous prior investigations have dichotomized DT by quit status (Anestis, Gratz, Bagge, & Tull, 2012; Daughters et al., 2009; Gorka, Ali, & Daughters, 2012; Schloss & Haaga, 2011; Tull, Gratz, Coffey, Weiss, & McDermott, 2012).
Data Analysis Plan
Analyses were conducted with adolescent distress tolerance (DT) as the dependent variable. As was previously discussed, DT was dummy coded as “high DT (0)” or “low DT (1)” for both mothers and adolescents. Potential covariates were determined by examining demographic variables and adolescent internalizing symptoms for associations with the dependent variable (adolescent DT) and proposed mediators (maternal internalizing symptoms, adolescent-maternal attachment and maternal response to adolescent distress), using bivariate correlations and independent sample t-tests. The identification of mediators and the unique and interactive effects of maternal DT and gender on adolescent DT were examined using PROCESS – an SPSS macro for path-analysis based modeling (Hayes, 2013). Relevant to the current study, for dichotomous outcome variables PROCESS employs logistic regression to estimate conditional indirect effects using standard ‘simple slopes’ methods for moderated mediation and two-way interactions in moderation models (Hayes, 2013; Aiken & West, 1991).
Results
Distress Tolerance
Adolescents persisted on the PASAT-C for an average of 317.0 (SD = 156.1) seconds and 37.4% (n = 52) quit the task (i.e., low DT). Paired t-tests indicated a significant increase in self-reported distress during the task [t(1, 138) = −6.9, p < .001, d = 0.50], with no relationship between adolescent DT and self-reported changes in distress (p > .05). Mothers persisted on the PASAT-C for an average of 367.6 (SD = 120.4) seconds and 20.9% (n = 29) quit the task. As expected, results indicated a significant increase in self-reported distress during the task [t(1, 138) = −9.2, p < .001, d = 0.79], with no relationship between maternal DT and self-reported change in distress (p > .05).
Identification of Covariates
Preliminary analyses were conducted to explore the impact of demographic factors (age, ethnic/racial background, gender, and family income), measures of internalizing psychopathology (composite measure of adolescent internalizing symptoms), and family context (maternal internalizing symptoms, adolescent-maternal attachment and maternal response to adolescent distress) on the dependent variable (adolescent distress tolerance) and independent variables/moderators (gender, maternal distress tolerance) to identify potential covariates and mediators for later analyses (see Tabachnick & Fidell, 1996). The interrelationships and descriptive data for continuous variables are presented in Table 1, and the relationship between study variables with gender and maternal and adolescent distress tolerance are presented in Table 2.The only data not presented in the tables is the insignificant chi square analyses examining the relationship of ethnicity with gender, maternal DT, and adolescent DT (all p’s > .05).
Table 1.
Bivariate correlations among study variables.
| Mean | SD | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Adolescent Age | 16.06 | 0.98 | --- | |||||||||
| 2. Maternal Age | 45.80 | 5.92 | 0.04 | --- | ||||||||
| 3. Annual Family Income | 86.45 | 48.19 | −0.09 | 0.29** | --- | |||||||
| 4. Mother CES-D | 5.22 | 4.38 | 0.05 | −0.13 | −0.27 | --- | ||||||
| 5. Mother STAI-State | 44.85 | 4.38 | 0.14 | −0.08 | −0.09 | 0.54** | --- | |||||
| 6. Mother STAI-Trait | 30.02 | 8.33 | −0.07 | 0.02 | −0.07 | 0.00 | −0.29** | --- | ||||
| 7. CCNES Supportive | 16.82 | 2.36 | −0.10 | −0.08 | 0.27** | −0.16 | −0.25** | 0.16 | --- | |||
| 8. CCNES Unsupportive | 7.41 | 2.38 | 0.02 | −0.11 | −0.29** | 0.36** | 0.31** | 0.15 | −0.07 | --- | ||
| 9. Adolescent PSB | 55.79 | 8.11 | 0.17* | −0.10 | 0.11 | −0.11 | 0.01 | 0.11 | 0.09 | −0.06 | --- | |
| 10. YSR Internalizing Scale | 51.96 | 9.34 | 0.01 | −0.05 | −0.03 | 0.12 | 0.20* | −0.06 | −0.06 | 0.07 | −0.34** | --- |
Note
p < .05
p < .01
SD = standard deviation; YSR = Youth Self-Report; CES-D = Center for Epidemiologic Studies Depression Scale; STAI = State-Trait Anxiety Inventory; PSB = Parent as a Secure Base; CCNES = Coping with Children’s Negative Emotions Scale
Table 2.
