Abstract
[Purpose] We performed early physiotherapy for elderly patients with pneumonia admitted to an intensive care unit (ICU), and examined the effects of this early physiotherapy on the severity of pneumonia. [Subjects and Methods] Patients for whom physiotherapy was started the day after admission to the ICU (acute phase) were assigned to the early intervention group and compared with patients in the standard intervention group. All patients were divided into three groups (Groups I, II, and III) based on the severity of pneumonia. We evaluated the ICU admission period, hospitalization period, and activities of daily living (ADL) before and after admission. [Results] With respect to the severity of pneumonia, Group II showed significant differences in the ICU admission period and rates of change in the operating range, cognitive domain, and Functional Independence Measure (FIM). Group III showed significant differences in the ICU admission period and rate of change in the cognitive domain (FIM item). The results were more favorable in the early intervention group than in the standard intervention group. [Conclusion] The ICU admission period was shorter and a reduction in the ADL level was prevented in Groups II, and III compared to Group I. This may have occurred because of the early rehabilitation.
Key words: Pneumonia, Early physiotherapy, Intensive care unit
INTRODUCTION
In Japan, ≥95% of persons who die of pneumonia are >65 years of age1). This raises the issue of pneumonia treatment in the acute phase with an emphasis on the importance of early intervention by physical therapists. Although early rehabilitation shows favorable effects on the respiratory, cardiovascular and locomotor systems and mental state of bedridden patients, excessive rest by elderly patients with pneumonia often leads to long-term recumbency and a reduction in activities of daily living (ADL)2).
Positive physiotherapy is not associated with adverse events in the intensive care unit (ICU) and can be safely performed under risk management3,4,5). Many studies have investigated the effects of exercise therapy early after admission to the ICU on early rehabilitation6, 7). The presence of protracted functional or ADL disorders has been recognized in previous ICU treatment assessments8, 9). Early rehabilitation by physical therapists may prevent pneumonia-related disuse syndrome, and is potentially an important treatment, considering patient prognoses and times until discharge.
In this study, we performed early physiotherapy for elderly patients admitted to an ICU with pneumonia, and examined the influence of early physiotherapy on the ICU admission period, hospitalization period, and ADL upon discharge with respect to the severity of pneumonia.
SUBJECTS AND METHODS
One hundred ninety-two elderly patients admitted to an ICU with community-acquired pneumonia between January 2011 and November 2014 were included in this study. Criteria for ICU admission included the presence of pneumonia on chest X-rays, presence of clinical symptoms, and an appropriate revised American Thoracic Society score10).
Early physiotherapy began the day after admission (acute phase) and was introduced in January 2013.
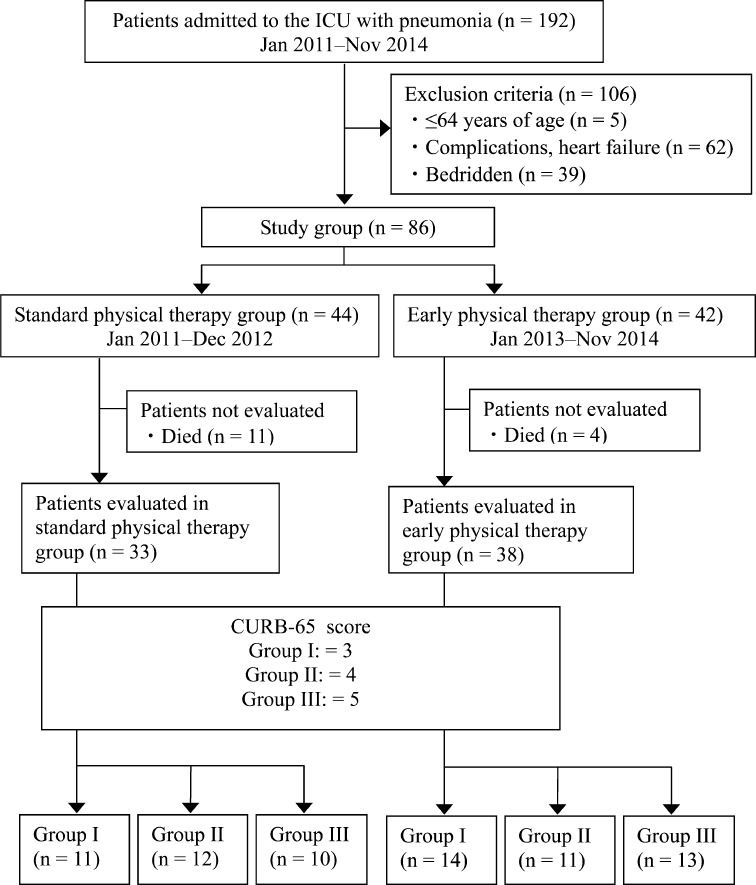
