Abstract
Objectives:
To assess the prevalence of concomitant use of two or more antipsychotic drugs and other psychotropic drugs in the Swedish population.
Methods:
Data for this observational cohort study were collected from the Swedish Prescribed Drug Register including all dispensed drugs to the entire Swedish population (9.4 million inhabitants). We identified all individuals with at least one dispensed prescription of antipsychotic drug during January to June 2008. After 12 months, a second exposure period was chosen. Individuals who were dispensed two or more antipsychotic drugs in both periods were considered long-time users of antipsychotic polypharmacy.
Results:
In 2008, 1.5% of the Swedish population was dispensed antipsychotic drugs, the majority (75%) using only one antipsychotic drug. Out of individuals who were dispensed 2 or more antipsychotic drugs during the first period, 62% also was also dispensed at least 2 antipsychotic drugs during the second period. A total of 665 different unique combinations were used in 2008. Individuals prescribed two or more antipsychotic drugs during both periods were more often dispensed anxiolytics and sedatives than those who were dispensed only one antipsychotic drug. Elderly were dispensed antipsychotic drugs much more often than younger persons.
Conclusions:
In Sweden, 25% of patients dispensed antipsychotic drugs receive a combination of two or more antipsychotic drugs. Individuals who are dispensed antipsychotic polypharmacy are more often dispensed anxiolytics and sedatives than those prescribed only one antipsychotic drug. Long-term observational studies are needed to assess the efficacy and safety of such combinations.
Keywords: antipsychotic agents, drug polytherapy, drug utilization, polypharmacy, psychotic disorders, schizophrenia
Introduction
Most psychiatrists come across patients with a combination of prescription drugs that challenge all guidelines and scientific evidence. Since 50 years, antipsychotic drugs are the pharmacological treatment of choice for most patients with schizophrenia and other psychotic disorders. The vast majority of clinical trials are made with monotherapy. Due to the severity of schizophrenia, many patients do not recover with one antipsychotic drug and, consequently, it is common practice to try different combinations of drugs. There are, however, few studies analyzing the benefit or risk of combination treatment with ⩾2 antipsychotic drugs [Schumacher et al. 2003; Tapp et al. 2003; Ganguly et al. 2004; Broekema et al. 2007; Kreyenbuhl et al. 2007a, 2007b; Megna et al. 2007; Lee and Walker, 2008; Pandurangi and Dalkilic, 2008; Tranulis et al. 2008]. Since antipsychotic drugs may cause severe side effects such as cognitive and emotional blunting, acute and chronic extrapyramidal side effects, torsade de pointes, weight gain and metabolic syndrome [Jeste and Caligiuri, 1993; Raschi et al. 2013], these drugs should be used with utmost care and only when really needed. Despite severe side effects and high treatment costs and the lack of evidence, there is a widespread use of antipsychotic drugs as sedatives–hypnotics even in the absence of a psychotic or bipolar disorder [Schmidt and Fastborn, 2000]. Several of the newest generation antipsychotic agents are also used as long-term mood stabilizers, either alone or in combination with lithium, and as treatment for manic episodes [Sanches et al. 2010; De Fazio et al. 2010]. An agitated in-patient may be prescribed several psychotropic drugs by different doctors resulting in strange combinations. The regular physician may miss that on-call doctors have added new drugs. It is always hard to assess the effect of a specific drug in patients receiving many different drugs.
Many elderly patients with dementia are prescribed antipsychotic drugs rather as an unspecific sedative than as an antipsychotic agent. Elderly are particularly sensitive to antipsychotic drugs, and get more severe acute and chronic extrapyramidal side effects [Jeste, 2000]. The positive effect is questionable and mortality increases [US Food and Drug Adminisation, 2008], although it has recently been proposed that it is the severity of the disease rather than the antipsychotic drug that causes the increased mortality in Alzheimer patients receiving antipsychotic drugs [Lopez et al. 2013].
The establishment of the Swedish Prescribed Drug Register in 2005 created new opportunities for studies of polypharmacy [Haider et al. 2009; Lesen et al. 2009; Wettermark et al. 2007]. This register includes all dispensed drugs to the entire Swedish population (9.4 million inhabitants). Each year approximately 90 million prescriptions are recorded for more than 6 million individuals (two-thirds of the Swedish population use prescription drugs). Consequently, the register represents one of the largest population-based pharmacoepidemiological databases in the world.
