Abstract
BACKGROUND AND OBJECTIVES:
Diagnostic codes are used widely within health care for billing, quality assessment, and to measure clinical outcomes. The US health care system will transition to the International Classification of Diseases, 10th Revision, Clinical Modification (ICD-10-CM), in October 2015. Little is known about how this transition will affect pediatric practices. The objective of this study was to examine how the transition to ICD-10-CM may result in ambiguity of clinical information and financial disruption for pediatricians.
METHODS:
Using a statewide data set from Illinois Medicaid specified for pediatricians, 2708 International Classification of Diseases, Ninth Revision, Clinical Modification, diagnosis codes were identified. Diagnosis codes were categorized into 1 of 5 categories: identity, class-to-subclass, subclass-to-class, convoluted, and no translation. The convoluted and high-cost diagnostic codes (n = 636) were analyzed for accuracy and categorized into “information loss,” “overlapping categories,” “inconsistent,” and “consistent.” Finally, reimbursement by Medicaid was calculated for each category.
RESULTS:
Twenty-six percent of pediatric diagnosis codes are convoluted, which represents 21% of Illinois Medicaid pediatric patient encounters and 16% of reimbursement. The diagnosis codes represented by information loss (3.6%), overlapping categories (3.2%), and inconsistent (1.2%) represent 8% of Medicaid pediatric reimbursement.
CONCLUSIONS:
The potential for financial disruption and administrative errors from 8% of reimbursement diagnosis codes necessitates special attention to these codes in preparing for the transition to ICD-10-CM for pediatric practices.
Keywords: ICD-9-CM, ICD-10-CM, diagnostic codes, health informatics, convolution
What’s Known on This Subject:
The US health care system transition to the ICD-10-CM will occur in October 2015. The logistical and financial impact of the transition for billing codes frequently used by pediatricians has not been studied.
What This Study Adds:
The findings of this study evaluate the government-provided mappings from ICD-9-CM to ICD-10-CM for accuracy and provide the diagnostic codes used by pediatricians, which may be adversely affected by the transition to ICD-10-CM.
Diagnostic codes are not only used for billing medical services but also to measure quality, predict clinical outcomes, and anticipate future needs (staffing, purchasing) by health care systems.1–4 The Centers for Medicare and Medicaid Services (CMS) mandated the US health system transition from the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) to the International Classification of Diseases, 10th Revision, Clinical Modification (ICD-10-CM) by October 1, 2015.5 The ICD-10-CM includes ∼68 000 codes, compared with 14 000 codes in the ICD-9-CM, and greater detail is embedded within each ICD-10-CM code.6 Compared with ICD-9-CM, ICD-10-CM is more flexible by accommodating advances in medicine and technology because new codes can be incorporated over time and it more accurately codes ambulatory encounters, including primary care and preventive health visits.6 Implementation of ICD-10-CM is estimated to cost from $83 000 to >$2 million per practice, depending on size.7 A number of previous reports have discussed the transition from different perspectives.8–11
Most countries transitioned to either the World Health Organization version of ICD-10 or developed their own version of ICD-10 in the 1990s. An analysis of the Swiss experience found that the accuracy of administrative data coded with ICD-10 improved somewhat over the 5 years after implementation, but accuracy varied by condition.12 In Canada, a comparison between ICD-9-CM and ICD-10-CA revealed similar validity of administrative data in documenting clinical conditions, and the implementation of ICD-10-CA did not improve the quality of the data.13 Worldwide, transitioning to ICD-10 has had a variable impact on data quality and accuracy; however, the impact of the transition on billing codes frequently used by pediatricians has not been studied.3,12 The objective of this study was to examine how the transition to ICD-10-CM may result in ambiguity of clinical information and financial disruption for pediatricians.