Thirty-eight patients treated after the introduction of early physiotherapy (January 2013 to November 2014) were assigned to the early intervention group. Thirty-three patients treated before the introduction of early physiotherapy (January 2011 to December 2012) were assigned to the standard intervention group. The severity of pneumonia on admission was evaluated using the Confusion, Urea, Respiratory rate, Blood pressure, and age >65 (CURB-65) score11). Patients scoring 3 points were assigned to Group I, those scoring 4 points were assigned to Group II, and those scoring 5 points were assigned to Group III (Fig. 1).
Fig. 1.
Flow diagram of the patients
We excluded patients aged ≤64 years, those bedridden before the onset of pneumonia, those with serious complications such as severe heart failure, and those who were discharged due to death.
The study protocol was approved by the ethics review board of Kanetsu Central Hospital. Consent to participate in this study was obtained from the patients after sufficient explanation of the study content. The study was conducted in accordance with the ethical principles of the Helsinki Declaration and with the protection of all patients’ information.
In the early intervention group, respiration training guidance, sputum elimination assistance12), and range-of-motion exercises (ROM ex) of the upper and lower limbs were conducted on the day of admission or the day after. Early rehabilitation was performed when possible. Respiration training was carried out by performing 10 sessions of slow, deep breathing starting immediately after admission13). Furthermore, the patients were instructed to perform self-sputum elimination using the active cycle of breathing technique with assistance14). ROM ex of the upper limbs (scapula, shoulder, elbow, wrist, and fingers) and lower limbs (hip, knee, ankle, and toes) was conducted in all ranges and directions of motion. This was continued from the day of admission, even for unconscious patients. Passive exercise was started and switched to active exercise when instructions could be followed. Early rehabilitation was conducted from the day of admission when the body temperature was controlled at <38 °C. When fever (≥38 °C), orthostatic hypotension, vomiting, or dyspnea was observed, early rehabilitation was discontinued. Initially, the patients were instructed to sit in a wheelchair. Standing and gait training were introduced in accordance with the patient’s condition.
In the standard intervention group, no intervention was performed by physical therapists immediately after admission. Sputum elimination and rehabilitation were conducted by ward nurses. After ≥1 week, when the pneumonia was expected to improve and the general condition had become stable, intervention by physical therapists was performed.
In each group, the intervention was performed for 40 minutes once a day.
The evaluation items comprised gender, age, body mass index, CURB-65 score on admission, ICU admission period, hospitalization period, and Functional Independence Measure (FIM) before admission and upon discharge.
The CURB-65 score11) was used to evaluate the severity of pneumonia. In the CURB-65 scoring system, 4 laboratory data items are evaluated; age is also assessed. CURB-65 scores range from 0 to 5. A higher score indicates a more severe condition in which the grade of invasiveness is more advanced (Table 1).