Relation of study variables to adolescent gender and maternal and adolescent distress tolerance.
| Adolescent Gender | Maternal DT | Adolescent DT | |||||||
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| Variable | t | p | d | t | p | d | t | p | d |
| Demographic Variables | |||||||||
| Adolescent Age | 0.27 | 0.79 | 0.05 | −0.07 | 0.94 | 0.02 | 1.25 | 0.21 | 0.23 |
| Maternal Age* | −0.71 | 0.48 | 0.13 | 2.18 | 0.03* | 0.47 | 0.72 | 0.47 | 0.13 |
| Annual Family Income | 0.53 | 0.60 | 0.11 | 1.66 | 0.10 | 0.44 | 0.30 | 0.77 | 0.06 |
| Mother Self-Report Measures | |||||||||
| CES-D* | 0.28 | 0.78 | 0.05 | −2.41 | 0.02* | 0.51 | −1.13 | 0.26 | 0.20 |
| STAI-State | 0.09 | 0.93 | 0.02 | −1.27 | 0.21 | 0.27 | 0.03 | 0.56 | 0.10 |
| STAI-Trait | 0.54 | 0.59 | 0.09 | −0.40 | 0.69 | 0.08 | −0.43 | 0.67 | 0.08 |
| CCNES Supportive Reactions | 0.39 | 0.69 | 0.07 | 1.46 | 0.15 | 0.32 | −1.73 | 0.09 | 0.31 |
| CCNES Unsupportive Reactions | 0.67 | 0.50 | 0.12 | −0.55 | 0.58 | 0.12 | −0.63 | 0.53 | 0.11 |
| Adolescent Self-Report Measures | |||||||||
| YSR Internalizing Scale | 0.09 | 0.93 | 0.02 | 0.43 | 0.67 | 0.10 | −0.97 | 0.34 | 0.18 |
| PSB | 0.57 | 0.57 | 0.10 | −.386 | 0.70 | 0.08 | −0.32 | 0.75 | 0.06 |
Note
p < .05
DT = distress tolerance; YSR = Youth Self-Report; CES-D = Center for Epidemiologic Studies Depression Scale; STAI = State-Trait Anxiety Inventory; PSB = Parent as a Secure Base; CCNES = Coping with Children’s Negative Emotions Scale; Independent sample t-tests were conducted with gender (female = 0, male = 1) and distress tolerance (high = 0, low = 1) as the dependent variables.
In order to meet criteria for moderated mediation, there must first be evidence of the moderation (adolescent gender) of the effect of the independent variable (maternal DT) on the mediator (maternal internalizing symptoms, adolescent attachment, maternal response to distress), and an effect of the mediator on the dependent variable (adolescent DT) (Hayes, 2013). Since there was no evidence of a relationship between the proposed mediators and the dependent variable, subsequent analyses did not examine moderated mediation. Variables significantly associated with gender, maternal DT, or adolescent DT were included as covariates. Specifically, mothers with low distress tolerance were significantly younger and reported higher levels of depressive symptoms.
Logistic Regression Moderation Analysis
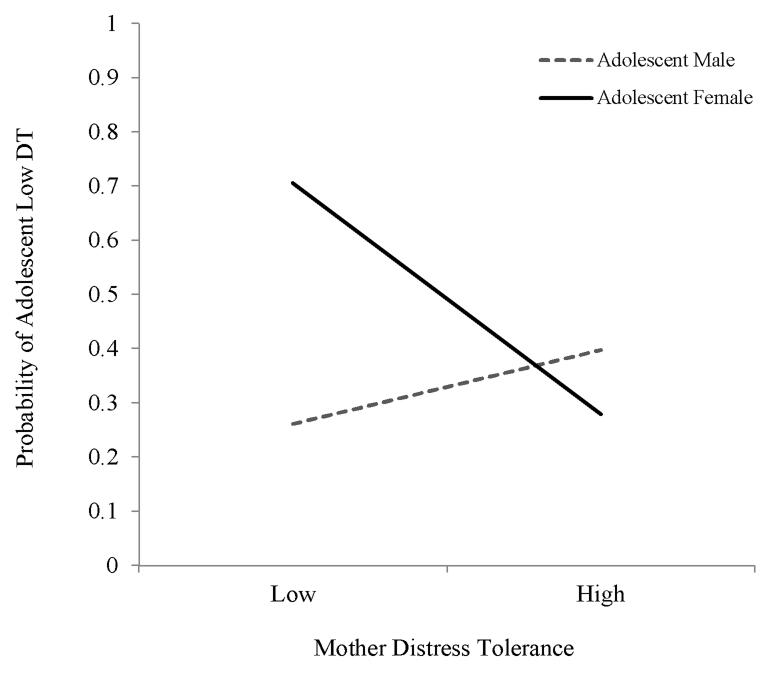
Results from the PROCESS (Hayes, 2013) moderation analyses are displayed in Table 3. The primary focus in the PROCESS moderation model is the coefficient for the product of the independent variable (i.e., maternal DT) and the moderator (i.e., adolescent gender), while accounting for the identified covariates (i.e., maternal age, maternal depressive symptoms). Results of the final model (Nagelkerke R2 = 0.16) indicate a significant main effect for maternal DT (B = 4.15, p < .01), such that low maternal DT was associated with low adolescent DT. However, these effects were qualified by a significant maternal DT by gender interaction (B = − 2.38, p < .05). For a significant interaction, PROCESS then provides the conditional effects of the independent variable at each value of the moderator (i.e., “simple slopes”). As displayed in Table 3 and Figure 1, these conditional effects indicated that mothers with low DT evidenced a higher probability of having a female adolescent with low DT (B = 1.77, p < .05). Maternal DT was not related to the DT of their male adolescent (B = −0.60, p > .05).
