Abstract
Setting: A rural private health facility, Ruby Medical Centre (RMC), participating in a safe motherhood health voucher system for poor women in Kiambu County, Kenya.
Objectives: Between 2007 and 2013, to determine 1) the number of women who delivered at the RMC, their characteristics and pregnancy-related outcomes, and 2) the number of women who received an incomplete antenatal care (ANC) package and associated factors.
Design: Retrospective cross-sectional study using routine programme data.
Results: During the study period, 2635 women delivered at the RMC: 50% were aged 16–24 years, 60% transferred in from other facilities and 59% started ANC in the third trimester of pregnancy. Of the 2635 women, 1793 (68%) received an incomplete ANC package: 347 (13%) missed essential blood tests, 312 (12%) missed the tetanus toxoid immunisation and 1672 (65%) had fewer than four visits. Presenting late and starting ANC elsewhere were associated with an incomplete package. One pregnancy-related mortality occurred; the stillbirth rate was 10 per 1000 births.
Conclusion: This first assessment of the health voucher system in rural Kenya showed problems in ANC quality. Despite favourable pregnancy-related outcomes, increased efforts should be made to ensure earlier presentation of pregnant women, comprehensive ANC, and more consistent and accurate monitoring of reproductive indicators and interventions.
Keywords: complete ANC package, output-based aid, SORT IT, operational research
Abstract
Contexte : Une structure de santé privée rurale, le Ruby Medical Centre (RMC), participant à un système de bons de traitement de Maternité sans risques destiné à des femmes pauvres du conté de Kiambu au Kenya.
Objectifs : Entre 2007 et 2013, déterminer 1) le nombre de femmes qui ont accouché au RMC, leurs caractéristiques et le devenir de leur grossesse, et 2) le nombre ne bénéficiant que d’un paquet de soins anténataux (ANC) incomplets et les facteurs associés.
Schéma : Etude rétrospective transversale basée sur les données recueillies en routine dans les programmes.
Résultats : Au cours de la période d’étude, 2635 femmes ont accouché au RMC : 50% étaient âgées de 16 à 24 ans, 60% avaient été transférées d’autres structures et 59% avaient débuté les ANC au cours du 3e trimestre. De ces 2635 femmes, 1793 (68%) avaient un paquet d’ANC incomplet : 347 (13%) ont manqué les principaux tests sanguins, 312 (12%) n’ont pas eu de vaccination anti-tétanique et 1672 (65%) ont eu moins de quatre consultations. Un démarrage tardif et des ANC débutés ailleurs étaient associés à un paquet d’ANC incomplet. Un décès lié à la grossesse est survenu et le taux de mortinatalité a été de 10/1000 naissances.
Conclusion : Cette première évaluation du système de bons de traitement dans les zones rurales du Kenya a mis en évidence des problèmes de qualité des ANC. En dépit de l’évolution favorable des grossesses, il est nécessaire d’accroitre les efforts pour faire venir les femmes enceintes plus tôt, offrir des ANC complets et un suivi plus cohérent et précis des indicateurs et des interventions de santé reproductive.
Abstract
Marco de referencia: El Ruby Medical Centre (RMC) es un centro de atención de salud privado en zona rural, que participa en el sistema de cupones por una maternidad sin riesgo en el condado de Kiambu, en Kenia.
Objetivos: Determinar entre el 2007 y el 2013: 1) la cantidad de mujeres cuyo parto se atendió en el RMC, las características de las mujeres y los desenlaces relacionados con el embarazo; y 2) el número de mujeres que recibieron una atención prenatal (ANC) incompleta y los factores asociados con esta situación.
Métodos: Fue este un estudio transversal retrospectivo a partir de los datos del programa corriente.
Resultados: Durante el período del estudio, se atendió el parto de 2635 mujeres en el RMC, el 50% de las cuales tenía entre 16 y 24 años de edad, el 60% acudió como remisión de otros centros de atención y el 59% había comenzado la ANC durante el tercer trimestre del embarazo. De las 2635 mujeres, 1793 recibieron una ANC incompleta (68%) a saber: en 347 no se practicaron los principales exámenes sanguíneos (13%); 312 no recibieron la vacuna con el toxoide antitetánico (12%); y 1672 acudieron a menos de cuatro citas de control (65%). Los factores asociados con una ANC incompleta fueron una presentación tardía al programa y el inicio de la ANC en un centro diferente. Se presentó un caso de mortalidad relacionada con el embarazo y la tasa de mortinatalidad fue de 10 por 1000 nacimientos.