Table 1. CURB-65.
| CURB-65 | |
|---|---|
| Symptom | Points |
| Confusion | 1 |
| BUN>19 mg/dl | 1 |
| Respiratory rate≥30 | 1 |
| SBP<90mmHg, DBP≤60mmHg | 1 |
| Age≥65 | 1 |
CURB-65 is a clinical prediction rule that has been validated for predicting mortality in community-acquired pneumonia.
For ADL assessment, the FIM was used15). We evaluated the FIM before admission and upon discharge. The FIM upon discharge was subtracted from that before admission to obtain the FIM change. The FIM before admission was evaluated based on information obtained through inquiry with the patients and their families.
The results of the early and standard intervention groups were compared using the t-test. The results of the severity of pneumonia were compared between the two groups using the Mann-Whitney U-test. SPSS statistical software (version 17.0; SPSS, Inc., Chicago, IL, USA) was used for all statistical analyses. A p-value ≤ 0.05 was regarded as statistically significant.
RESULTS
The results of the standard and early intervention groups were compared. There were no significant differences in age, or body mass index. However, the ICU admission period was shorter and the rate of change in the FIM was smaller in the early intervention group than in the standard intervention group. Patients in the early intervention group also exhibited more favorable ADL upon discharge (Table 2). With respect to the severity of pneumonia, Group I exhibited no significant differences in the evaluation items. Group II showed significant differences in the ICU admission period, locomotory/cognitive domains and rate of change in the FIM. Group III showed significant differences in the ICU admission period and rate of change in the cognitive domain. The results were favorable in the early intervention group (Table 3).
Table 2. Comparison between standard and early intervention groups.
| Standard intervention group |
Early intervention group |
||
|---|---|---|---|
| Patients, n (male/female) | 33 (26/7) | 38 (23/15) | |
| Age, years | 80.5 ± 6.1 | 82.2 ± 7.6 | |
| Body mass index | 20.06 ± 1.8 | 20.1 ± 2.5 | |
| Interval until the start of physiotherapy, days | 10.27 ± 3.03 | 1.63 ± 1.03 | |
| Admission period, days | 37.7 ± 13.8 | 31.7 ± 16.7 | |
| ICU admission period, days | 15.45 ± 3.76 | 12.03 ± 4.14 ** | |
| CURB-65 score / n | 3 / 11 | 3 / 14 | |
| 4 / 12 | 4 / 11 | ||
| 5 / 10 | 5 / 13 | ||
| FIM before admission | 81.9 ± 12.7 | 81.9 ± 7.04 | |
| Locomotory domain | 56.8 ± 10.9 | 57.7 ± 5.8 | |
| Cognitive domain | 25.3 ± 2.6 | 24.2 ± 2.5 | |
| FIM on dischargem | 61.4 ± 16.7 | 67.6 ± 9.2 | |
| Locomotory domain | 41.5 ± 12.6 | 46.9 ± 8.4 * | |
| Cognitive domain | 18.4 ± 4.5 | 19.5 ± 3.3 | |
| Rate of change in FIM | 20.3 ± 7.6 | 14.3 ± 5.7 ** | |
| Locomotory domain | 15.3 ± 7.1 | 10.8 ± 5.3 * | |
| Cognitive domain | 6.6 ± 2.8 | 4.7 ± 2.2 ** | |
Data are presented as mean ± standard deviation unless otherwise indicated. *p < 0.05, **p < 0.01. ICU: intensive care unit, CURB-65: The Confusion, Urea, Respiratory rate, Blood pressure, and age >65, FIM: Functional Independence Measure
Table 3. Background and effects of intervention with respect to severity of pneumonia.