Table 3.
Regression and follow-up analyses predicting adolescent distress tolerance.
| Coefficient | SE | Z | p | |
|---|---|---|---|---|
| Regression Model | ||||
| Constant | −6.47 | 2.62 | −2.47 | 0.02 |
| Maternal Age | 0.02 | 0.04 | 0.62 | 0.54 |
| Maternal CES-D | 0.06 | 0.04 | 1.26 | 0.21 |
| Adolescent Gender | 0.57 | 0.44 | 1.29 | 0.20 |
| Maternal DT** | 4.15 | 1.60 | 2.59 | 0.00 |
| Maternal DT × Adol Gender* | −2.38 | 0.98 | −2.42 | 0.02 |
| Follow-up Analyses | ||||
| Adolescent Females* | 1.77 | 0.74 | 2.41 | 0.02 |
| Adolescent Males | −0.60 | 0.68 | −0.89 | 0.37 |
Note
p < .01
p < .05
CI = Confidence Intervals; CES-D = Center for Epidemiologic Studies Depression Scale; DT = distress tolerance; Maternal DT was dummy coded as either high DT (0; did not quit the task) or low DT (1; did quit the task).
Figure 1.
Probability of adolescent low distress tolerance as a function of maternal distress tolerance and gender.
Discussion
Distress tolerance, or the ability to persist in goal directed activity when experiencing physical or psychological distress, is a well-established correlate of maladaptive behavior and psychopathology among both adults and adolescents. Yet, despite theory and research linking emotion regulation in adolescence to maternal individual differences, no studies to date have examined this relation. We aimed to close this gap in the current study by examining whether maternal distress tolerance predicts adolescent distress tolerance, and if adolescent gender moderates this relation. Indeed, findings indicate that maternal distress tolerance is a significant predictor of adolescent distress tolerance in daughters, but not sons.
This finding is the first to provide empirical support for an association between maternal and adolescent distress tolerance, and is in line with work suggesting a genetic component to distress tolerance (Amstadter et al., 2012), as well as theory and research indicating the importance of family context in the development of emotion regulation skills (e.g., Morris et al., 2007). Moreover, this finding extends the family based models that parents impact emotion regulation by finding effects in adolescence. Previous work has focused primarily on the influence of parental emotion regulation on infancy and early childhood (e.g., Eisenberg et al., 1998), and the current findings suggest that these relationships extend to older adolescence, in particular between mothers and adolescent daughters. Importantly, distress tolerance was assessed with a laboratory-based behavioral task, thereby eliminating many of the limitations associated with self-report (e.g., difficulty recalling the circumstances under which a behavior occurred; inaccurate reporting).
The finding that the maternal-adolescent distress tolerance relation is specific to daughters is in line with our hypotheses. However, the current study did not provide data as to the underlying processes by which maternal distress tolerance impacts the distress tolerance of daughters, but not sons. One explanation is that the role of modeling is facilitated by gender identification, as postulated in social learning theory (Bandura, 1977). Alternatively, it is possible that mothers socialize the regulation of emotions differently between daughters and sons. Although recent literature suggests that mothers socialize emotions similarly in adolescent daughters and sons (Brand & Klimes-Dougan, 2010), research indicates gender difference in emotion socialization in younger children (Adams et al., 1995). For example, parents encourage boys’ anger and discourage/punish girls’ anger (Chaplin, Casey, Sinha, & Mayes, 2010). Although in need of empirical investigation, it is plausible that a lack of acceptance of negative emotions among girls at an early age may lead to an inability to regulate negative emotions in adolescence, in particular among adolescents whose mothers display low distress tolerance.
Research supporting the tripartite model indicates that children and adolescents learn how to regulate emotions via modeling, observing emotion-relevant parenting practices, and/or the emotional climate of the family. The current study partially assessed for these potential factors, namely maternal internalizing symptoms, adolescent attachment and maternal responses to adolescent distress. Contrary to expectation, there was no evidence of a relationship among these factors with maternal or adolescent distress tolerance. Although theory suggests that negative parental responses to children’s emotional displays serve to heighten children’s emotional arousal and teach avoidance rather than appropriate expression of negative emotions (Eisenberg et al., 1998), the majority of work in this area has been conducted with pre-school and school aged children, with limited data on the effect of parental response to adolescent distress on adolescent emotion regulation. Given the increased influence of peers and the external environment, it is possible that family emotional climate is not as predictive of emotion regulation, and in particular distress tolerance, in adolescents as they are in childhood. Notably, we did not assess all aspects of the family emotional climate, such as maternal modeling. It is possible that maternal modeling of response to their own distress in the presence of their adolescent exerts greater influence than maternal response to adolescent distress (e.g., Saarni, 1999).
