Abstract
The transradial approach for coronary catheterisation has gained rising popularity owing to its fewer access site complications compared with the transfemoral approach. A rare but recognisable complication of the procedure is radial artery pseudoaneurysm (PSA). We report a case of radial PSA occurring 2 h following percutaneous coronary intervention in an 85-year-old woman, which was successfully treated by ultrasound-guided thrombin injection. This non-surgical technique has recently gained rising popularity as a relatively novel modality of managing radial PSA.
Background
The occurrence of radial pseudoaneurysm (PSA) following transradial angiography is considered rare, with incidence figures ranging from 3 to 20:10 000 as evident from our literature search.1 2
Treatment options currently available include conventional surgical repair, ultrasound-guided compression repair (UGCR) and, more recently, ultrasound-guided thrombin injection (UGTI). We aim to report the success of the latter modality (UGTI) in the management of the single case of radial PSA that was diagnosed at our tertiary interventional cardiology facility to date.
Case presentation
An 85-year-old woman underwent successful percutaneous coronary intervention to her right coronary artery for stable angina. Her medical history included inferior myocardial infarction, hypertension and hypothyroidism. The procedure was performed via the right radial artery using a JR4 guide catheter. A TR compression band (Terumo, Japan) was placed on the radial artery postprocedure in order to attain haemostasis.
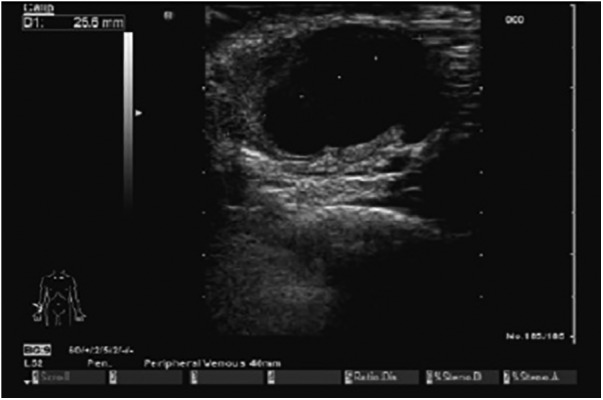
Two hours following the procedure, the patient developed a pulsatile swelling on the right radial aspect of her forearm, underlying the puncture site used for her procedure (figure 1). Given her recent intervention, the swelling was thought to be most likely due to a PSA of the right radial artery.
Figure 1.

Pseudoaneurysm formation after transradial puncture.
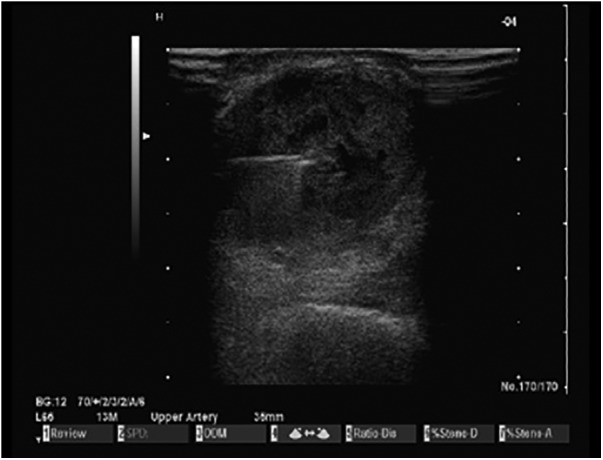
Duplex ultrasound scan confirmed the diagnosis, revealing a PSA measuring 2.5×2.3 cm (figure 2). A decision was made to manage the patient by thrombin injection of the aneurysmal sac under ultrasound guidance, due to its reportedly superior primary success rate in treating upper limb extremity PSA, as in recent case series.
Figure 2.
Doppler ultrasound of the right wrist was carried out, which confirmed the diagnosis of pseudoaneurysm of radial artery measuring 2.5×2.3 cm.
Investigations
An ultrasound scan of the patient's right radial artery revealing the PSA measuring 2.5×2.3 cm is demonstrated in figure 2.
Treatment
After confirmation of the diagnosis, the patient underwent injection of thrombin (1 mL) into the sac of the PSA under ultrasound guidance (figure 3). This resulted in immediate and complete thrombosis of the sac (figure 4), and the patient was discharged home the following day with arrangement of outpatient follow-up after a 6-week interval.
Figure 3.
Ultrasound-guided injection of 1 mL of thrombin via a 22G spinal needle.