| CURB-65 score | Group I | Group II | Group III | |||
|---|---|---|---|---|---|---|
| 3 | 4 | 5 | ||||
| Patients, n | Standard | Early | Standard | Early | Standard | Early |
| 11 | 14 | 12 | 11 | 10 | 13 | |
| Age, years | 75.5 ± 6.4 | 78.1 ± 6.7 | 83.3 ± 4.2 | 87.7 ± 4.2 | 82.5 ± 4.5 | 82.0 ± 8.4 |
| Body mass index | 20.2 ± 1.6 | 20.4 ± 2.8 | 20.1 ± 1.9 | 20.9 ± 2.7 | 19.8 ± 2.1 | 19.6 ± 2.4 |
| Admission period, days | 29.7 ± 17.8 | 22.1 ± 14.9 | 30.5 ± 13.3 | 26.2 ± 17.7 | 46.1 ± 14.5 | 42.0 ± 11.6 |
| ICU admission period, days | 11.9 ± 2.9 | 9.8 ± 2.7 | 14.7 ± 3.9 | 10.7 ± 4.7 ** | 17.1 ± 3.6 | 13.5 ± 2.6 * |
| FIM before admission | 87.1 ± 11.1 | 84.6 ± 6.8 | 76.2 ± 15.3 | 79.5 ± 2.9 | 77.0 ± 4.6 | 75.5 ± 5.1 |
| Locomotory domain | 60.4 ± 8.7 | 59.7 ± 5.2 | 53.4 ± 12.9 | 54.3 ± 3.7 | 53.4 ± 7.6 | 54.3 ± 7.2 |
| Cognitive domain | 26.6 ± 2.9 | 24.9 ± 2.6 | 24.6 ± 2.3 | 24.3 ± 1.0 | 23.6 ± 3.4 | 21.7 ± 2.6 |
| FIM upon discharge | 69.3 ± 14.3 | 70.1 ± 11.8 | 53.8 ± 14.3 | 64.3 ± 1.6 | 46.6 ± 8.6 | 52.5 ± 1.8 |
| Locomotory domain | 49.6 ± 9.3 | 49.3 ± 8.8 | 34.4 ± 8.1 | 43.2 ± 2.3* | 28.6 ± 3.6 | 35.7 ± 4.5 |
| Cognitive domain | 19.8 ± 5.1 | 20.8 ± 5.4 | 18.2 ± 3.0 | 20.5 ± 1.6 | 13.4 ± 1.8 | 16.8 ± 2.9 |
| Rate of change in FIM | 13.4 ± 5.1 | 12.4 ± 4.5 | 23.4 ± 4.3 | 13.5 ± 2.3** | 31.0 ± 7.2 | 23.8 ± 3.3 |
| Locomotory domain | 10.0 ± 5.2 | 9.4 ± 4.6 | 18.0 ± 5.6 | 4.6 ± 8.4* | 24.9 ± 7.3 | 18.5 ± 2.4 |
| Cognitive domain | 5.6 ± 2.3 | 5.2 ± 2.5 | 6.6 ± 1.3 | 4.5 ± 7.4* | 10.6 ± 3.2 | 5.3 ± 1.5** |
Data are presented as mean ± standard deviation unless otherwise indicated. *p < 0.05, **p < 0.01. ICU: intensive care unit, CURB-65: The Confusion, Urea, Respiratory rate, Blood pressure, and age >65, FIM: Functional Independence Measure. Group I comprised patients scoring 3 points on CURB-65 score, Group II comprised patients scoring 4 points, and Group III comprised patients scoring 5 points
DISCUSSION
We performed early physiotherapy for elderly patients with pneumonia admitted to an ICU and examined its influence on the severity of pneumonia. We compared the results of the standard and early intervention groups. In the early intervention group, the ICU admission period was significantly shorter and the rate of change in the FIM was smaller than in the standard intervention group. The FIM upon discharge of the early intervention group was better than that of the standard intervention group. Another study evaluated the effects of early physiotherapy on patients with pneumonia, including those with a severe clinical status, admitted to an ICU and reported improvement in ADL, reduction of delirium, shortening of the artificial respiration period, shortening of the ICU admission period, shortening of the hospitalization period, improvement in the 6-minute walking distance, improvement in health-related quality of life, and improvement in muscle strength3). The results of the present study also demonstrate the beneficial effects of early physiotherapy on ADL and the ICU admission period. This is important with respect to the patient’s prognosis at home and reductions in health expenditures.