Prior to drawing the conclusion that these variables are not as relevant to adolescence, it is important to consider the possibility that the null findings are partially attributable to our methodological approach, such that distress tolerance was assessed behaviorally whereas family emotional climate variables were self-report. Previous work examining family emotional climate and emotion regulation has utilized self-report measures of emotion regulation (e.g., Gresham & Gullone, 2012), and evidence suggests a discrepancy between self-report and behavioral assessments broadly (Mauss & Robinson, 2009), and specifically in the assessment of distress tolerance (e.g., McHugh et al., 2010). It is possible that behavioral and self-report measures are not capturing the same construct, and/or individuals are not accurate reporters of their behavior. It will therefore be important for future studies to include a comprehensive battery of both self-report and behavioral measures of distress tolerance and family emotional climate to disentangle the influence of each construct. For instance, examining the relationship between distress tolerance and maternal response to adolescent distress via observation of a real-time parent-adolescent interaction. Similarly, evidence indicates that genetic (e.g., Amstadter et al., 2012), physiological (e.g., Perry et al., 2012) and neurological (e.g., Ochsner et al., 2004) indices underlie distress tolerance and/or emotion regulation, yet it is unclear if these indices account for the maternal-adolescent distress tolerance relationship. An important next step is a multi-method approach to understanding the biobehavioral and neurological pathogenesis of the maternal-adolescent female distress tolerance relationship. Finally, these findings highlight the potential benefit of future studies examining maternal distress tolerance in the context of treatments aimed at addressing affect regulation in adolescence. Dialectical behavior therapy (DBT; Linehan, 1993) targets difficulties with emotion regulation and includes a specific module aimed at improving distress tolerance, and has been adapted for adolescents presenting a range of psychopathology and problem behavior (e.g., DBT-A; Miller et al., 2007). Furthermore, given evidence that poor child and adolescent outcomes is consistently associated with parental psychopathology and parental affect regulation (Southam-Gerow, Kendall, & Weersing, 2001;Werba et al., 2002), the incorporation of DBT, and more specifically distress tolerance skills, for parents is an important avenue for future research (e.g., Ben-Porath, 2010).
A number of limitations are of note. First, the current study did not include an assessment of paternal distress tolerance. Future work examining the contribution of both maternal and paternal distress tolerance to adolescent distress tolerance in males and females is an important next step, in particular given evidence that generally the socialization of emotion in adolescents appears comparable by mothers and fathers (Klimes-Dougan et al., 2007). Second, the cross-section design limits causal interpretation. Future longitudinal work is needed to examine the contribution of parental distress tolerance over time. Third, other forms of psychopathology among mothers and adolescents were not assessed; therefore it is unclear whether psychiatric diagnoses may have impacted the findings. Despite these limitations, the current study provides initial evidence for the impact of maternal distress tolerance on adolescent female distress tolerance, highlighting the need for future research to continue to examine the pathogenesis of this clinically relevant construct.
Acknowledgments
This work was supported by National Institute of Drug Abuse Grant R21DA022741 (PI: Daughters).
References
- Achenbach TM, Rescorla LA. Manual for the ASEBA School-Age Forms & Profiles. University of Vermont, Research Center for Children, Youth, & Families; Burlington, VT: 2001. [Google Scholar]
- Adams S, Kuebli J, Boyle PA, Fivush R. Gender differences in parent child conversations about past emotions: A longitudinal investigation. Sex Roles. 1995;33:309–323. [Google Scholar]
- Aiken LS, West SG. Multiple regression: Testing and interpreting interactions. Sage; Newbury Park, CA: 1991. [Google Scholar]
- Amstadter AB, Daughters SB, MacPherson L, Reynolds EK, Danielson CK, Wang F, Potenza M, Gelertner J, Lejuez CW. Genetic associations with performance on a behavioral measure of distress intolerance. Journal of Psychiatric Research. 2012;46:87–94. doi: 10.1016/j.jpsychires.2011.09.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anestis MD, Selby EA, Fink EL, Joiner TE. The multifaceted role of distress tolerance in dysregulated eating behaviors. International Journal of Eating Disorders. 2007;40:718–726. doi: 10.1002/eat.20471. [DOI] [PubMed] [Google Scholar]