Conclusión: El presente estudio es la primera evaluación del sistema de cupones por una maternidad sin riesgo en la zona rural de Kenia y puso en evidencia problemas en materia de calidad de la ANC. Pese a los desenlaces favorables del embarazo, se precisan iniciativas que fomenten una presentación más temprana de las embarazadas al programa, la ANC integral, y una vigilancia más regular y exacta de los indicadores y las intervenciones en materia de salud reproductiva.
Accessible, good quality antenatal care (ANC) is critical to ensure favourable maternal and neonatal outcomes. While good ANC is provided for >90% of pregnant women in industrialised countries, coverage is far lower in sub-Saharan Africa due to poor health-seeking behaviour, lack of access to services, social and cultural barriers and poverty.1,2 Maternal and perinatal mortality therefore remains high in many African countries.
In Kenya, the maternal mortality ratio was reported at 488 per 100 000 live births in the 2008/2009 Kenya Demographic Health Survey.1 This is a far cry from the projected target of 147/100 000 live births, which would accelerate attainment of the Millennium Development Goal 5 by 2015.3 Impoverished pregnant women are particularly vulnerable due to malnutrition, lower levels of education, less empowerment and financial insecurity, and this often results in no or delayed access to reproductive health services, which in turn compromises quality of care.4 Various strategies have been used to improve the uptake and quality of care, including targeted ANC, conditional cash transfer voucher schemes, subsidised financing, free maternity services and maternity waiting homes for pregnancy and childbirth.5–7
In Kenya, one recent strategy is output-based aid (OBA), a health voucher system that targets low-income mothers, enabling them to obtain a package of antenatal, intrapartum and postpartum care along with the provision of long-term family planning. Unlike the routine established health system in Kenya, where women have to pay out-of-pocket expenses for pregnancy and childbirth, fees paid by women in OBA are highly subsidised, with health facilities being reimbursed by the voucher management agency depending on the services that they have provided to expectant and post-partum mothers.8,9
The OBA project in Kenya was established in 2006 as a collaborative public-private partnership between the Kenyan and German governments, with services being provided to pregnant women in the Nairobi slums and the counties of Kisumu, Kitui and Kiambu.10 A number of health facilities within each of these areas are accredited to provide a package of reproductive health services under the OBA health voucher system. This is designed to provide the safe motherhood package of services in a structured manner and to encourage mothers to attend the recommended scheduled visits and receive the appropriate interventions, with freedom to select their preferred OBA facility.11 The Ruby Medical Centre (RMC), based in Kiambu West, was incorporated into the OBA project in 2007 and is one of 10 OBA accredited health facilities in Kiambu.
The OBA health voucher system has not yet been formally evaluated at the county level. As it is now in its seventh year of implementation, and given the importance of public-private partnership in Kenya, this is an appropriate time to conduct this assessment.12 The aim of the present study was to report on the use of ANC and pregnancy outcomes among women who delivered through the OBA health voucher system at the RMC. Specific objectives were to determine 1) the number of women who delivered at the RMC, their characteristics and pregnancy-related outcomes; and 2) the number of women who received an incomplete ANC package and associated factors.
METHODS
Study design
This was a cross-sectional study using routinely collected programme data.
Setting
General
Kenya is an East African country (population 38 million) with a gross domestic product of USD 882 per capita per year in 2012.13,14 The country is now divided into 47 counties, each with a local administrative bureaucracy, with health care being decentralised to the county level. Health care is not free at the point of care; out-of-pocket expenditures occur for every aspect of diagnosis, treatment and prevention, including reproductive services. However, free maternity services have been offered in government facilities since June 2013.
Study setting
The study was carried out at the RMC, Kiambu West, Rungiri township, 22 km from Nairobi, the capital city of Kenya. The catchment area has a radius of 10–15 km and serves a population of approximately 150 000, consisting mainly of poor subsistence farmers earning <USD 1.00 a day. RMC is a private maternity centre, with 12 beds, a delivery room, an operating theatre and a newborn nursery that handles term babies. All pre-term or low birth weight babies (defined as <2.0 kg) are referred to specialised services. RMC operates as a private-public partnership with the Ministry of Health, with services offering capacity building for health personnel, pregnancy and childbirth services, including caesarean sections, family planning, neonatal immunisation and a rigorous monitoring system in line with Ministry of Health systems and quality assurance. The clinical staff consists of one obstetrician-gynaecologist, one medical officer, one clinical officer-anaesthetist, two general care clinical officers and five midwives. Sick mothers and babies requiring intensive care are referred to Kenyatta National Hospital or Kijabe Mission Hospital.