Figure 4.

Immediate postinjection complete thrombosis on ultrasound imaging.
Outcome and follow-up
At a review in clinic at 6 weeks postdischarge, the patient's right radial artery PSA had healed well (figure 5), and the radial artery pulse was palpable. The patient gave an account of her ‘wrist swelling’ completely resolving approximately 2 weeks after her UGTI procedure.
Figure 5.
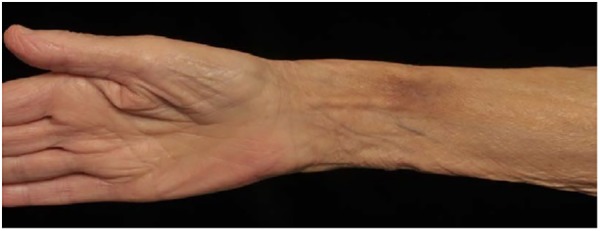
Picture taken 6 weeks following thrombin injection showing complete resolution of the pseudoaneurysm.
Discussion
Transradial angiography and angioplasty is a preferable route to the more traditional femoral approach and results in fewer vascular complications. In the RIVAL study, there was a significant reduction in large haematomas and PSA formation.1 3 There are many contributing factors for development of a PSA including antiplatelet and anticoagulant therapy, hypertension and inadequate compression of the puncture site postprocedure.4 5
Surgical repair of post-catheterisation PSA has become uncommon with the evolution of non-surgical minimally invasive techniques,4 6 and is primarily restricted to certain indications. These include UGCR and UGTI. The latter has become superior to UGCR in respect to success rate, time to achieve thrombosis and need for analgaesia.5 7–11
The primary success rate of UGTI therapy, when compared with UGCR, in PSA resolution is reported to range from 91% to 100%9–11 versus 63% to 98%,5 respectively.
Webber et al reported a primary success rate of UGTI ranging from 91% to 100% through their meta-analysis of a summary of 14 UGTI series (1329 PSA injections), with a cumulative success rate of 97%. However, these UGTI series assessed UGTI of lower limb PSAs and therefore results may not be generalised to all PSA sites.5
Two studies demonstrated an average time range for achieving thrombosis as being seconds with UGTI, compared to 33–37 min with UCGR.5 7
As with most interventions, the success of UGTI does not come without complications. Possible adverse events that may result include: deep venous thrombosis, pulmonary embolism and thrombosis of the injected artery. Allergic reactions and anaphylaxis may also occur, particularly in patients previously sensitised to bovine thrombin. Although rare, Webber et al5 concluded an overall complication rate of 1.3%, with a risk for embolism of 0.5%, in their meta-analysis referred to in the last paragraph.12
As evidenced by our literature search, there are a limited number of reports (n=24) on post-catheterisation radial artery PSA, which occasionally report it among other sites of PSA. An even fewer number of reports (n=7) focuses on the efficacy of UGTI therapy in radial artery PSA.2 13–16 These have all concluded similar evidence, that being UGTI is a feasible and effective treatment option, which usually results in rapid and complete occlusion of the PSA. Zegri et al2 claimed to report the largest case series to date of post-catheterisation radial artery PSA managed by non-surgical techniques. Their series consisted of five patients who developed radial artery PSA, who were all managed initially with prolonged direct mechanical compression, which failed in four patients (80%). Two patients were then managed by thrombin injection (1 mL, 500 IU), which was successful in both patients.
It is important to note UGTI therapy remains unlicensed and may lead to potentially serious complications, despite their rare occurrence. There remains a discrepancy on the standardised dose of thrombin required to achieve successful thrombosis of the aneurysmal sac.
Learning points.
The occurrence of a pseudoaneurysm (PSA) post-transradial angiography is a rare yet potentially serious complication.
Non-surgical methods (ultrasound-guided compression repair, UGCR and ultrasound-guided thrombin injection, UGTI) should be considered in the treatment of post-catheterisation PSA, however, it is imperative to recognise their contraindications and complications.
UGTI has a significantly higher success rate in resolution of PSA when compared to UGCR, and requires notably less time to perform.
Although UGTI is a safe and effective treatment modality for achieving successful thrombosis of radial PSA, thrombin remains unlicensed for this use and, therefore, use must be directed by an experienced clinician.