- Baker TB, Piper ME, McCarthy DE, Majeskie MR, Fiore MC. Addiction motivation reformulated: An affective processing model of negative reinforcement. Psychological Review. 2004;111:33–51. doi: 10.1037/0033-295X.111.1.33. [DOI] [PubMed] [Google Scholar]
- Bandura A. Social Learning Theory. Prentice-Hall; Englewood Cliffs, NJ: 1977. [Google Scholar]
- Bariola E, Hughes EK, Gullone E. Relationships between parent and child emotion regulation strategy use: A brief report. Journal of Child and Family Studies. 2012;21:1–6. [Google Scholar]
- Ben-Porath DD. Dialectical behavior therapy applied to parent skills training: Adjunctive treatment for parents with difficulties in affect regulation. Cognitive and Behavioral Practice. 2010;17:458–465. doi:10.1016/j.cbpra.2009.07.005. [Google Scholar]
- Block JH. Differential premises arising from differential socialization of the sexes: Some conjectures. Child development. 1983;54:1335–1354. [PubMed] [Google Scholar]
- Bornovalova MA, Gratz KL, Daughters SB, Nick B, Delany-Brumsey A, Lynch TR, Lejuez CW. A multimodal assessment of the relationship between emotion dysregulation and borderline personality disorder among inner-city substance users in residential treatment. Journal of Psychiatric Research. 2008;42:717–726. doi: 10.1016/j.jpsychires.2007.07.014. [DOI] [PubMed] [Google Scholar]
- Brand A,E, Klimes-Dougan B. Emotion socialization in adolescence: The roles of mothers and fathers. New Directions for Child and Adolescent Development. 2010;128:85–100. doi: 10.1002/cd.270. doi:10.1002/cd.270. [DOI] [PubMed] [Google Scholar]
- Bridges LJ, Denham SA, Ganiban JM. Definitional issues in emotion regulation research. Child Development. 2004;75:340–345. doi: 10.1111/j.1467-8624.2004.00675.x. doi:10.1111/j.1467-8624.2004.00675.x. [DOI] [PubMed] [Google Scholar]
- Buckner JD, Keough ME, Schmidt NB. Problematic alcohol and cannabis use among young adults: The roles of depression and discomfort and distress tolerance. Addictive Behaviors. 2007;32:1957–63. doi: 10.1016/j.addbeh.2006.12.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casey BJ, Getz S, Galvan A. The adolescent brain. Developmental Review. 2008;28(1):62–77. doi: 10.1016/j.dr.2007.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cassidy J, Woodhouse S. The Secure Base Scale–Revised. 2003. Unpublished manuscript. [Google Scholar]
- Cassidy J, Ziv Y, Rodenberg M, Woodhouse SS, Kobak R. Adolescent perceptions of parents: Associations with adolescent attachment (AAI) and interactions with parents. Assessing attachment in middle childhood and adolescence: Toward a multi-method approach; Symposium conducted at the biennial meeting of the Society for Research in Child Development; Tampa, FL. 2003, April; (Chair) [Google Scholar]
- Chaplin TM, Casey J, Sinha R, Mayes LC. Gender differences in caregiver emotion socialization of low-income toddlers. New Directions for Child and Adolescent Development. 2010;128:11–27. doi: 10.1002/cd.266. DOI:10.1002/cd.266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colman I, Wadsworth M, Croudace T, Jones P. Forty-year psychiatric outcomes following assessment for internalizing disorder in adolescence. American Journal of Psychiatry. 2007;164(1):126–133. doi: 10.1176/ajp.2007.164.1.126. [DOI] [PubMed] [Google Scholar]
- Craig L. Does father care mean fathers share?: A comparison of how mothers and fathers in intact families spend time with children. Gender & Society. 2006;20:259–281. [Google Scholar]
- Cummings JR, Bornovalova MA, Ojanen T, Hunt E, MacPherson L, Lejuez CW. Time doesn’t change everything: The longitudinal course of distress tolerance and its relationship with externalizing and internalizing symptoms during early adolescence. Journal of Abnormal Child Psychology. 2013;1:1–14. doi: 10.1007/s10802-012-9704-x. doi:0.1007/s10802-012-9704-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Danielson C, Ruggiero KJ, Daughters SB, Lejuez CW. Distress tolerance, risk-taking propensity, and PTSD symptoms in trauma-exposed youth: Pilot study. The Behavior Therapist. 2010;33:28–34. [Google Scholar]
- Daughters SB, Lejuez C, Kahler CW, Strong DR, Brown RA. Psychological distress tolerance and duration of most recent abstinence attempt among residential treatment-seeking substance abusers. Psychology of Addictive Behaviors. 2005;19:208. doi: 10.1037/0893-164X.19.2.208. [DOI] [PubMed] [Google Scholar]
- Daughters SB, Lejuez CW, Bornovalova MA, Kahler CW, Strong DR, Brown RA. Distress tolerance as a predictor of early treatment dropout in a residential substance abuse treatment facility. Journal of Abnormal Psychology. 2005;114:729–734. doi: 10.1037/0021-843X.114.4.729. [DOI] [PubMed] [Google Scholar]