OBA system
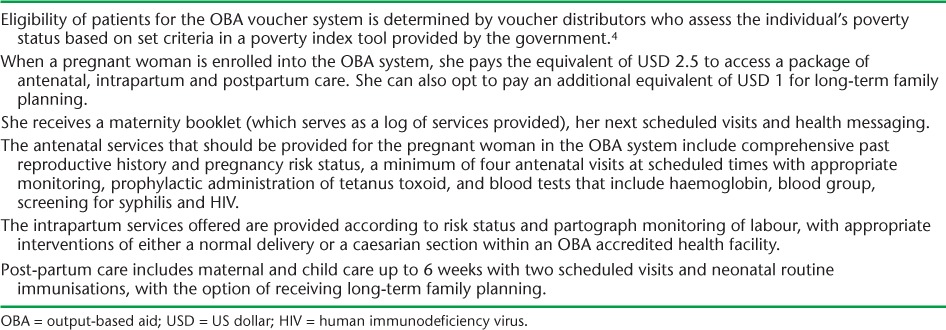
The essential aspects of the OBA voucher system are shown in Table 1. Pregnant women who enrol in an OBA facility are encouraged to stay with that facility for the duration of the pregnancy, the delivery and 6 weeks of post-partum care. However, they may transfer to another of the nine OBA facilities within the county at any stage.
TABLE 1.
Key components of the OBA system in Kenya
Study population
The study population included all women who enrolled and delivered in the OBA health voucher system at the RMC between January 2007 and December 2013.
Data variables
Data variables included numbers enrolled in each quarter, socio-demographic and reproductive characteristics, the use by each woman of the different components of the ANC package, and maternal and perinatal outcomes at delivery. These data were routinely captured in patient file records, Ministry of Health antenatal enrolment records, maternal log booklets and delivery registers, which were extracted into an Excel (Microsoft, Redmond, WA, USA) electronic database maintained by the RMC between August 2013 and April 2014. Data in the electronic database were validated for consistency and checked for missing variables using pre-developed Stata scripts (StataCorp, College Station, TX, USA). A complete ANC package was defined as blood tests for haemoglobin, blood group, screening for syphilis and human immunodeficiency virus (HIV), tetanus toxoid immunisation, and four or more antenatal visits. An incomplete ANC package was defined as failure to undergo one or more of these listed components.
Analysis and statistics
Data were transferred and analysed using EpiData Analysis software (version 2.2.2.182, EpiData Association, Odense, Denmark), and a descriptive analysis was performed. Maternal and neonatal outcomes in women who received a complete ANC package and those who received an incomplete package were compared using the χ2 test, with relative risks (RRs) and 95% confidence intervals (CIs). Levels of significance were set at 0.05. For morbidity statistics, we report disease episodes instead of patient-specific morbidity due to the multiplicity of diagnoses per patient.
Ethics approval
Ethics approval for the study was obtained from the Moi University Institutional Research and Ethics Committee (Eldoret, Kenya) and met the Médecins Sans Frontières (Geneva, Switzerland) Ethics Review Board-approved criteria for the analysis of routinely collected programme data. It also satisfied the requirements of the Ethics Advisory Group of the International Union Against Tuberculosis and Lung Disease, Paris, France, and met their approval.
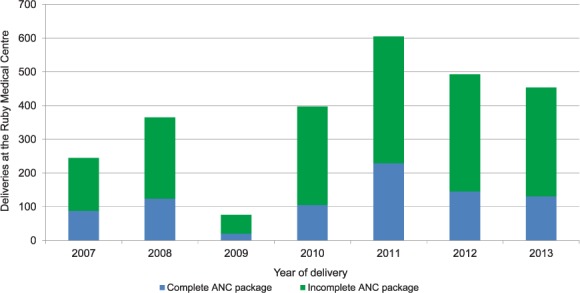
RESULTS
A total of 2635 women were enrolled and delivered at the RMC during the study period, (numbers for each quarter are shown in Figure 1). There was a striking decline in deliveries starting in the second half of 2008 as a result of both reaccreditation processes and financial constraints within the OBA health voucher system and another decline in the second half of 2013, coinciding with the Ministry of Health’s introduction of free maternity care in the country.
FIGURE 1.
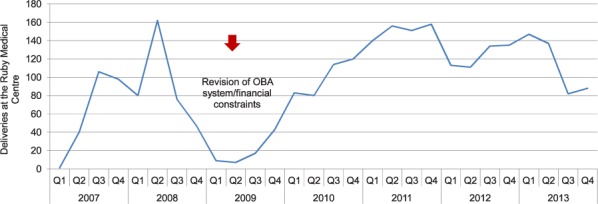
Number of pregnant women who delivered in each quarter at the Ruby Medical Centre, Kiambu, Kenya, 2007–2013. OBA = output-based aid; Q = quarter.