Footnotes
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Jolly S, Yusuf S, Cairns J et al. Radial versus femoral access for coronary angiography and intervention in patients with acute coronary syndromes (RIVAL): a randomised, parallel group, multicentre trial. Lancet 2011;377:1409–20. 10.1016/S0140-6736(11)60404-2 [DOI] [PubMed] [Google Scholar]
- 2.Zegri I, Garicia-Touchard A, Cuenca S et al. Radial artery pseudoaneurysm after cardiac catheterisation: peculiarities and non-surgical treatment results. Rev Esp Cardiol 2015;68:349–51. 10.1016/j.recesp.2014.11.018 [DOI] [PubMed] [Google Scholar]
- 3.Kanei Y, Kwan T, Nakra NC et al. Transradial cardiac catheterization: a review of access site complications. Catheter Cardiovasc Interv 2011;78:840–6. 10.1002/ccd.22978 [DOI] [PubMed] [Google Scholar]
- 4.Morgan R, Belli AM. Current treatment methods for postcatheterization pseudoaneurysms. J Vasc Interv Radiol 2003;14:697–710. 10.1097/01.RVI.0000071089.76348.6A [DOI] [PubMed] [Google Scholar]
- 5.Webber G, Jang J, Gustavson S et al. Contemporary management of postcatheterization pseudoaneurysms. Circulation 2007;115:2666–74. 10.1161/CIRCULATIONAHA.106.681973 [DOI] [PubMed] [Google Scholar]
- 6.Bhat T, Teli S, Bhat H et al. Access-site complications and their management during transradial cardiac catheterization. Exp Rev Cardiovasc Ther 2012;10:627–34. 10.1586/erc.12.16 [DOI] [PubMed] [Google Scholar]
- 7.Taylor BS, Rhee RY, Muluk S et al. Thrombin injection versus compression of femoral artery pseudoaneurysms. J Vasc Surg 1999;30:1052–9. 10.1016/S0741-5214(99)70043-1 [DOI] [PubMed] [Google Scholar]
- 8.Kang SS, Labropoulos N, Mansour MA et al. Expanded indications for ultrasound-guided thrombin injection of pseudoaneurysms. J Vasc Surg 2000;31:289–98. 10.1016/S0741-5214(00)90160-5 [DOI] [PubMed] [Google Scholar]
- 9.Krueger K, Zaehringer M, Strohe D et al. Postcatheterization pseudoaneurysm: results of US-guided percutaneous thrombin injection in 240 patients. Radiology 2005;236:1104–10. 10.1148/radiol.2363040736 [DOI] [PubMed] [Google Scholar]
- 10.Sheiman R, Mastromatteo M. Iatrogenic femoral pseudoaneurysms that are unresponsive to percutaneous thrombin injection: potential causes. AJR Am J Roentgenol 2003;181:1301–4. 10.2214/ajr.181.5.1811301 [DOI] [PubMed] [Google Scholar]
- 11.La Perna L, Olin JW, Goines D et al. Ultrasound-guided thrombin injection for the treatment of postcatheterization pseudoaneurysms. Circulation 2000;102:2391–5. 10.1161/01.CIR.102.19.2391 [DOI] [PubMed] [Google Scholar]
- 12.Teh LG, Sieunarine K. Thrombin injection for repair of pseudoaneurysms: a case for caution. Australas Radiol 2003;47:64–6. 10.1046/j.1440-1673.2003.01106.x [DOI] [PubMed] [Google Scholar]
- 13.Komorowska-Timek E, Teruya TH, Abou-Zamzam AM Jr et al. Treatment of radial and ulnar artery pseudoaneurysms using percutaneous thrombin injection. J Hand Surg (USA) 2004;29:936–42. 10.1016/j.jhsa.2004.05.009 [DOI] [PubMed] [Google Scholar]
- 14.Herold J, Brucks S, Boenigk H et al. Ultrasound guided thrombin injection of pseudoaneurysm of the radial artery after percutaneous coronary intervention. Vasa J Vasc Dis 2011;40:78–81. [DOI] [PubMed] [Google Scholar]
- 15.Collins N, Wainstein R, Ward M et al. Pseudoaneurysm after transradial cardiac catheterization: case series and review of the literature. Catheter Cardiovasc Interv 2012;80:283–7. 10.1002/ccd.23216 [DOI] [PubMed] [Google Scholar]
- 16.Pozniak MA, Mitchell C, Ledwidge M. Radial artery pseudoaneurysm: a maneuver to decrease the risk of thrombin therapy. J Ultrasound Med 2005;24:119–22. [DOI] [PubMed] [Google Scholar]