Methods
Overview
Pediatric ICD-9-CM codes were obtained from Illinois Medicaid and were mapped to ICD-10-CM codes by using CMS General Equivalent Mappings (GEMs), a tool created by the CMS and the Centers for Disease Control and Prevention to assist with the conversion between ICD-9-CM and ICD-10-CM codes.5,14 The mappings were examined by pediatricians for clinical accuracy, and financial analysis of the findings was conducted. The study was approved by the University of Illinois Institutional Review Board.
Data Set
We used the statewide data set of Illinois Medicaid ICD-9-CM data for a 1-year (2010) complete billing picture for all patients identified as primary care patients of the University of Illinois system in the month of April 2011. All physician bills were labeled by medical specialty and subspecialty by Medicaid, which included the amount of money the state paid for each claim. The data set was then filtered for bills submitted by a pediatrician including general pediatricians and pediatric subspecialists. A total of 2708 diagnosis codes were used by pediatricians in a total of 174 500 patient encounters for a total payment by Medicaid of $12 298 520. The diagnosis code 999.99 was excluded from analysis because it is not an official ICD-9-CM code and has no defined clinical meaning.
Mapping ICD-9-CM to ICD-10-CM Codes
The CMS GEMs5 directional mapping of codes from ICD-9-CM to ICD-10-CM, and a separate file for ICD-10-CM to ICD-9-CM, was used to create the online analysis tool (version 1.0) and to map the billing codes.14 A total of >100 000 mappings from ICD-9-CM to ICD-10-CM and ICD-10-CM to ICD-9-CM exist.
Categorization of Complexity of Mapping
After mapping, all the ICD-9-CM codes were categorized for the complexity of transition to ICD-10-CM. Boyd et al14 provided classification for mapping on the basis of on how codes associate with each other. The ICD-9-CM codes were categorized into 5 categories on the basis of how they map to ICD-10-CM: identity (where the codes are equivalent), class-to-subclass (1 ICD-9-CM code going to multiple ICD-10-CM codes), subclass-to-class (multiple ICD-9-CM codes to 1 ICD-10-CM code), no transition (no mapping to ICD-10-CM), and convoluted (a complex mapping of ICD-9-CM to and from ICD-10-CM; see Fig 1).14 The first 4 categories include codes where the transition is straightforward and easy to identify; however, the convoluted codes have complex mappings making the transition difficult.
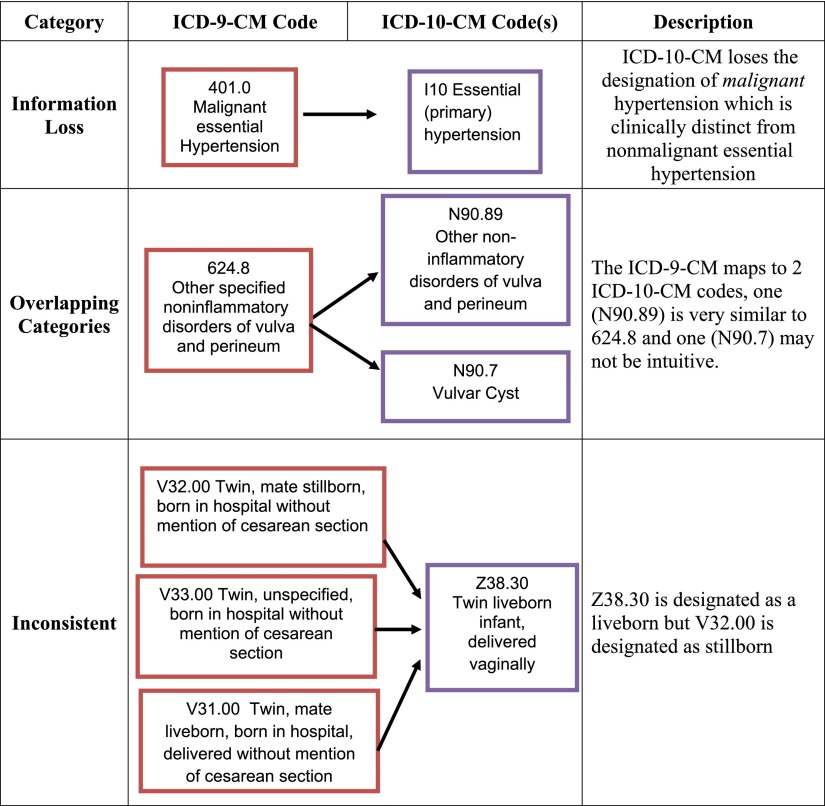
FIGURE 1.