Socio-demographic and reproductive characteristics of women delivering at RMC are shown in Table 2. Key findings were that half of the women were aged 16–24 years, most were married and housewives, and only about half had primary school education. Most women already had children. There was poor documentation of pregnancy risk status, but where it was indicated the majority (402/427) were high risk. Two thirds of women started ANC in OBA clinics elsewhere and transferred to the RMC for their delivery. Figure 2 shows the gestational age in weeks of women presenting for their first ANC visit. It should be noted that 1548 (59%) women started their care in the third trimester.
TABLE 2.
Socio-demographic and reproductive characteristics of all pregnant women who delivered at the Ruby Medical Centre, Kiambu, Kenya, 2007–2013
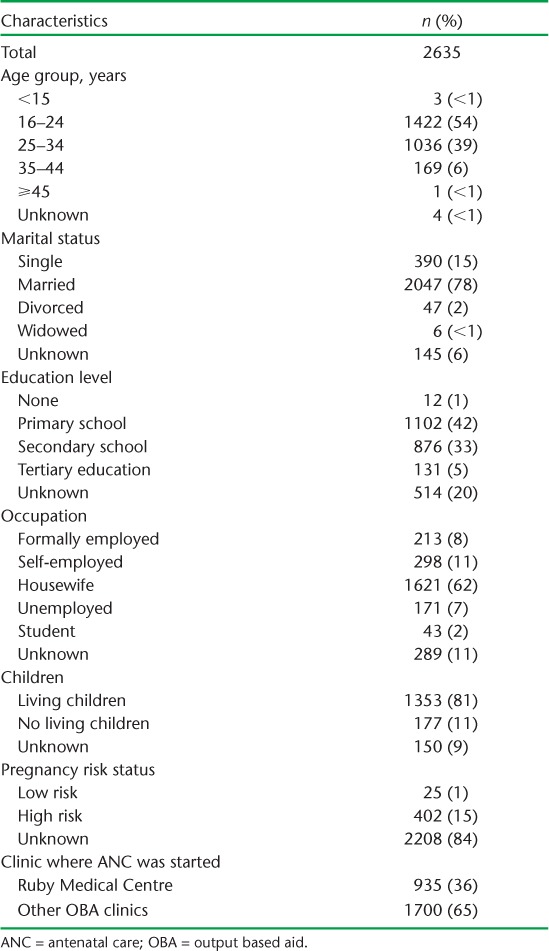
FIGURE 2.
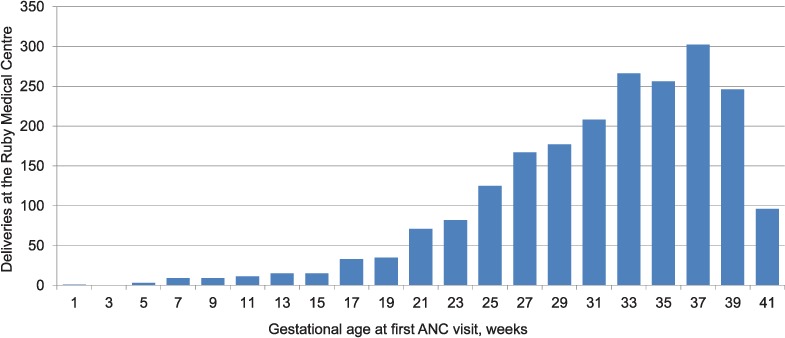
Gestational age at first ANC visit for women who delivered at the Ruby Medical Centre, Kiambu, Kenya, 2007–2013. ANC = antenatal care.
