Figure 4.
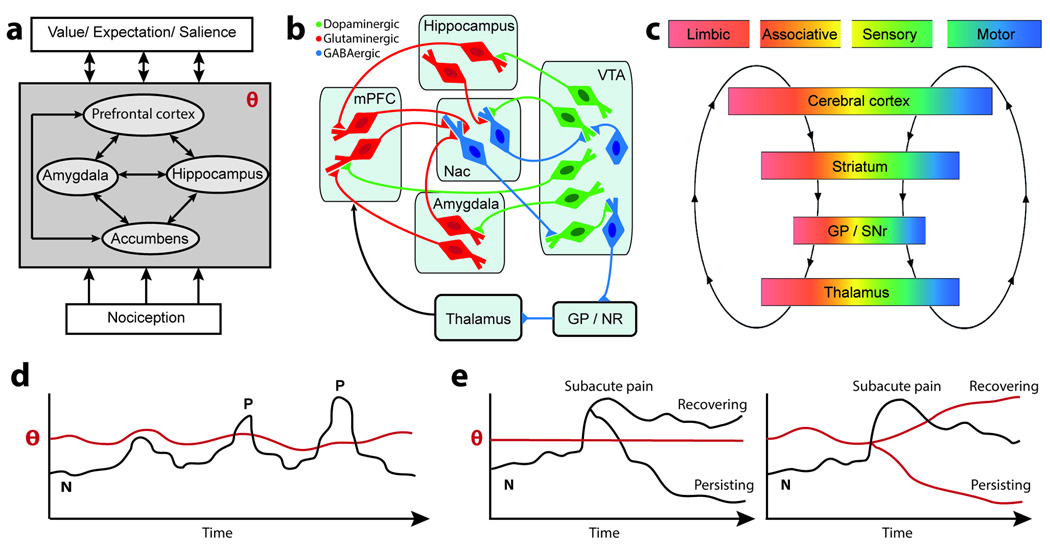
Transition to chronic pain may be deconstructed to four component phases: Predisposition, injury or inciting event, a transition period, and a maintenance phase. Brain circuitry and their interactions across the phases are illustrated in human brain imaging studies, a–h. a. Specific brain white matter regional properties (red) impart risk for developing chronic pain following an acute episode of back pain (Mansour et al., 2013). b. Limbic brain structural properties may also impart risk for pain chronification (e.g. shape and/or size of the hippocampus) (Mutso et al., 2012). c. In the transition phase, strength of information exchange between the prefrontal cortex and accumbens, after an end organ injury, determines long-term pain chronification (Baliki et al., 2012). d. The transition process is the influence of predisposing brain factors in combination with the injury-induced nociceptive signals that control mesolimbic learning mechanisms, altogether determining extent of prefrontal-accumbens information exchange (modulating θ in figure 2). Chronification of pain gives rise to: e. condition specific subjective pain-related brain activity patterns (Baliki et al., 2006; Hashmi et al., 2013; Parks et al., 2011), f. increased information exchange within the hippocampus and between the hippocampus and the cortex (Mutso et al., 2013), g. reorganization of brain grey matter regional similarity (Baliki et al., 2011), and h. distortions in information sharing in resting state brain activity, specifically brain activity phase relationship between the default mode network and the rest of the brain shows chronic pain type-specific patterns (Baliki et al., 2014b).
In rodent models for persistent pain, the four phases are better conceptualized as pre-injury manipulations that influence post-injury pain-like behavior, and early and late post-injury consequences. Supraspinal circuits implicated in the rodent four phases of pain persistence are highlighted in 1–9: 1. Bilateral lesion of the rat basolateral amygdala (BLA) diminishes post-injury tactile allodynia for 28 days after neuropathy (Li et al., 2013). 2. Lidocaine infusion within accumbens in the rat diminishes post-injury tactile allodynia for the duration of infusion (14 days), after a neuropathic injury (spared nerve injury, SNI) (Chang et al., 2014). 3. Hours following induction of an arthritis model in the rat, amygdala neurons become hyperexcitable (Neugebauer et al., 2003). 4. Five days after SNI neuropathy in the rat, accumbens covariance of receptor gene expression is upregulated (Chang et al., 2014), and 5. dendritic size and branchings of prefrontal pyramidal neurons are expanded (Metz et al., 2009). 6. Fifteen days after SNI neuropathy adult hippocampal neurogenesis is downregulated (Mutso et al., 2012). 7. Accumbens medium spiny neurons with dopamine D2 receptors show decreased AMPA/NMDA ratio in neuropathic injured rodents (Schwartz et al., 2014). 8. Resting state whole-brain functional network in the anesthetized rat shows increased (red) and decreased (blue) functional connections 28 days after SNI neuropathy relative to sham injury (Baliki et al., 2014a). 9. Six months following neuropathic injury prefrontal (PFC) cortical grey matter volume is decreased in the rat (Seminowicz et al., 2009).
Overall, the human data illustrates brain risk factors for, and brain reorganization with, chronification of pain. The rodent results show persistent painlike behavior is dependent on, and in turn reorganizes, limbic brain circuitry.