- Daughters SB, Reynolds EK, MacPherson L, Kahler CW, Danielson CK, Zvolensky M, Lejuez C. Distress tolerance and early adolescent externalizing and internalizing symptoms: The moderating role of gender and ethnicity. Behaviour Research and Therapy. 2009;47:198–205. doi: 10.1016/j.brat.2008.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daughters SB, Sargeant MN, Bornovalova MA, Gratz KL, Lejuez C. The relationship between distress tolerance and antisocial personality disorder among male inner-city treatment seeking substance users. Journal of Personality Disorders. 2008;22:509–524. doi: 10.1521/pedi.2008.22.5.509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eisenberg N, Cumberland A, Spinrad TL. Parental socialization of emotion. Psychological inquiry. 1998;9(4):241–273. doi: 10.1207/s15327965pli0904_1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eisenberg N, Morris AS. Children’s emotion-related regulation. In: Kail R, editor. Advances in Child Development and Behavior. Vol. 30. Academic Press; Amstersdam: 2002. pp. 190–229. [PubMed] [Google Scholar]
- Fabes RA, Eisenberg N. The Coping with Children’s Negative Emotions Scale - Adolescent Perception Version: Procedures and scoring. Arizona State University; Tempe, AZ: 1998. [Google Scholar]
- Fivush R, Brotman MA, Buckner JP, Goodman SH. Gender differences in parent–child emotion narratives. Sex Roles. 2000;42:233–253. [Google Scholar]
- Fonagy P, Gergely G, Jurist EL, Target M. Affect regulation, mentalization, and the development of the self. H. Karnac (Books) Ltd.; London: 2006. [Google Scholar]
- Fuchs D, Thelen MH. Children’s expected interpersonal consequences of communicating their affective state and reported likelihood of expression. Child Development. 1988;59:1314–1322. doi: 10.1111/j.1467-8624.1988.tb01500.x. [DOI] [PubMed] [Google Scholar]
- Galvan A, Hare T, Voss H, Glover G, Casey BJ. Risk-taking and the adolescent brain: who is at risk? Developmental Science. 2007;10(2):F8–F14. doi: 10.1111/j.1467-7687.2006.00579.x. [DOI] [PubMed] [Google Scholar]
- Galvan A, Hare TA, Parra CE, Penn J, Voss H, Glover G, Casey BJ. Earlier development of the accumbens relative to orbitofrontal cortex might underlie risk-taking behavior in adolescents. Journal of Neuroscience. 2006;26:6885–6892. doi: 10.1523/JNEUROSCI.1062-06.2006. doi:10.1523/jneurosci.1062-06.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garber J, Braafladt N, Zeman J. The regulation of sad affect: An information-processing perspective. In: Dodge KA, editor. The development of emotion regulation and dysregulation. Cambridge studies in social and emotional development. Cambridge University Press; New York: 1991. pp. 208–240. [Google Scholar]
- Garnefski N, Kraaij V, van Etten M. Specificity of relations between adolescents’ cognitive emotion regulation strategies and internalizing and externalizing psychopathology. Journal of adolescence (London, England) 2005;28:619–631. doi: 10.1016/j.adolescence.2004.12.009. [DOI] [PubMed] [Google Scholar]
- Gilliom M, Shaw DS, Beck JE, Schonberg MA, Lukon JEL. Anger regulation in disadvantaged preschool boys: strategies, antecedents, and the development of self-control. Developmental Psychology. 2002;38:222. doi: 10.1037//0012-1649.38.2.222. [DOI] [PubMed] [Google Scholar]
- Gorka SM, Ali B, Daughters SB. The role of distress tolerance in the relationship between depressive symptoms and problematic alcohol use. Psychology of Addictive Behaviors. 2012;26:621–626. doi: 10.1037/a0026386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gottman JM, Katz LF, Hooven C. Parental meta-emotion philosophy and the emotional life of families: Theoretical models and preliminary data. Journal of Family Psychology. 1996;10:243–268. [Google Scholar]
- Gratz KL, Roemer L. Multidimensional assessment of emotion regulation and dysregulation: Development, factor structure, and initial validation of the difficulties in emotion regulation scale. Journal of Psychopathology and Behavioral Assessment. 2004;26:41–54. [Google Scholar]
- Gresham D, Gullone E. Emotion regulation strategy use in children and adolescents: The explanatory roles of personality and attachment. Personality and Individual Differences. 2012;52:616–621. [Google Scholar]
- Gross JJ, John OP. Individual differences in two emotion regulation processes: implications for affect, relationships, and well-being. Journal of Personality and Social Psychology. 2003;85:348–362. doi: 10.1037/0022-3514.85.2.348. [DOI] [PubMed] [Google Scholar]
- Hayes AF. An introduction to mediation, moderation, and conditional process analysis: A regression-based approach. Guilford Press; New York: 2013. [Google Scholar]
- Hops H. Age-and gender-specific effects of parental depression: A commentary. Developmental Psychology. 1995;31(3):428. [Google Scholar]
- Keough ME, Riccardi CJ, Timpano KR, Mitchell MA, Schmidt NB. Anxiety symptomatology: The association with distress tolerance and anxiety sensitivity. Behavior Therapy. 2010;41(4):567–574. doi: 10.1016/j.beth.2010.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klimes-Dougan B, Brand AE, Zahn Waxler C, Usher B, Hastings PD, Kendziora K, Garside RB. Parental emotion socialization in adolescence: Differences in sex, age and problem status. Social Development. 2007;16:326–342. [Google Scholar]