The aim of this study was to assess the prevalence of the simultaneous use of two or more antipsychotic drugs in the Swedish population.
Material and methods
This was an observational cohort study based on data on dispensed prescriptions of antipsychotic drugs to the entire Swedish population collected from the Swedish Prescribed Drug Register [Wettermark et al. 2007]. The register contains patient identity data on substance, brand name, formulation and package as well as date of prescribing and dispensing. All drugs are classified according to the Anatomical Therapeutic Chemical (ATC) classification system. The register is managed by the National Board of Health and Welfare. Over-the-counter (OTC) medications and drugs used in hospitals are not included. Most nursing home patients get their drugs dispensed on prescriptions or multidose dispensing, and are thus included in the register. Antipsychotic drugs (ATC N05A) except lithium registered in Sweden in 2008 are listed in Table 1 along with the number of dispensed defined daily doses (DDDs). Some nonregistered antipsychotic drugs prescribed on special permission from the regulatory agency were also included.
Table 1.
Antipsychotic drugs dispensed in ambulatory care in Sweden during 2008.
| ATC code and substance name | No. of DDDs | ATC code and substance name | No. of DDDs |
|---|---|---|---|
| N05AH03 Olanzapin | 6,461,443 | N05AD03 Melperon | 123,364 |
| N05AN01 Litium | 5,323,841 | N05AF03 Klorprotixen | 116,236 |
| N05AX08 Risperidon | 3,709,272 | N05AB01 Dixyrazin | 36,876 |
| N05AF05 Zuklopentixol | 2,074,121 | N05AC02 Tioridazin | 36,558 |
| N05AD01 Haloperidol | 1,841,969 | N05AG02 Pimozid | 35,842 |
| N05AH04 Quetiapin | 1,800,467 | N05AB04 Proklorperazin | 29,036 |
| N05AH02 Klozapin | 1,783,062 | N05AA01 Klorpromazin | 15,926 |
| N05AB03 Perfenazin | 1,491,791 | N05AE03 Sertindol | 9492 |
| N05AX12 Aripiprazol | 1,270,095 | N05AX13 Paliperidon | 8820 |
| N05AF01 Flupentixol | 755,546 | N05AL01 Sulpirid | 6685 |
| N05AA02 Levomepromazin | 696,561 | N05AL03 Tiaprid | 1048 |
| N05AE04 Ziprasidon | 636,867 | N05AC01 Periciazin | 938 |
| N05AB02 Flufenazin | 213,000 | N05AD05 Pipamperon | 116 |
ATC, Anatomical Therapeutic Chemical; DDD, defined daily dose.
The period prevalence of antipsychotic drug use was assessed as the proportion of subjects in the Swedish population that were dispensed antipsychotic drugs during 2008 and 2009, respectively. Due to its unique position as a mood stabilizer in bipolar disorders and lack of evidence for treatment of schizophrenia, lithium was excluded from the analysis. All antipsychotic drugs except lithium are referred to as APD in this paper.
The incidence of new APD users was assessed by identifying individuals purchasing an antipsychotic drug for the first time after a 1 year run-in period without any dispensed antipsychotic drugs. To investigate the long-term use of multiple antipsychotic drugs, we identified all persons with at least 1 dispensed prescription APD during a period of 6 months (January to June 2008, exposure window 1). Among these we identified individuals purchasing ⩾2 APDs during the period. To minimize the number of patients on cross-titration, a second exposure window was chosen after a period of 12 months (January to June 2009, exposure window 2). Patients who were still dispensed ⩾2 APDs were identified and considered long-time users of antipsychotic polypharmacotherapy [Fincke et al. 2005]. The length of the windows (6 months) and the antipsychotic free run-in period (1 year) to determine incidence were selected because the Swedish reimbursement system allows patients to be dispensed drugs for a period of 3 months at the time to receive full reimbursement. For long-term users of ⩾2 APDs, concomitant dispensing of adjuvant psychotropic medication was also studied for opiates (N02A), anxiolytics (N05B), sedatives (N05C), antidepressants (N06A) and antidementia drugs (N06D). Patients who died during the observation period were identified using the Swedish cause-of-death register [Furu et al. 2010].