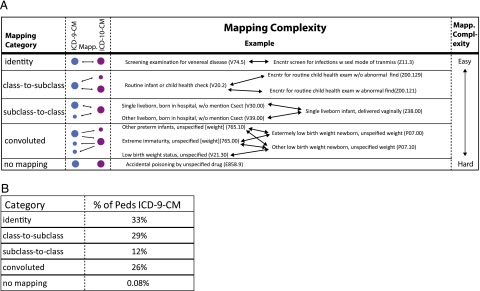
Mapping complexity (A) and category (B) of diagnosis codes. Csect, C-section; Encntr, encounter; find, finding; Peds, pediatrics; Sexl, sexually; transmiss, transmission.
Data Analysis
After the pediatric ICD-9-CM codes were mapped to ICD-10-CM codes and labeled into the above 5 categories,14 an initial patient visit count and cost analysis were performed for each category. To appreciate potential clinical complexity inherent in the transition to ICD-10-CM, the convoluted codes were evaluated by physicians and classified into to 1 of 4 categories: information loss, overlapping categories, inconsistent, or consistent. “Information loss” was used when the transition obscures a clinically important diagnostic distinction, resulting in a potential loss of relevant clinical detail. “Overlapping category” was used when the transition results in a distinction without a clinically relevant difference or could result in confusion for appropriate code assignment. The overlapping category included ICD-9-CM codes that mapped to ICD-10-CM codes where additional nonintuitive clinical information was needed to understand the mapping. “Inconsistent” was used when ICD-10-CM codes were clinically different than the ICD-9-CM codes to which they mapped. The “consistent” category was used when the transition resulted in a consistent and clinically intuitive ICD-10-CM code (see Fig 2). Every convoluted code was analyzed by at least 2 independent physicians (R.C., L.W., G.M., S.R.-C., H.N.), and all discrepancies in classification were rectified by the group. To calculate the total financial impact of the different categories, the percentage of cost was divided by the total cost of all pediatric bills paid by Medicaid in the state of Illinois to reflect a percentage of overall costs related to pediatricians.
FIGURE 2.
Evaluation categories: category examples for ICD-9-CM codes with convoluted mapping transitions to ICD-10-CM codes.
Five physicians coded the mappings and were instructed to focus only on the clinical accuracy of each mapping. Physicians were selected to be a mix of practicing pediatricians and resident physicians. We included senior resident physicians to balance any bias that could exist from more seasoned physicians whose coding practices may be more likely to be unintentionally influenced by reimbursement rates or clinical experiences. None of the physicians had expertise in billing or coding outside of on-the-job experience as a practicing physician.
