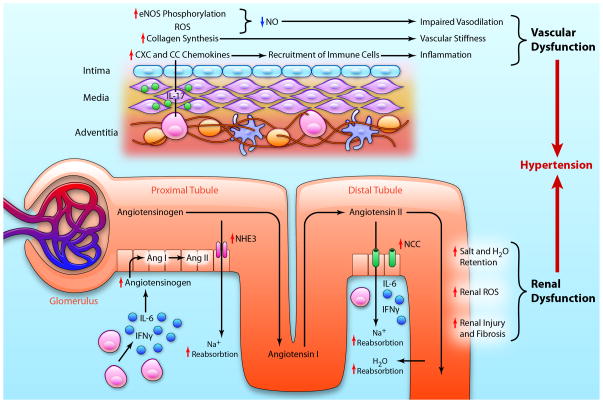
Figure 3.
Cytokines and end-organ dysfunction in hypertension. A) In vessels T cells infiltrate the adventitia and perivascular fat through the vasa vasorum. T cell-derived IL-17A acts on smooth muscle cells and adventitial fibroblasts to increase eNOS phosphorylation, reactive oxygen species (ROS) production, collagen synthesis, and chemokine production leading to a decrease in bioavailable nitric oxide (NO) and impaired vasodilation, increased vascular stiffness, and increased recruitment of immune cells, propagating the inflammatory response. These effects result in vascular dysfunction. B) In the renal medulla and cortex, activated T cells produce cytokines such as IL-6 and IFNγ that stimulate production of angiotensinogen. Angiotensinogen is converted to angiotensin I (Ang I) by intrarenal renin and subsequently to angiotensin II (Ang II) by intrarenal angiotensin converting enzyme. Angiotensin II upregulates and stimulates transport channels in the proximal and distal convoluted tubules including the sodium hydrogen exchanger 3 (NHE3) and sodium chloride co-transporter (NCC). In conjunction with salt and water retention, T cell activation causes an increase in renal ROS production, and renal injury and fibrosis, all of which lead to renal dysfunction. The culmination of vascular and renal dysfunction caused by T cell derived cytokines exacerbates hypertension. (Illustration credit: Ben Smith).