Ethical considerations
All analyses were undertaken by the Swedish National Board of Health and Welfare, which is a government agency that, in accordance with Swedish law, can use population-based registers to follow and analyse health and social conditions among the general population. All data were made anonymous for the research team with no possibility to identify any individual patient.
Results
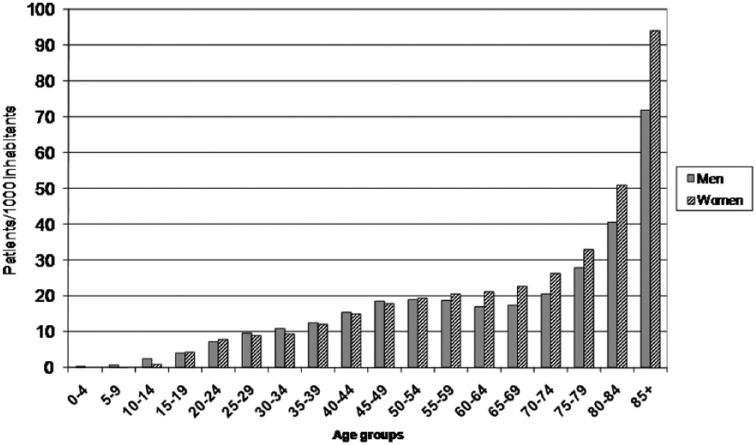
In 2008, 132,000 persons, corresponding to 1.5% of the Swedish population were dispensed APDs. In addition, 11,000 persons were dispensed lithium. Figure 1 shows the number of patients dispensed APDs per 1000 inhabitants in Sweden during 2008 split by age and sex. The utilization of antipsychotic drugs was scarce among children and increased from puberty to about 45 years of age. Then it remained stable until about 65 years of age, but tripled in the group aged 85 years and older. Men used antipsychotic drugs more often than women until about 50 years of age. Thereafter women used more antipsychotic drugs than men (Figure 1).
Figure 1.
Utilization of antipsychotic drugs in Sweden during 2008 by age and sex.
During the year, a total of 34,100 patients were initiated on APD treatment. This corresponds to an incidence rate of 3.7/1000 person-years. For persons aged 75+, the incidence was 15.6/1000 person-years. The overall use of APDs in Sweden decreased by 3% in 2009 compared with 2008. The decrease was most pronounced among patients over 80 years of age (18%). Correspondingly, in 2009 the incidence rate had decreased to 3.5/1000 person- years. For persons aged 75+, the incidence decreased by 18% to 12.7/1000 person-years.
The total number of individuals purchasing at least one APD during both exposure windows was 80,576 (44,074 females and 36,502 males). Among these, 60,597 individuals (75%) were dispensed only one APD during both exposure windows.
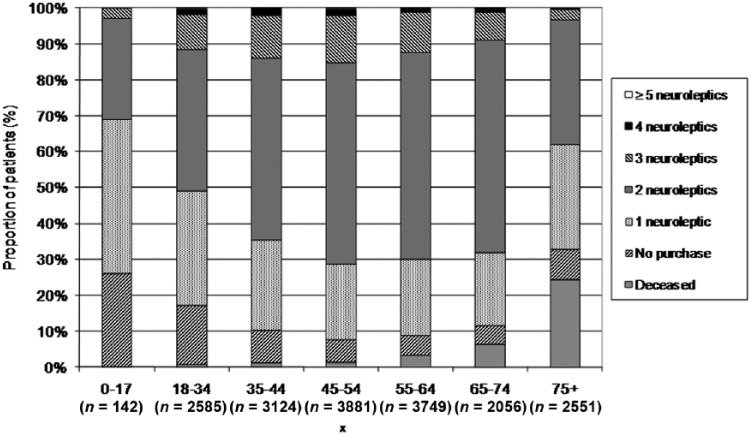
Of the 18,088 individuals who were dispensed ⩾2 APDs during exposure window 1, 988 (5%) died before exposure window 2. In addition, 1513 persons (8%) did not purchase any APDs during the second period. A total of 11,142 (62%) were dispensed at least 2 APDs during both windows (Table 1, Figure 2). In the youngest group (0–17 years of age), about 25% were not dispensed any APDs during the second period and about 45% were dispensed a single APD. In those aged 18–34, about 17% were not dispensed any APD, but 30% were dispensed 1 APD and 40% two APDs. In the group aged 45–74, about 50% were dispensed 2 APDs and 70 ⩾2 APDs.