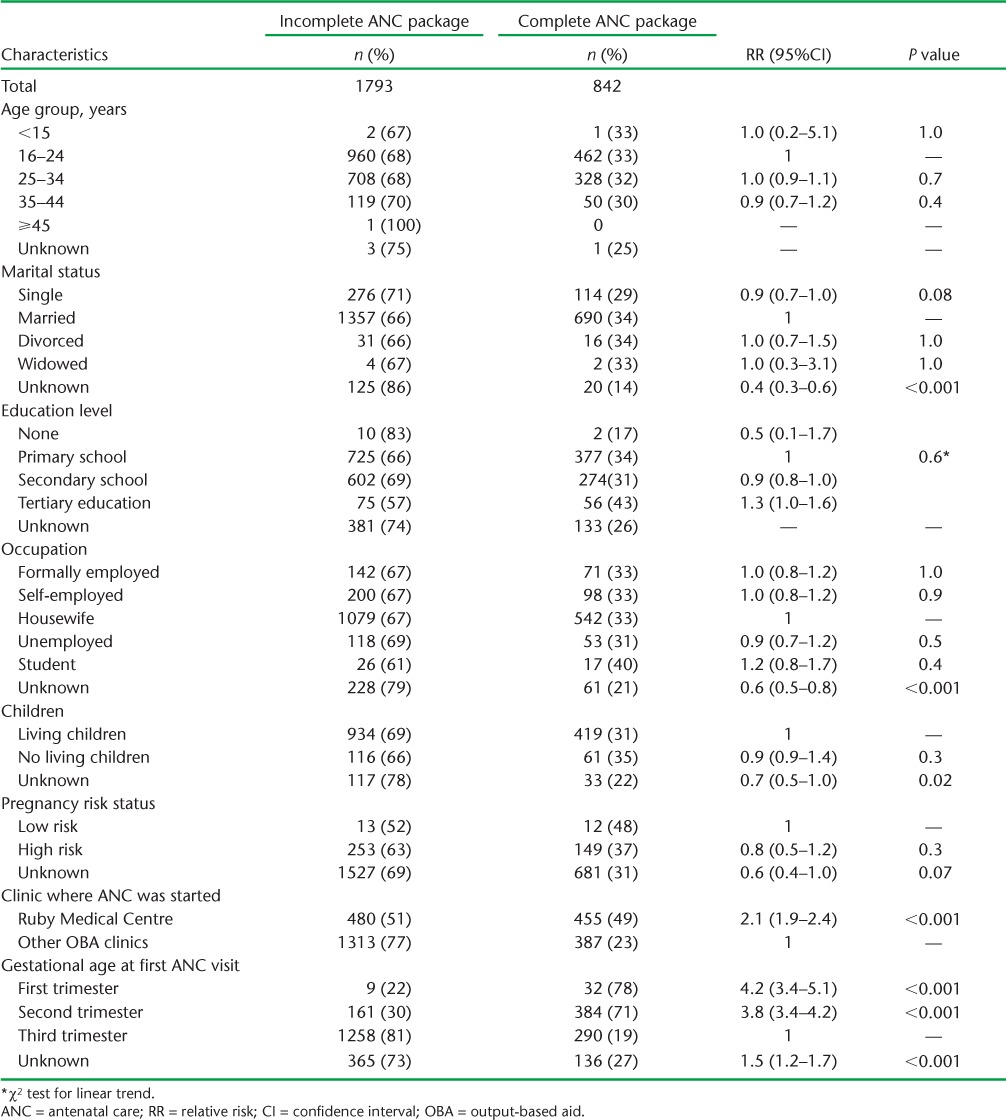
The numbers and proportions of women receiving a complete or incomplete ANC package each year are shown in Figure 3: 842 (32%) received the complete package. Of the 1793 women who received an incomplete package, the number and proportion that missed different components of the package are shown in Table 3. In summary, 13% missed one or more laboratory tests, 12% missed their tetanus toxoid injection and 66% had fewer than four antenatal care visits. Factors associated with receiving a complete or an incomplete ANC package are shown in Table 4. Receiving an incomplete care package was associated with starting ANC elsewhere and presenting in the third trimester.
FIGURE 3.
Pregnant women who delivered and received a complete or incomplete ANC package at the Ruby Medical Centre, Kiambu, Kenya, 2007–2013. ANC = antenatal care.
TABLE 3.
Pregnant women who delivered and received an incomplete ANC package at the Ruby Medical Centre, Kiambu, Kenya, 2007–2013
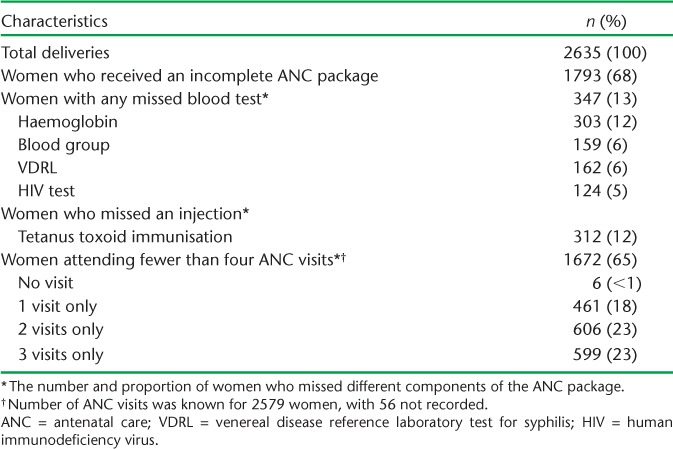
TABLE 4.
