Figure 1. CT of the Chest Performed in Three Patients with Pneumonitis Associated with the Use of Anti– Programmed Cell Death 1 Antibodies.
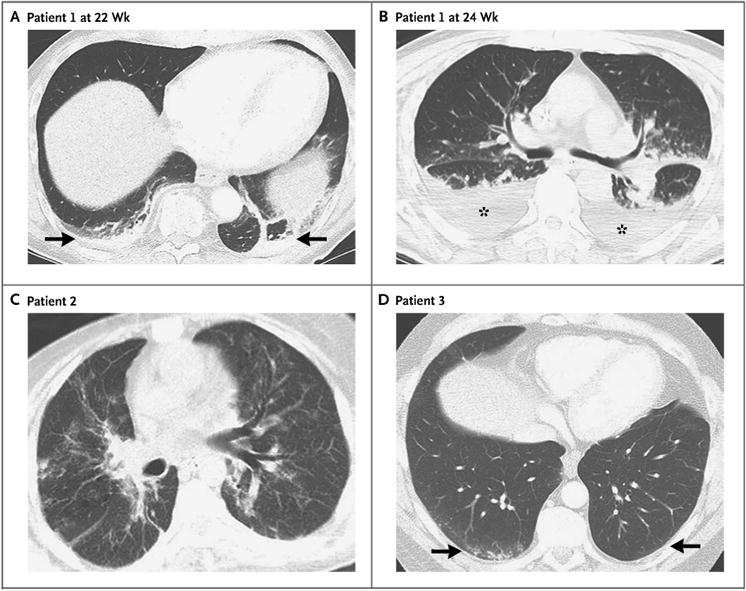
In Patient 1, a 70-year-old man with advanced melanoma who was treated in a trial of nivolumab given sequentially with ipilimumab, chest CT at 22 weeks of therapy revealed consolidation in the bilateral lower lobes with reticular and ground-glass opacities (Panel A, arrows). Two weeks later, the findings significantly progressed (Panel B, asterisks) and involved all lobes, with decreased lung volumes and pleural effusion. In Patient 2, a 38-year-old woman with advanced melanoma who was treated with nivolumab, chest CT at 15 weeks of therapy revealed diffuse ground-glass opacities, reticular opacities, consolidations, traction bronchiectasis, and areas of centrilobular nodularity (Panel C) involving all lobes and more than 50% of all lung zones, with decreased lung volumes. In Patient 3, a 58-year-old man with advanced melanoma who was treated with nivolumab, chest CT at 7 weeks of therapy revealed bilateral ground-glass opacities, reticular opacities, and small areas of consolidation in predominantly lower and peripheral distribution (Panel D, arrows), indicative of a pattern of nonspecific interstitial pneumonia.