Figure 2.
Individuals dispensed two or more antipsychotic drugs during January to June 2008, and the number of antipsychotic drugs they were dispensed during January to June 2009, by age groups.
Different combinations of substances
Of the 8370 individuals who were dispensed 2 APDs during both time windows, 800 were dispensed the same combination during both periods whereas 7570 had a different combination. For the individuals with combinations of 3 APDs, 132 of 1022 had the same combination during both periods. Among individuals who were dispensed 4 APDs during both time windows, 13 of 85 had the same combination of drugs. The individuals who were dispensed ⩾5 APDs are not reported due to small numbers (Table 2).
Table 2.
Individuals dispensed two or more antipsychotic drugs during January to June 2008, and the number of antipsychotic drugs they were dispensed during January to June 2009.
| No. of substances in 2008 | Deceased ⩽30 June 2009 | 2009 |
|||||
|---|---|---|---|---|---|---|---|
| No purchase | 1 substance | 2 substances | 3 substances | 4 substances | ⩾5 substances | ||
| 2 (n = 15,339) | 882 (5.8%) | 1337 (8.7%) | 3984 (26.0%) | 8370 (54.6%) | 705 (4.6%) | 57 (0.4%) | 4 (<0.1%) |
| 3 (n = 2404) | 97 (4.0%) | 156 (6.5%) | 410 (17.1%) | 620 (25.8%) | 1022 (42.5%) | 90 (3.7%) | 9 (0.4%) |
| 4 (n = 313) | 9 (2.9%) | 19 (6.1%) | 43 (13.7%) | 82 (26.2%) | 69 (22.0%) | 85 (27.2%) | 6 (1.9%) |
| ⩾5 (n = 32) | 0 | 1 (<0.1%) | 8 (25.0%) | 5 (15.6%) | 6 (18.8%) | 4 (12.5%) | 8 (25.0%) |
| Total (n = 18,088) | 988 | 1513 | 4445 | 9077 | 1802 | 236 | 27 |
A total of 665 different unique substance combinations were used in 2008. The most commonly dispensed combination was levomepromazine + risperidone (Table 3).
Table 3.
Most commonly dispensed combinations of antipsychotic drugs N05A January to June 2008. *
| Combination of two substances | n | Combination of three substances | n |
|---|---|---|---|
| levomepromazine + risperidone | 1119 | Levomepromazin + zuklopentixol + olanzapin | 118 |
| levomepromazine + olanzapine | 961 | Levomepromazin + haloperidol + olanzapine | 106 |
| olanzapine + risperidone | 788 | Levomepromazin + perphenazine + olanzapine | 84 |
| levomepromazine + haloperidol | 780 | Levomepromazin + olanzapin + risperidone | 83 |
| haloperidol + risperidone | 656 | Levomepromazin + zuklopentixol + risperidone | 68 |
Lithium is excluded.
Concomitant use of other psychotropic drugs
Out of the 11,142 individuals with ⩾2 APDs both during the first and the second time window, a total of 5058 (45%) were dispensed anxiolytics (N05B), 5468 (49%) were dispensed sedatives (N05C), 4683 (42%) were dispensed antidepressants (N06A), 1060 (10%) were dispensed opiates (N02A) and 78 (1%) were dispensed antidementia drugs during the second time window. The corresponding figures for the 60,597 patients only purchasing 1 APD in both periods were 35% (anxiolytics), 40% (sedatives), 47% (antidepressants), 15% (opiates) and 4% (antidementia drugs), respectively.