Factors associated with receiving a complete or incomplete ANC package in women who delivered at the Ruby Medical Centre, Kiambu, Kenya, 2007–2013
Two thousand, two hundred and sixteen (84%) women had a spontaneous vaginal delivery, 8 (<1%) had an assisted vaginal delivery and 409 (16%) had a caesarean section: no record of the mode of delivery was found for two patients. Maternal morbidities included postpartum haemorrhage (37/151, 25%), obstructed labour (17/151, 11%), pre-eclampsia/eclampsia (25/151, 17%) and HIV (2/151, 1%). There was one pregnancy-related maternal death from eclampsia. Among neonates, there were 2695 (99%) live births, 28 (1%) still births (16 fresh and 12 macerated) and 2 with no documentation, giving a still birth rate of 10 per 1000 births. Among the causes of neonatal morbidity, birth asphyxia (57/119, 48%), respiratory distress (30/119, 25%) and prematurity (26/119, 22%) were common. There was no significant difference in maternal or perinatal outcomes between those who received a complete and those with an incomplete ANC package.
DISCUSSION
This is the first formal assessment of the OBA health voucher system in a large county in Kenya. Over the 7-year period, the system worked well, with over 2600 women delivering at the RMC, and resulted in excellent maternal and perinatal outcomes compared with national figures.1 The health voucher system in general targeted young married housewives, the majority of whom already had children.
An interesting finding was that two thirds of women started ANC in another OBA-accredited facility, generally in the public sector, and transferred to the RMC for delivery. Many of these women also presented for ANC late in their third trimester of pregnancy. The reasons for not attending the RMC first are not clear, but may be related to health-seeking behaviour, the proximity of their homes to the health facility,2 transport costs and enrolment bureaucracy.
Only a third of the women received the complete ANC package. The main reason for not receiving the full package was failure to visit the ANC on four or more occasions, one of the key factors recommended by the World Health Organization for achieving the full life saving potential that ANC promises for women and babies.15 A proportion of women also missed their tetanus toxoid immunisation and blood tests for haemoglobin, syphilis and HIV. Ascertaining a woman’s haemoglobin level is essential, as anaemia in the antenatal period can be corrected with iron and folate supplementation, and precautionary preparations can be made before delivery, as haemorrhage is a major cause of maternal mortality.16 Maternal syphilis is an important cause of stillbirth, and is treatable.15 In Kenya and other African countries with high HIV prevalence,14,17 HIV testing is crucial to identify HIV-infected women, prevent mother-to-child transmission of HIV and ensure maternal and childhood survival.18
Although perinatal outcomes were good, there were 28 stillbirths. In worldwide data-collating systems, stillbirths do not count. In 2009, there were an estimated 2.6 million stillbirths, the majority in South Asia and sub-Saharan Africa, and although these are thought to be declining, progress is not as good as with maternal mortality and deaths in infants and children aged <5 years.19 Stillbirths cause considerable maternal grief, stigma and marginalisation, with the mother’s sins and evil spirits being held by rural communities to be important causes.20 It is believed that appropriate high-quality interventions in the pre-conception, antenatal and intrapartum periods could reduce the incidence of stillbirths by 33%.21
The strengths of this study were the large number of women included, the 7-year period of observation and the generally good documentation of socio-demographic characteristics, ANC interventions and pregnancy-related outcomes. Attention was also paid to following internationally agreed recommendations for reporting on observational studies.22,23
There were some limitations. First, the study design would have been strengthened by including a comparator group. However, this was difficult to do within the clinic, as the voucher system targeted women from low-income settings, while the clinic provided services to private patients. Furthermore, there were no other similar clinics not running a voucher system with which to compare data. Second, recording of reproductive characteristics focusing on pregnancy risk status was poor, and this needs to be improved in future. Third, we did not look at the county uptake of care in the OBA health voucher system; this would have required information on all deliveries in the county between 2007 and 2013. Studies have shown an increased uptake of institutional delivery using maternal health voucher schemes in South Asia,24,25 and this is an area of work that we would like to look into in future.
The study has several implications. First, the striking decline in the number of deliveries at the RMC in 2008 and 2009 was associated with bureaucratic hurdles and financial constraints, and these must be anticipated and prevented so that services are not interrupted. Such management practices are now in place. Second, women should be strongly encouraged to present earlier in pregnancy so that they can receive optimal benefit from appropriate ANC interventions that are known to reduce maternal and perinatal morbidity and mortality.15 One ANC visit and late presentation is not enough to predict or prevent obstetric complications.26 More needs to be done to provide ANC at the community level close to women’s homes. Third, documentation should be improved so that there is comprehensive, good-quality data, especially for reproductive health characteristics. In these settings, there is a need for regular, structured and rigorous monitoring of interventions to determine whether the quality of care is good and whether this is making a difference to maternal health, and a cohort analysis approach might be useful.27 Finally, further quantitative and qualitative research is needed to better understand the dynamics and client perspectives of the OBA health voucher system, whether this can be further decentralised into the community and whether it is still viable now that national policy includes free maternal care.