Results
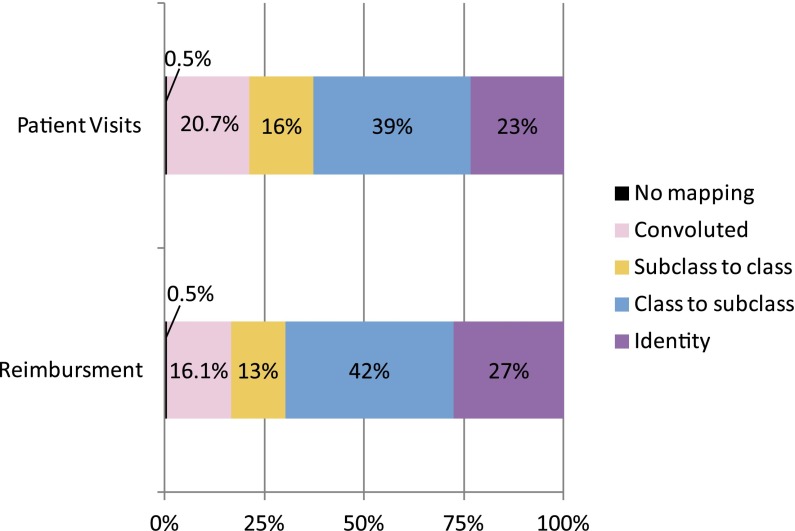
Of the 2708 diagnosis codes, we found 26% of all pediatric ICD-9-CM codes and 21% of pediatric patient visits associated with convoluted codes (Figs 1 and 3). Only 27 ICD-9-CM codes had no ICD-10-CM mapping due to diagnosis codes being redacted or no translation (Figs 1 and 3). Code 999.99, which was not included in the analysis, had $264 181 in payments and 128 432 visits associated with it. Code classification discrepancies were found for 132 codes (21%). The team of physicians reviewed every discrepancy and came to a consensus on the classification. The majority of discrepancies (111 of 132) involved minor differences in clinical interpretation of the mapping.
FIGURE 3.
Percentage of patient visits and reimbursement associated with the coding categories.
Of the 636 convoluted codes analyzed by pediatricians for accuracy, nearly 40% were categorized into the following 3 categories: information loss (14%), overlapping categories (18%), or inconsistent categories (7%) (Table 1). ICD-9-CM codes related to pregnancy and postpartum complications in which the transition to ICD-10-CM required additional clinical information were included in the overlapping category. (See the Supplemental Information for a list of specific ICD-9-CM codes.)
TABLE 1.
Analyzed Pediatric ICD-9-CM Codes of All Pediatric ICD-9-CM Codes in Illinois Medicaid
| Number of Analyzed Codesa (N = 636) | Codes Analyzed, % | Total Illinois Medicaid Diagnosis Codes, % | Reimbursement (% of Total Reimbursement) | |
|---|---|---|---|---|
| Information loss | 88 | 14 | 2.5 | $455 320.84 (3.6) |
| Overlapping categories | 115 | 18 | 3.2 | $399 302.13 (3.2) |
| Inconsistent | 42 | 7 | 1 | $156 637 (1.2) |
| Consistent | 385 | 61 | 10 | $1 970 000 (15.7) |
| Unanalyzed transition | — | — | 83.3 | $9 300 000 (75) |
The last row represents the percentage of codes and cost that were not analyzed by the pediatricians. Overlapping categories at 3.2% of codes and 3.2% of overall cost is the largest contributor to clinically incorrect concepts.
Six codes had no mapping and were excluded from analysis.
Illinois Medicaid reimbursements associated with ICD-9-CM codes categorized as the information loss category during translation to ICD-10-CM totaled $455 320 (3.6% of total cost), the overlapping category totaled $399 302 (3.2% of total cost), and the inconsistent category totaled $156 637 (1.2% of total cost).
Discussion
Coding data are used broadly within health care for billing, surveillance (infections, mortality, etc), quality assessment, and administrative decisions (staffing needs, supply needs, etc). Although the quality of ICD-9-CM data has been called into question,15 the US health care system relies on diagnostic coding data. We found the 26% of pediatric ICD-9-CM codes were convoluted (ie, complex mapping). A similar analysis revealed that 18% of adult oncology codes, 31% of emergency department codes, and 55% of hospital procedure codes are convoluted, showing variability in potential coding challenges by type of practice and the importance of understanding potential issues associated with codes commonly used by each specialty (A.D.B., unpublished data).14,16 To assist with analysis of data that span the transition time frame (2015–2016), the American Medical Association suggests mapping in the direction with the most data (initially map ICD-10-CM back to ICD-9-CM; then, as more ICD-10-CM codes are used, map ICD-9-CM to ICD-10-CM).17 However, using the GEMs files for simple transitions will miss a large number of codes: for example, if mapping from ICD-9-CM to ICD-10-CM using GEMs you map to only 24% of ICD-10-CM codes. Alternately, if mapping from ICD-10-CM to ICD-9-CM using GEMs you map to only 70% of ICD-9-CM codes.18 Thus, it is important to note that simple mapping without examining the codes in detail could result in underutilization of a substantial number of codes.