Discussion
To our surprise, there were a total of 665 unique combinations of APDs. However, the majority of patients (75%) were dispensed only 1 APD. Among those who were prescribed >1 APD at baseline, only about 10% had the same combination of APDs the next year. Since many patients with schizophrenia and other psychoses do not recover in spite of following guidelines, it is reasonable to try other treatment strategies under careful observation of the patients. Without clinical data, we had no possibility of judging if concomitant use of more than one APD was good or bad for the individual patient. In addition, those taking two APD during both periods were more often taking anxiolytics and sedatives than those taking only one APD. It is a fair guess that those patients are very sick and difficult to treat from many points of view. On the contrary, individuals taking one APD were more often taking opiates, suggesting that some patients in palliative care were included in this group. Combinations of an APD and opioids are partly used for the relief of pain and nausea.
Levomepromazine has been available in Sweden since 1959 and has strong anticholinergic and sedative properties. It was present in the two most common combinations of two antipsychotics, and in the three most common combinations of three antipsychotics. It is likely that levomepromazine is used widely for sleep and sedation due to its sedative properties.
Schizophrenia usually starts during teens and early adulthood, and strikes men more severely than women [Hafner, 2003]. There is a second peak of onset for women about the time of menopause. Our finding of a slightly higher consumption of APD in men until about 50 years of age and higher in women thereafter is in accordance with this. The use of APDs was highest among the oldest patients, although schizophrenia is rare in this group due to increased mortality. Psychotic symptoms do occur in the elderly due to delirium, degenerative changes in the brain, dementia or as a part of depression. If an elderly person presents with psychotics symptom, a careful workup should be started to determine the underlying cause. APDs should be used with great caution in the elderly, which is not always the case. In nursing homes, the access to doctors is limited and APDs may be used as sedatives, also in the absence of a proper indication. The elderly are more sensitive to extrapyramidal and anticholinergic effects than young people, and have more somatic disorders and thus more other drugs.
In 2005, there were international alarm reports about the increased risk for death for patients with dementia using modern generation anti-psychotics (US Food and Drug Adminstration, 2008).
The Swedish drug regulatory agency, the Medical Products Agency, which released its guidelines on Behavioural and Psychological Problems in Dementia (BPSD) in October 2008, strongly recommended other treatment strategies than drugs for this group. We believe that the new guidelines may have contributed to the decrease in the use of APDs for this group in Sweden.
In our study, mortality actually decreased with the number of APDs dispensed at baseline, contrary to what one would expect. The reason for this is unknown, but it may well be that this group of patients with extensive pharmacological APD treatment is carefully monitored by the healthcare profession. Alternatively, a combination therapy may actually be beneficial.
This study was based on the Swedish Prescribed Drug Register, which is one of the largest population-based databases in the world. We used data on dispensed drugs to determine concomitant use. To asses polypharmacy using registers is a challenge since we only have information on dispensed drugs and not on the actual use of these drugs. However, the agreement between dispensed prescriptions and self-reported data in a cohort of elderly residents in Finland was shown to be almost perfect or substantial for all antipsychotic drugs. The authors emphasized the need to select a time window in the register with caution since the sensitivity decreased with shorter time periods [Haukka et al. 2007; Rikala et al. 2010].
It is also important to recognize that there are certain limitations concerning the methodology. There is no gold standard on how to study polypharmacy in registers. We used a modified version of the method proposed by Fincke and colleagues [Fincke et al. 2005]. The reason for using a 12 month gap instead of a 6 month gap was an attempt to control for cross-titration at the beginning of therapy and to assess long-term use of ⩾2 APDs. We have no information on diagnosis for the individuals in this study and a previous report estimated that approximately 25% of antipsychotics were prescribed to individuals without psychotic disease [SBU, 1997] .
Despite the limitations, this study covering the total APDs dispensed in Sweden has clarified the extent of concomitant use of more than one APD. There is no way to assess the efficacy and safety of all those combinations in randomized clinical trials. Researchers must consider other ways of doing systematic research on this patient group, such as postmarketing surveillance studying using observational data from healthcare quality registers. This has proven helpful for other categories of patients and drugs [Askling et al. 2006; Kobelt et al. 2008]. A second opinion and re-evaluation of diagnosis, social situation and compliance, medication review by a clinical pharmacologist, a survey of nonprescription drugs that may interfere with APDs, pharmacogenetic assessment and blood level analysis of drugs should be offered systematically to therapy-resistant patients. This can be implemented by educational activities for physicians by, for example, the local Drug Therapeutic Committee that has the competence and network for this.