- Kopp CB. Regulation of distress and negative emotions: A developmental view. Developmental Psychology. 1989;25(3):343–354. [Google Scholar]
- Lamb ME, editor. The role of the father in child development. Wiley; 2004. [Google Scholar]
- Larson RW, Richards MH, Moneta G, Holmbeck G, Duckett E. Changes in adolescents’ daily interactions with their families from ages 10 to 18: Disengagement and transformation. Developmental Psychology. 1996;32:744–754. [Google Scholar]
- Lejuez CW, Daughters SB, Danielson CK, Ruggiero K. The Behavioral Indicator of Resiliency to Distress (BIRD) 2006. Unpublished manual. [Google Scholar]
- Lejuez CW, Kahler CW, Brown RA. A modified computer version of the Paced Auditory Serial Addition Task (PASAT) as a laboratory-based stressor. the Behavior Therapist. 2003;26:290–293. [Google Scholar]
- Leyro TM, Zvolensky MJ, Bernstein A. Distress tolerance and psychopathological symptoms and disorders: A review of the empirical literature among adults. Psychological Bulletin. 2010;136:576–600. doi: 10.1037/a0019712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacPherson L, Reynolds EK, Daughters SB, Wang F, Cassidy J, Mayes LC, Lejuez C. Positive and negative reinforcement underlying risk behavior in early adolescents. Prevention Science. 2010;11:331–342. doi: 10.1007/s11121-010-0172-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mauss IB, Robinson MD. Measures of emotion: A review. Cognition and Emotion. 2009;23:209–237. doi: 10.1080/02699930802204677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDowell DJ, Kim M, O’neil R, Parke RD. Children’s emotional regulation and social competence in middle childhood: The role of maternal and paternal interactive style. Marriage & Family Review. 2002;34:345–364. [Google Scholar]
- McGue M, Iacono WG. The association of early adolescent problem behavior with adult psychopathology. American Journal of Psychiatry. 2005;162:1118–1124. doi: 10.1176/appi.ajp.162.6.1118. [DOI] [PubMed] [Google Scholar]
- Miller AL, Rathus JH, Dubose AP, Dexter-Mazza ET, Goldklang AR. Dialectical Behavior Therapy for Adolescents. In: Dimeff L, Koerner K, editors. Dialectical Behavior Therapy in Clinical Practice: Applications Across Disorders and Settings. Guilford; New York: 2007. pp. 245–263. [Google Scholar]
- Miller AL, Wyman SE, Huppert JD, Glassman SL, Rathus JH. Analysis of behavioral skills utilized by suicidal adolescents receiving dialectical behavior therapy. Cognitive and Behavioral Practice. 2000;7:183–187. [Google Scholar]
- Monk CS, McClure EB, Nelson EE, Zarahn E, Bilder RM, Leibenluft E, Pine DS. Adolescent immaturity in attention-related brain engagement to emotional facial expressions. Neuroimage. 2003;20:420–428. doi: 10.1016/s1053-8119(03)00355-0. [DOI] [PubMed] [Google Scholar]
- Morris AS, Silk JS, Steinberg L, Myers SS, Robinson LR. The role of the family context in the development of emotion regulation. Social Development. 2007;16:361–388. doi: 10.1111/j.1467-9507.2007.00389.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neumann A, van Lier PAC, Gratz KL, Koot HM. Multidimensional assessment of emotion regulation difficulties in adolescents using the Difficulties in Emotion Regulation Scale. Assessment. 2010;17:138–149. doi: 10.1177/1073191109349579. [DOI] [PubMed] [Google Scholar]
- Nock MK, Mendes WB. Physiological arousal, distress tolerance, and social problem-solving deficits among adolescent self-injurers. Journal of Consulting and Clinical Psychology. 2008;76:28. doi: 10.1037/0022-006X.76.1.28. [DOI] [PubMed] [Google Scholar]
- Nolen-Hoeksema S, Girgus JS. Explanatory style and achievement, depression, and gender differences in childhood and early adolescence. In: Buchanan G, Seligman MP, editors. Explanatory style. Lawrence Erlbaum Associates, Inc.; Hillsdale, NJ England: 1995. pp. 57–70. [Google Scholar]
- Patterson GR. The early development of coercive family process. In: Reid JB, Patterson GR, Snyder J, editors. Antisocial behavior in children and adolescents: A developmental analysis and model for intervention. American Psychological Association; Washington, DC: 2002. pp. 25–44. [Google Scholar]
- Perry NB, Calkins SD, Nelson JA, Leerkes EM, Marcovitch S. Mothers’responses to children’s negative emotions and child emotion regulation: The moderating role of vagal suppression. Developmental Psychobiology. 2012;54:503–513. doi: 10.1002/dev.20608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pleck J. Paternal involvement: Levels, sources and consequences. In: Lamb ME, editor. The role of the father in child development. Vol. 1997. Wiley; New York: pp. 66–103. [Google Scholar]