The convoluted codes categorized as information loss, overlapping categories, or inconsistent have the potential to cause inaccuracies during the transition to ICD-10-CM, which may lead to adverse consequences, including financial loss from billing errors, errors in surveillance, and inaccurate administrative data. The overlapping category accounted for transitions in which nonintuitive details are needed to understand which ICD-10-CM code is accurate. For example, ICD-9-CM code 528.9 (other and unspecified disease of the oral soft tissue) maps to 4 ICD-10-CM codes: E08.638 (diabetes due to underlying condition with other oral complication), E09.638 (drug- or chemical-induced diabetes with other oral complication), K13.70 (unspecified lesions of oral mucosa), and K13.79 (other lesions of oral mucosa). All 4 of the ICD-10-CM codes could encompass “other diseases of oral soft tissues”; thus, it may not be intuitive when to select K13.70 versus K13.79, especially if nonclinical individuals conduct the coding. The information loss category accounted for 14% of pediatric ICD-9-CM codes, which could result in a loss of clinically relevant information. For example, ICD-9-CM code 385.83 (retained foreign body of middle ear) maps to ICD-10-CM code H74.8X9 (other disorder of middle ear and mastoid). A “retained foreign body in the middle ear” elicits a fairly straightforward clinical scenario, whereas “other disorder of middle ear and mastoid” could be any number of clinical issues and levels of acuity.
Coding inaccuracies could result in financial loss. The purpose of a diagnostic code is to determine medical necessity of a specific treatment or intervention. Theoretically, a clinician could select what he or she believes is a clinically correct code, but the insurance company uses a mapping to a different ICD-10-CM code, which could result in financial disruption due to billing errors. Such errors will likely occur harmlessly due to the complex nature of the transition to the new coding system. However, some errors may occur intentionally because a provider or insurance company could try to maximize gains by selectively mapping to certain ICD-10-CM codes. Furthermore, the misallocation of scarce resources (personnel, supplies, etc) due to inaccurate projections if coding data are incorrect could have financial and logistical implications for practices and health care systems.
More than 40% of visits were coded 999.99 and were excluded from our analysis because we could not categorize on the basis of the clinical definition of the code. The general nature of this diagnosis code limited our ability to evaluate the impact for pediatricians. We do not know what clinical encounters typically prompt the use of ICD-9-CM code 999.99, especially because the reimbursement appears to be quite low (∼$2).
Despite the potential for financial disruption, the transition to ICD-10-CM is likely to provide important benefits over time. The increased level of clinical detail embedded in each ICD-10-CM code, if coded appropriately, should improve the overall quality of billing data, leading to improvements in how we measure quality of care, reimburse providers, and use resources. Because there is less clinical ambiguity in ICD-10-CM codes, compared with ICD-9-CM, it should be easier to compare clinical documents with the codes billed for service and identify inconsistencies between a diagnosis and the care provided (procedures, studies, etc), decreasing opportunities for health care fraud.19 As pediatric providers and practices prepare for the transition to ICD-10-CM, awareness of the complexity of the transition process, as well as specific codes with potential pitfalls, will be important to maximize clinical accuracy of coding data and to minimize financial disruptions and administrative burdens.