Footnotes
Funding: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Conflict of interest statement: The authors declare no conflicts of interest in preparing this article.
Contributor Information
Annica Bergendal, Division of Clinical Pharmacology, Department of Laboratory Medicine, Karolinska Institute at Karolinska University Hospital, Huddinge, C1:68, SE-141 86 Stockholm, Sweden.
Helena Schiöler, National Board of Health and Welfare, SE-106 30 Stockholm, Sweden.
Björn Wettermark, Division of Clinical Pharmacology, Department of Laboratory Medicine, Karolinska Institutet at Karolinska University Hospital Huddinge, C1:68, SE-141 86 Stockholm Sweden and Stockholm County Council, Box 6909, SE-102 39 Stockholm, Sweden.
Karin Sparring Björkstén, Department of Neurobiology, Care sciences and Society, Karolinska Institutet, SLSO, Psykiatri Södra Stockholm, Box 5040, SE-121 05 Johanneshov, Sweden.
References
- Askling J., Fored C., Geborek P., Jacobsson L., van Vollenhoven R., Feltelius N., et al. (2006) Swedish registers to examine drug safety and clinical issues in RA. Ann Rheum Dis 65: 707–712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Broekema W., de Groot I., van Harten P. (2007) Simultaneous prescribing of atypical antipsychotics, conventional antipsychotics and anticholinergics – a European study. Pharm World Sci 29: 126–130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Fazio P., Girardi P., Maina G., Mauri M., Mauri M., Monteleone P., et al. (2010) Aripiprazole in acute mania and long-term treatment of bipolar disorder: a critical review by an Italian working group. Clin Drug Investig 30: 827–841. [DOI] [PubMed] [Google Scholar]
- Fincke B., Snyder K., Cantillon C., Gaehde S., Standring P., Fiore L., et al. (2005) Three complementary definitions of polypharmacy: methods, application and comparison of findings in a large prescription database. Pharmacoepidemiol Drug Saf 14: 121–128. [DOI] [PubMed] [Google Scholar]
- Furu K., Wettermark B., Andersen M., Martikainen J., Almarsdottir A., Sørensen H., et al. (2010) The Nordic countries as a cohort for pharmacoepidemiological research. Basic Clin Pharmacol Toxicol 106: 86–94. [DOI] [PubMed] [Google Scholar]
- Ganguly R., Kotzan J., Miller L., Kennedy K., Martin B. (2004) Prevalence, trends, and factors associated with antipsychotic polypharmacy among Medicaid-eligible schizophrenia patients, 1998–2000. J Clin Psychiatry 65: 1377–1388. [DOI] [PubMed] [Google Scholar]
- Hafner H. (2003) Gender differences in schizophrenia. Psychoneuroendocrinology 28(Suppl. 2): 17–54. [DOI] [PubMed] [Google Scholar]
- Haider S., Johnell K., Weitoft G., Thorslund M., Fastbom J. (2009) The influence of educational level on polypharmacy and inappropriate drug use: a register-based study of more than 600,000 older people. J Am Geriatr Soc 57: 62–69. [DOI] [PubMed] [Google Scholar]
- Haukka J., Suvisaari J., Tuulio-Henriksson A., Lönnqvist J. (2007) High concordance between self-reported medication and official prescription database information. Eur J Clin Pharmacol 63: 1069–1074. [DOI] [PubMed] [Google Scholar]
- Jeste D. (2000) Tardive dyskinesia in older patients. J Clin Psychiatry 61(Suppl. 4): 27–32. [PubMed] [Google Scholar]
- Jeste D., Caligiuri M. (1993) Tardive dyskinesia. Schizophr Bull 19: 303–315. [DOI] [PubMed] [Google Scholar]
- Kobelt G., Berg J., Lindgren P., Jonsson B., Stawiarz L., Hillert J. (2008) Modeling the cost-effectiveness of a new treatment for MS (natalizumab) compared with current standard practice in Sweden. Mult Scler 14: 679–690. [DOI] [PubMed] [Google Scholar]