In conclusion, this first formal assessment of the health voucher system in rural Kenya uncovered problems with the quality of ANC. Despite favourable pregnancy-related outcomes, increased efforts should be made to ensure earlier presentation of pregnant women, comprehensive ANC, and more consistent and accurate monitoring of reproductive indicators and interventions.
Acknowledgments
This research was conducted through the Structured Operational Research and Training Initiative (SORT IT), a global partnership led by the Special Programme for Research and Training in Tropical Diseases at the World Health Organization (WHO/TDR, Geneva, Switzerland). The model is based on a course developed jointly by the International Union Against Tuberculosis and Lung Disease (The Union, Paris, France) and Médecins Sans Frontières (MSF, Brussels Operational Centre, Luxembourg). The specific SORT IT programme which resulted in this publication was jointly developed and implemented by: the Operational Research Unit (LUXOR), MSF, Brussels Operational Center, Luxembourg; the Centre for Operational Research, The Union, Paris, France; The Union South-East Asia Regional Office, New Delhi, India; and the Centre for International Health, University of Bergen, Bergen, Norway.
Special thanks go to the Administrator of Ruby Medical Centre, F C Njoroge, and the record clerks who entered the data, D M Gitari and R M Nthiga.
The programme was funded by MSF, The Union, the Department for International Development (London, UK) and the WHO. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. In accordance with the WHO’s open-access publication policy for all work funded by WHO or authored/co-authored by WHO staff members, the WHO retains the copyright of this publication through a Creative Commons Attribution Intergovernmental Organizations licence (http://creativecommons.org/licenses/by/3.0/igo/legalcode), which permits unrestricted use, distribution and reproduction in any medium provided the original work is properly cited.
Footnotes
Conflict of interest: none declared.
References
- 1.Kenya National Bureau of Statistics. Kenya demographic and health survey 2008–09. Nairobi, Kenya: Kenya NBS; 2010. http://apps.who.int/medicinedocs/en/m/abstract/Js17116e/ Accessed November 2014. [Google Scholar]
- 2.Thaddeus S, Maine D. Too far to walk: maternal mortality in context. Newsl Womens Glob Netw Reprod Rights. 1991;(36):22–24. [PubMed] [Google Scholar]
- 3.Bhutta Z A, Chopra M, Axelson H et al. Countdown to 2015 decade report (2000–10): taking stock of maternal, newborn, and child survival. Lancet. 2010;375:2032–2044. doi: 10.1016/S0140-6736(10)60678-2. [DOI] [PubMed] [Google Scholar]
- 4.Armstrong S. Vouchers: making motherhood safer for Kenya’s poorest women: Germany’s contribution to the achievement of MDG5 in Kenya. Bonn, West Germany: Federal Ministry for Economic Cooperation and Development; 2012. http://german-practice-collection.org/en/successful-programmes/sexual-health-and-rights/vouchers-making-motherhood-safer-for-kenyas-poorest-women Accessed November 2014. [Google Scholar]
- 5.Malqvist M, Yuan B, Trygg N, Selling K, Thomsen S. Targeted interventions for improved equity in maternal and child health in low- and middle-income settings: a systematic review and meta-analysis. PLOS ONE. 2013;8:e66453. doi: 10.1371/journal.pone.0066453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Carroli G, Villar J, Piaggio G et al. WHO systematic review of randomised controlled trials of routine antenatal care. Lancet. 2001;357:1565–1570. doi: 10.1016/S0140-6736(00)04723-1. [DOI] [PubMed] [Google Scholar]
- 7.Zomorodian L M, Massawe E, Makundi J P, Mitchell C M, Eschenbach D A. Obstetric care preferences and desire for maternity waiting homes among labor and delivery patients in Arusha, Tanzania. Obstet Gynecol. 2014;123(Suppl 1):179S–180S. [Google Scholar]
- 8.Abuya T, Njuki R, Warren C E et al. A policy analysis of the implementation of a reproductive health vouchers program in Kenya. BMC Public Health. 2012;12:540. doi: 10.1186/1471-2458-12-540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Janisch C P, Albrecht M, Wolfschuetz A, Kundu F, Klein S. Vouchers for health: a demand side output-based aid approach to reproductive health services in Kenya. Glob Public Health. 2010;5:578–594. doi: 10.1080/17441690903436573. [DOI] [PubMed] [Google Scholar]