In terms of the severity of pneumonia, there were no effects of early intervention among the patients in Group I, who showed the mildest conditions. This was possibly because the severity of pneumonia was low, the ICU admission period was short, and the progression of disuse syndrome was slight in this group.
In Group II, comparison of the rate of change in the FIM locomotory and cognitive domains revealed better results in the early intervention group. In the locomotory domain, the prevention of ICU-acquired weakness (ICUAW) may have contributed to this result. Five factors, namely multiple organ failure, inactivity, hyperglycemia, steroids, and neuromuscular blockers, may be primarily involved in the development of ICUAW3). ICUAW influences artificial respiratory control, prolongs the ICU admission period, and delays ADL recovery16). Early intervention by physiotherapy may have reversed the patients’ inactivity, preventing ICUAW. Another study reported that continuous passive exercise of the unilateral lower limb significantly ameliorated both muscular atrophy and decreases in the muscular protein level in patients with severe respiratory failure when the contralateral lower limb was regarded as the control4). In the early intervention group, passive ROM ex were conducted even for unconscious patients. This may have contributed to the favorable results in the locomotory domain through similar effects. Long-term inactivity of patients in an ICU affects the patients’ ADL, and how best to promote physical activity in ICUs must be reviewed.
In Group III, comparison of the rate of change in the cognitive domain revealed the early intervention group had better results, as reported for Group II. Some studies have described the lack of an association of cognitive impairment after intensive care with the severity of the patient’s condition and length of the ICU admission period17). However, in the present study, the ICU admission period was longer in patients with more severe pneumonia, and cognitive impairment was more marked. If early intervention by physiotherapy shortens the ICU admission period, cognitive impairment may be reduced. Delirium reduces the cognitive level of many patients in an ICU18). However, one study reported that physiotherapy during artificial respiration reduced delirium19), and another study indicated that early physiotherapy decreased the incidence of delirium in patients with acute respiratory disorder7). Thus, physiotherapy is beneficial for patients’ physical and mental states. This is consistent with the results of the present study. Early physiotherapy may help to prevent reductions in the cognitive level, regardless of severity.
Although the effects of early intervention by physiotherapy for elderly patients with pneumonia in an ICU depend on the severity of pneumonia, early physiotherapy may shorten the ICU admission period and prevent decline in ADL. Physiotherapy should be recognized as an effective treatment method that prevents complications and improves the prognosis associated with ADL, and not solely as a method to prevent disuse syndrome. Further research is needed in this field.
Acknowledgments
The authors thank the intensive care unit team members for their participation and the physical therapists and the nursing team members for their extensive collaboration.