- Kreyenbuhl J., Marcus S., West J., Wilk J., Olfson M. (2007a) Adding or switching antipsychotic medications in treatment-refractory schizophrenia. Psychiatr Serv 58: 983–990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kreyenbuhl J., Valenstein M., McCarthy J., Ganoczy D., Blow F. (2007b) Long-term antipsychotic polypharmacy in the VA health system: patient characteristics and treatment patterns. Psychiatr Serv 58: 489–495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee B., Walker V. (2008) Polypharmacy as the initial second-generation antipsychotic treatment. Psychiatr Serv 59: 717. [DOI] [PubMed] [Google Scholar]
- Lesen E., Petzold M., Andersson K., Carlsten A. (2009) To what extent does the indicator ‘concurrent use of three or more psychotropic drugs’ capture use of potentially inappropriate psychotropics among the elderly? Eur J Clin Pharmacol 65: 635–642. [DOI] [PubMed] [Google Scholar]
- Lopez O., Becker J., Chang Y., Sweet R., Aizenstein H., Snitz B., et al. (2013) The long-term effects of conventional and atypical antipsychotics in patients with probable Alzheimer’s disease. Am J Psychiatry 170:1051–1058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Megna J., Kunwar A., Mahlotra K., Sauro M., Devitt P., Rashid A. (2007) A study of polypharmacy with second generation antipsychotics in patients with severe and persistent mental illness. J Psychiatr Pract 13: 129–137. [DOI] [PubMed] [Google Scholar]
- Pandurangi A., Dalkilic A. (2008) Polypharmacy with second-generation antipsychotics: a review of evidence. J Psychiatr Pract 14: 345–367. [DOI] [PubMed] [Google Scholar]
- Raschi E., Poluzzi E., Godman B., Koci A., Moretti U., Kalaba M., et al. (2013) Torsadogenic risk of antipsychotics: combining adverse event reports with drug utilization data across Europe. PLoS One 8: e81208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rikala M., Hartikainen S., Sulkava R., Korhonen M. (2010) Validity of the Finnish Prescription Register for measuring psychotropic drug exposure among elderly finns: a population-based intervention study. Drugs Aging 27: 337–349. [DOI] [PubMed] [Google Scholar]
- Sanches M., Newberg A., Soares J. (2010) Emerging drugs for bipolar disorder. Expert Opin Emerg Drugs 15: 453–466. [DOI] [PubMed] [Google Scholar]
- SBU (1997) Behandling med neuroleptika. Stockholm: Statens beredning för medicinsk utvärdering (SBU) Available at: http://www.sbu.se/sv/Publicerat/Gul/Behandling-med-neuroleptika/(accessed 13 November 2014). [Google Scholar]
- Schmidt I., Fastborn J. (2000) Quality of drug use in Swedish nursing homes. Clin Drug Invest 20: 433–446. [Google Scholar]
- Schumacher J., Makela E., Griffin H. (2003) Multiple antipsychotic medication prescribing patterns. Ann Pharmacother 37: 951–955. [DOI] [PubMed] [Google Scholar]
- Tapp A., Wood A., Secrest L., Erdmann J., Cubberley L., Kilzieh N., et al. (2003) Combination antipsychotic therapy in clinical practice. Psychiatr Serv 54: 55–59. [DOI] [PubMed] [Google Scholar]
- Tranulis C., Skalli L., Lalonde P., Nicole L., Stip E. (2008) Benefits and risks of antipsychotic polypharmacy: an evidence-based review of the literature. Drug Saf 31: 7–20. [DOI] [PubMed] [Google Scholar]
- US Food and Drug Administration (2008) FDA Alert (6/16/2008) Information on conventional antipsychotics. Rockville, MD: US Food and Drug Administration; Available at: http://www.fda.gov/Drugs/DrugSafety/PostmarketDrugSafetyInformationforPatientsandProviders/ucm107211.htm. 2008. (accessed 13 November 2014). [Google Scholar]
- Wettermark B., Hammar N., Fored C., Leimanis A., Otterblad Olausson P., Bergman U., et al. (2007) The new Swedish Prescribed Drug Register – opportunities for pharmacoepidemiological research and experience from the first six months. Pharmacoepidemiol Drug Saf 16: 726–735. [DOI] [PubMed] [Google Scholar]