- 10.Centre for Health Market Innovations. Program: Kenya Output-Based Aid Voucher Program. Washington DC, USA: CHMI; 2005. http://healthmarket-innovations.org/program/kenya-output-based-aid-voucher-program Accessed November 2014. [Google Scholar]
- 11.Maine D, Rosenfield A. The Safe Motherhood Initiative: why has it stalled? Am J Public Health. 1999;89:480–482. doi: 10.2105/ajph.89.4.480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sambo L G, Kirigia J M. Africa’s health: could the private sector accelerate the progress towards health MDGs? Int Arch Med. 2011;4:39. doi: 10.1186/1755-7682-4-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Global Property Guide. GDP per capita: Kenya compared to continent. Bristol, UK: Global Property Guide; 2013. http://www.globalpropertyguide.com/Africa/Kenya/gdp-per-capita Accessed November 2014. [Google Scholar]
- 14.World Health Organization. World Health Statistics, 2014. Geneva, Switzerland: WHO; 2014. [Google Scholar]
- 15.Lincetto O, Mothebesoane-Anoh S, Gomez P, Munjanja S. Antenatal care. In: Lawn J, Kerber K, editors. Opportunities for Africa’s newborns: practical data, policy and programmatic support for newborn care in Africa. Geneva, Switzerland: World Health Organization; 2006. pp. 51–62. [Google Scholar]
- 16.Kassebaum N, Bertozzi A V, Cozzeshall M et al. Global, regional and national levels and causes of maternal mortality during 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2014;384:980–1004. doi: 10.1016/S0140-6736(14)60696-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.National AIDS and STI Control Programme, Ministry of Heath, Kenya. Kenya AIDS Indicator Survey Preliminary Report 2012. Kenya MoH; 2013. http://nascop.or.ke/library/3d/Preliminary%20Report%20for%20Kenya%20AIDS%20indicator%20survey%202012.pdf Accessed November 2014. [Google Scholar]
- 18.World Health Organization. Consolidated guidelines on the use of antiretroviral drugs for treating and preventing HIV infection. Recommendations for a public health approach. Geneva, Switzerland: WHO; 2013. http://apps.who.int/iris/bitstream/10665/85321/1/9789241505727_eng.pdf Accessed November 2014. [PubMed] [Google Scholar]
- 19.Cousens S, Blencowe H, Stanton C et al. National, regional, and worldwide estimates of stillbirth rates in 2009 with trends since 1995: a systematic analysis. Lancet. 2011;377:1319–1330. doi: 10.1016/S0140-6736(10)62310-0. [DOI] [PubMed] [Google Scholar]
- 20.Froen J F, Cacciatore J, McClure E M et al. Stillbirths: why they matter. Lancet. 2011;377:1353–1366. doi: 10.1016/S0140-6736(10)62232-5. [DOI] [PubMed] [Google Scholar]
- 21.Bhutta Z A, Das J K, Bahl R et al. Can available interventions end preventable deaths in mothers, newborn babies and stillbirths, and at what cost? Lancet. 2014;384:347–370. doi: 10.1016/S0140-6736(14)60792-3. [DOI] [PubMed] [Google Scholar]
- 22.Von Elm E, Altman D G, Egger M, Pocock S J, Gotzsche P, Vandenbroucke J P, for the STROBE initiative The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. 2007;370:1453–1457. doi: 10.1016/S0140-6736(07)61602-X. [DOI] [PubMed] [Google Scholar]
- 23.Edginton M, Enarson D, Zachariah R et al. Why ethics is indispensible for good-quality operational research. Public Health Action. 2012;2:21–22. doi: 10.5588/pha.12.0001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Agha S. Impact of a maternal health voucher scheme on institutional delivery among low income women in Pakistan. Reproductive Health. 2011;8:10. doi: 10.1186/1742-4755-8-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ahmed S, Khan M M. Is demand-side financing equity enhancing? Lessons from a maternal health voucher scheme in Bangladesh. Soc Sci Med. 2011;72:1704–1710. doi: 10.1016/j.socscimed.2011.03.031. [DOI] [PubMed] [Google Scholar]
- 26.Ching P K, Hall M H, MacGillivray I. An audit of antenatal care: the value of the first antenatal visit. BMJ. 1980;281:1184–1186. doi: 10.1136/bmj.281.6249.1184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Harries A D, Jahn A, Ben-Smith A et al. Cohort analysis of antenatal care and delivery outcomes in pregnancy: a basis for improving maternal health. Public Health Action. 2014;4:75–78. doi: 10.5588/pha.13.0103. [DOI] [PMC free article] [PubMed] [Google Scholar]