We acknowledge that our categories will not be clinically relevant to all providers. The potential errors for each practice and pediatrician will depend on the types of codes frequently used for billing and for other administrative purposes (staffing, ordering supplies, quality assurance). The Illinois Medicaid database is not representative of all patient populations across the country or coding variations regionally. The data involved in the study reflect the requirements for Illinois Medicaid in the year 2010. Patient data sets from private insurers or other government data set could result in different diagnosis codes being used more frequently. The payment by Medicaid tends to be less than other insurers, so the total monetary impact may be more than estimated by this article. Finally, we acknowledge that our interpretation of the mappings could be influenced by personal and clinical experiences. Because of the vast number of health care providers, payers, technology vendors, and commercial mapping tools in the United States, there will be a lack of consensus regarding how to map the codes and how to interpret the mappings for years to come.
Conclusions
The potential for financial disruption and administrative errors from 39% of pediatric diagnosis codes (8% of Medicaid reimbursement) necessitates special attention to these codes in preparing for the transition to ICD-10-CM for pediatric practices. Many pediatric practices function on a thin financial margin in which 3% to 5% of codes resulting in billing errors could have a significant financial impact. Sufficient planning to mitigate this challenge and prepare is necessary.
Supplementary Material
Glossary
- CMS
Centers for Medicare and Medicaid Services
- GEM
General Equivalent Mapping
- ICD-9-CM
International Classification of Diseases, Ninth Revision, Clinical Modification
- ICD-10-CM
International Classification of Diseases, 10th Revision, Clinical Modification
Footnotes
Dr Caskey helped to conceptualize and design the study, participated in determining criteria for categorization of ICD-10-CM codes, categorized the ICD-10-CM codes, and drafted the initial manuscript; Mr Zaman performed initial analyses for the accuracy of the codes and the analysis of the financial data and reviewed and revised the manuscript; Drs Nam, Chae, Williams, and Mathew participated in determining criteria for categorization of ICD-10-CM codes, categorized the ICD-10-CM codes, and reviewed and revised the manuscript; Mr Burton queried the initial database of Medicaid, assisted in the characterization of the data and the analysis of the financial data, and reviewed and revised the manuscript; Mr Li carried out the initial analyses for the accuracy of the codes and the analysis of the financial data and reviewed and revised the manuscript; Dr Lussier helped to conceptualize and design the study; Dr Boyd helped to conceptualize and design the study, identified key collaborators, had access to all of the data throughout the study, and assisted in drafting the initial manuscript; and all authors approved the final manuscript as submitted.
FINANCIAL DISCLOSURE: The authors have indicated they do not have a financial relationship relevant to this article to disclose.
FUNDING: Drs Boyd and Lussier are supported in part by the Center for Clinical and Translational Sciences of the University of Illinois (NIH 1UL1RR029879-01, NIH/NCATS UL1TR000050), the Institute for Translational Health Informatics of the University of Illinois at Chicago, the Office of the Vice-President for Health Affairs of the University of Illinois Hospital and Health Sciences System, Department of Biomedical and Health Information Sciences, and the Department of Pediatrics.
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
COMPANION PAPER: A companion to this article can be found on page 169, and online at www.pediatrics.org/cgi/doi/10.1542/peds.2014-0726.