REFERENCES
- 1.Teramoto S, Fukuchi Y, Sasaki H, et al. Japanese Study Group on Aspiration Pulmonary Disease: High incidence of aspiration pneumonia in community- and hospital-acquired pneumonia in hospitalized patients: a multicenter, prospective study in Japan. J Am Geriatr Soc, 2008, 56: 577–579. [DOI] [PubMed] [Google Scholar]
- 2.Okuno Y, Miyasaka T, Dobashi K: Factors influencing the outcome of acute rehabilitation: functional independence measure assessment at discharge. J Phys Ther Sci, 2012, 24: 491–494. [Google Scholar]
- 3.Schweickert WD, Kress JP: Implementing early mobilization interventions in mechanically ventilated patients in the ICU. Chest, 2011, 140: 1612–1617. [DOI] [PubMed] [Google Scholar]
- 4.Griffiths RD, Palmer TE, Helliwell T, et al. : Effect of passive stretching on the wasting of muscle in the critically ill. Nutrition, 1995, 11: 428–432. [PubMed] [Google Scholar]
- 5.Bailey P, Thomsen GE, Spuhler VJ, et al. : Early activity is feasible and safe in respiratory failure patients. Crit Care Med, 2007, 35: 139–145. [DOI] [PubMed] [Google Scholar]
- 6.Thomas JA, McIntosh JM: Are incentive spirometry, intermittent positive pressure breathing, and deep breathing exercises effective in the prevention of postoperative pulmonary complications after upper abdominal surgery? A systematic overview and meta-analysis. Phys Ther, 1994, 74: 3–10, discussion 10–16. [DOI] [PubMed] [Google Scholar]
- 7.Needham DM, Korupolu R, Zanni JM, et al. : Early physical medicine and rehabilitation for patients with acute respiratory failure: a quality improvement project. Arch Phys Med Rehabil, 2010, 91: 536–542. [DOI] [PubMed] [Google Scholar]
- 8.Herridge MS, Cheung AM, Tansey CM, et al. Canadian Critical Care Trials Group: One-year outcomes in survivors of the acute respiratory distress syndrome. N Engl J Med, 2003, 348: 683–693. [DOI] [PubMed] [Google Scholar]
- 9.Herridge MS, Tansey CM, Matté A, et al. Canadian Critical Care Trials Group: Functional disability 5 years after acute respiratory distress syndrome. N Engl J Med, 2011, 364: 1293–1304. [DOI] [PubMed] [Google Scholar]
- 10.Phua J, Ngerng WJ, Lim TK: The impact of a delay in intensive care unit admission for community-acquired pneumonia. Eur Respir J, 2010, 36: 826–833. [DOI] [PubMed] [Google Scholar]
- 11.Lim WS, van der Eerden MM, Laing R, et al. : Defining community acquired pneumonia severity on presentation to hospital: an international derivation and validation study. Thorax, 2003, 58: 377–382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Akazawa C, Egawa T, Tamaki A: Standardization of the squeezing technique for expectoration in terms of timing, pressure, and direction. J Phys Ther Sci, 2012, 24: 1247–1249. [Google Scholar]
- 13.Pasquina P, Tramèr MR, Granier JM, et al. : Respiratory physiotherapy to prevent pulmonary complications after abdominal surgery: a systematic review. Chest, 2006, 130: 1887–1899. [DOI] [PubMed] [Google Scholar]
- 14.Cecins NM, Jenkins SC, Pengelley J, et al. : The active cycle of breathing techniques—to tip or not to tip? Respir Med, 1999, 93: 660–665. [DOI] [PubMed] [Google Scholar]
- 15.Keith RA, Granger CV, Hamilton BB, et al. : The functional independence measure: a new tool for rehabilitation. Adv Clin Rehabil, 1987, 1: 6–18. [PubMed] [Google Scholar]
- 16.Kress JP, Pohlman AS, O’Connor MF, et al. : Daily interruption of sedative infusions in critically ill patients undergoing mechanical ventilation. N Engl J Med, 2000, 342: 1471–1477. [DOI] [PubMed] [Google Scholar]
- 17.Hopkins RO, Weaver LK, Collingridge D, et al. : Two-year cognitive, emotional, and quality-of-life outcomes in acute respiratory distress syndrome. Am J Respir Crit Care Med, 2005, 171: 340–347. [DOI] [PubMed] [Google Scholar]
- 18.Ely EW, Shintani A, Truman B, et al. : Delirium as a predictor of mortality in mechanically ventilated patients in the intensive care unit. JAMA, 2004, 291: 1753–1762. [DOI] [PubMed] [Google Scholar]
- 19.Schweickert WD, Pohlman MC, Pohlman AS, et al. : Early physical and occupational therapy in mechanically ventilated, critically ill patients: a randomised controlled trial. Lancet, 2009, 373: 1874–1882. [DOI] [PMC free article] [PubMed] [Google Scholar]