- Quinn EP, Brandon TH, Copeland AL. Is task persistence related to smoking and substance abuse? The application of learned industriousness theory to addictive behaviors. Experimental and Clinical Psychopharmacology. 1996;4:186–190. [Google Scholar]
- Radloff LS. The CES-D scale A self-report depression scale for research in the general population. Applied psychological measurement. 1977;1:385–401. [Google Scholar]
- Romeo RD, McEwen BS. Stress and the adolescent brain. Annals of the New York Academy of Sciences. 2007;1094:202–214. doi: 10.1196/annals.1376.022. [DOI] [PubMed] [Google Scholar]
- Rutherford HJV, Goldberg B, Luyten P, Bridgett DJ, Mayes LC. Parental reflective functioning is associated with tolerance of infant distress but not general distress: Evidence for a specific relationship using a simulated baby paradigm. Infant Behavior and Development. doi: 10.1016/j.infbeh.2013.06.008. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saarni C. The Development of Emotional Competence. Guilford Press; New York: 1999. [Google Scholar]
- Schloss HM, Haaga DA. Interrelating behavioral measures of distress tolerance with self-reported experiential avoidance. Journal of Rational-Emotive & Cognitive-Behavior Therapy. 2011;29:53–63. doi: 10.1007/s10942-011-0127-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shapiro SS, Wilk MB. An analysis of variance test for normality (Complete Samples) Biometrika. 1965;52:591–611. [Google Scholar]
- Sheeber L, Davis B, Hops H. Gender-specific vulnerability to depression in children of depressed mothers. Children of depressed parents: Mechanisms of risk and implications for treatment. In: Goodman SH, Gotlib IH, editors. American Psychological Association; Washington, DC US: 2002. pp. 253–274. [Google Scholar]
- Silk JS, Shaw DS, Skuban EM, Oland AA, Kovacs M. Emotion regulation strategies in offspring of childhood-onset depressed mothers. Journal of Child Psychology and Psychiatry. 2006;47(1):69–78. doi: 10.1111/j.1469-7610.2005.01440.x. doi:10.1111/j.1469-7610.2005.01440.x. [DOI] [PubMed] [Google Scholar]
- Southam-Gerow MA, Kendall PC, Weersing VR. Examining outcome variability: Correlates of treatment response in a child and adolescent anxiety clinic. Journal of Clinical Child Psychology. 2001;30:422–436. doi: 10.1207/S15374424JCCP3003_13. [DOI] [PubMed] [Google Scholar]
- Spear LP. The adolescent brain and age-related behavioral manifestations. Neuroscience & Biobehavioral Reviews. 2000;24:417–463. doi: 10.1016/s0149-7634(00)00014-2. [DOI] [PubMed] [Google Scholar]
- Spielberger CD. Manual for the State-Trait Anxiety Inventory. Consulting Psychologists Press; Palo Alto, CA: 1983. [Google Scholar]
- Tabachnick BG, Fidell LS. Using multivariate statistics. 3rd ed. Harper Collins; New York: 1996. [Google Scholar]
- Thompson RA. Emotion regulation: A theme in search of definition. Monographs of the society for research in child development. 1994;59:25–52. [PubMed] [Google Scholar]
- Tull MT, Gratz KL, Coffey SF, Weiss NH, McDermott MJ. Examining the interactive effect of posttraumatic stress disorder, distress tolerance, and gender on residential substance use disorder treatment retention. Psychology of Addictive Behaviors. 2012 doi: 10.1037/a0029911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Werba BE, Eyberg SM, Boggs S, Algina J. Predicting outcome in parent-child interaction therapy: Success and attrition. Behavior Modification. 2002;30:618–646. doi: 10.1177/0145445504272977. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Sholomskas D, Pottenger M, Prusoff BA, Locke BZ. Assessing depressive symptoms in five psychiatric populations: a validation study. American Journal of Epidemiology. 1977;106:203–214. doi: 10.1093/oxfordjournals.aje.a112455. [DOI] [PubMed] [Google Scholar]
- Woodhouse SS, Ramos-Marcuse F, Ehrlich KB, Warner S, Cassidy J. The role of adolescent attachment in moderating and mediating links between parent and adolescent psychological symptoms. Journal of Clinical Child Adolescent Psychology. 2010;39:51–63. doi: 10.1080/15374410903401096. doi:10.1080/15374410903401096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woodhouse, Zeman J, Cassano M, Perry-Parrish C, Stegall S. Emotion regulation in children and adolescents. Journal of Developmental & Behavioral Pediatrics. 2006;27:155–168. doi: 10.1097/00004703-200604000-00014. [DOI] [PubMed] [Google Scholar]
- Zeman J, Klimes-Dougan B, Cassano M, Adrian M. Measurement issues in emotion research with children and adolescents. Clinical Psychology: Science and Practice. 2007;14:377–401. [Google Scholar]
- Zvolensky MJ, Vujanovic AA, Bernstein A, Leyro T. Distress Tolerance: Theory, measurement, and relations to psychopathology. Current Directions in Psychological Science. 2010;19:406–410. doi: 10.1177/0963721410388642. doi:10.1177/0963721410388642. [DOI] [PMC free article] [PubMed] [Google Scholar]