References
- 1.Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45(6):613–619 [DOI] [PubMed] [Google Scholar]
- 2.Dubberke ER, Butler AM, Yokoe DS, et al. Multicenter study of surveillance for hospital-onset clostridium difficile infection by the use of ICD-9-CM diagnosis codes. Infect Control Hosp Epidemiol. 2010;31(3):262–268 [DOI] [PMC free article] [PubMed]
- 3.Henderson T, Shepheard J, Sundararajan V. Quality of diagnosis and procedure coding in ICD-10 administrative data. Med Care. 2006;44(11):1011–1019 [DOI] [PubMed] [Google Scholar]
- 4.Hougland P, Nebeker J, Pickard S, et al. Using ICD-9-CM codes in hospital claims data to detect adverse events in patient safety surveillance. In: Henriksen K, Battles JB, Keyes MA, Grady ML, eds. Advances in Patient Safety: New Directions and Alternative Approaches. Vol. 1 Rockville, MD: Agency for Healthcare Research and Quality; 2008 [PubMed] [Google Scholar]
- 5.Centers for Medicare and Medicaid Services. Overview: ICD-10. Updated 2011. Available at: https://www.cms.gov/ICD10/. Accessed February 29, 2012
- 6.AAP Division of Health Care Finance and Quality Improvement. ICD-10-CM implementation delayed until 2013. AAP News 2009;30(4):31. Available at: http://aapnews.aappublications.org/content/30/4/31.1.short. Accessed November 26, 2013
- 7.Godedert J. AMA to Sebelius: Stop ICD-10. HealthData Management February 2, 2012 Availible at: www.healthdatamanagement.com/news/icd-10-hhs-sebelius-american-medical-association-43967-1.html. Accessed April 28, 2014
- 8.Sanders TB, Bowens FM, Pierce W, Stasher-Booker B, Thompson EQ, Jones WA. The road to ICD-10-CM/PCS implementation: forecasting the transition for providers, payers, and other healthcare organizations. Perspect Health Inf Manag. 2012;9:1f. [PMC free article] [PubMed] [Google Scholar]
- 9.Meyer H. Coding complexity: US health care gets ready for the coming of ICD-10. Health Aff (Millwood). 2011;30(5):968–974 [DOI] [PubMed]
- 10.Topaz M, Shafran-Topaz L, Bowles KH. ICD-9 to ICD-10: evolution, revolution, and current debates in the United States. Perspect Health Inf Manag. 2013;10:1d. [PMC free article] [PubMed] [Google Scholar]
- 11.Chute CG, Huff SM, Ferguson JA, Walker JM, Halamka JD. There are important reasons for delaying implementation of the new ICD-10 coding system. Health Aff (Millwood). 2012;31(4):836–842 [DOI] [PubMed]
- 12.Januel JM, Luthi JC, Quan H, et al. Improved accuracy of co-morbidity coding over time after the introduction of ICD-10 administrative data. BMC Health Serv Res. 2011;11:194 [DOI] [PMC free article] [PubMed]
- 13.Quan H, Eastwood C, Cunningham CT, et al. Validity of AHRQ patient safety indicators derived from ICD-10 hospital discharge abstract data (chart review study). BMJ Open. 2013;3(10):e003716 [DOI] [PMC free article] [PubMed]
- 14.Boyd AD, Li JJ, Burton MD, et al. The discriminatory cost of ICD-10-CM transition between clinical specialties: metrics, case study, and mitigating tools. J Am Med Inform Assoc. 2013;20(4):708–717 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.White RH, Sadeghi B, Tancredi DJ, et al. How valid is the ICD-9-CM based AHRQ patient safety indicator for postoperative venous thromboembolism? Med Care. 2009;47(12):1237–1243 [DOI] [PubMed] [Google Scholar]
- 16.Venepalli N.K, Qamruzzaman Y, Li J, Lussier YA, Boyd AD. Identifying clinically disruptive ICD-10-CM conversions to mitigate financial costs using an online tool. J Oncology Practice. February 11, 2014. doi:10.1200/JOP.2013.001156 [DOI] [PubMed] [Google Scholar]
- 17.American Medical Association. Crosswalking between ICD-9 and ICD-10. Preparing for the ICD-10 code set: October 1, 2014 compliance date. Fact Sheet 7. Updated 2012. Available at: www.ama-assn.org/resources/doc/washington/crosswalking-between-icd-9-and-icd-10.pdf. Accessed April 5, 2013
- 18.Boyd AD, Lussier YA. Mitigating tools for ICD-10-CM transition through convolution and entanglement. HIMSS14 Annual Conference and Exhibition; 2014, February 23-27; Orlando, FL, Educational Session 137. Available at: www.himssconference.org/Education/EventDetail.aspx?ItemNumber=25017. Accessed April 29, 2014
- 19.Centers for Disease Control and Prevention. ICD-10 update. Updated 2012. Available at: www.cdc.gov/nchs/icd/icd10cm.htm#10update. Accessed January 2012
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.