Abstract
Purpose
The Physiological and Operative Severity Score for enUmeration of Mortality and morbidity (POSSUM) and its Portsmouth modification (P-POSSUM) are comprehensive assessment methods for evaluating patient and surgical factors widely used to predict 30-day mortality rates. In this retrospective study, we evaluated the usefulness of POSSUM and P-POSSUM in predicting 30-day mortality after intraoperative cardiac arrests in adult patients undergoing non-cardiac surgery.
Materials and Methods
Among 190486 patients who underwent anesthesia, 51 experienced intraoperative cardiac arrest as defined in our study protocol. Predicted mortality rates were calculated using POSSUM and P-POSSUM equations and were compared with actual outcomes using exponential and linear analyses. In addition, a receiver operating characteristic curve analysis was undertaken, and area-under-the-curve (AUC) values with confidence intervals (CIs) were calculated for POSSUM and P-POSSUM.
Results
Among the 51 patients with intraoperative cardiac arrest, 32 (62.7%) died within 30 days postoperatively. The overall predicted 30-day mortality rates using POSSUM and P-POSSUM were 65.5% and 57.5%, respectively. The observed-to-predicted (O:E) ratio for the POSSUM 30-day mortality was 1.07, with no significant difference between the observed and predicted values (χ2=4.794; p=0.779). P-POSSUM predicted mortality equally well, with an O:E ratio of 1.10 (χ2=8.905; p=0.350). AUC values (95% CI) were 0.771 (0.634-0.908) and 0.785 (0.651-0.918) for POSSUM and P-POSSUM, respectively.
Conclusion
Both POSSUM and P-POSSUM performed well to predict overall 30-day mortality following intraoperative cardiac arrest in adults undergoing non-cardiac surgery at a university teaching hospital in Korea.
Keywords: Cardiac arrest, mortality, surgery
INTRODUCTION
Despite its low incidence, intraoperative cardiac arrest is a potentially catastrophic event, leading to a high mortality rate.1 Complicating patient, anesthetic, and surgical factors can be associated with the incidence and survival outcomes of cardiac arrest in the operating room.2 Although cardiac arrest due solely to anesthesia and mainly related to medication and airway issues can still occur in clinical practice, its incidence has been gradually decreasing in modern anesthetic practice, and patients with anesthesia-related cardiac arrest show a higher survival rate than those with intraoperative cardiac arrest due to other causes.3 The overall survival outcome after intraoperative cardiac arrest is generally better than that of in-hospital cardiac arrest,4 as some surgical causes of cardiac arrest are more likely to be reversible and the immediate availability of physician-led care in the operating room could improve survival after arrest by influencing the speed and quality of the response. Recent major studies with large surgical populations reported that the incidence and survival outcomes of intraoperative cardiac arrest may mainly depend on patients' physiological status and operative severity.1,4 Although much attention has rightly been focused on issues surrounding the frequency and risk factors of cardiac arrest in surgical patients, there is relatively little information regarding risk assessment tools that can predict its outcome.
Although several prediction models for mortality after in- or out-of-hospital cardiac arrest have been developed,5,6 these models seem to be unsuitable for surgical patients. Also, preoperative cardiac risk assessment based on cardiac function and functional capacity does not fully account for other systemic physiological factors and the intraoperative course.7 The Physiological and Operative Severity Score for enUmeration of Mortality and morbidity (POSSUM) and its Portsmouth modification (P-POSSUM) are comprehensive assessment methods used to evaluate patient and surgical factors, consisting of a 12-item physiological and 6-item operative severity data set.8,9 Each item has a 4-grade exponential severity score used to calculate a predicted percent morbidity or mortality using logistic regression analysis equations.10 The POSSUM system was initially developed for comparative surgical audits and has been shown to be a good predictor of morbidity and mortality in various types of surgery.10 We hypothesized that this well-validated scoring system would produce standardized and balanced information on the major patient and surgical factors that influence survival outcomes following intraoperative cardiac arrest.
The aim of this study was to examine the value of POSSUM and P-POSSUM in predicting 30-day mortality following intraoperative cardiac arrest in adult patients undergoing non-cardiac surgery at a university teaching hospital.
MATERIALS AND METHODS
The Institutional Review Board of Yonsei University Health System approved this study. We analyzed all reported cases of intraoperative cardiac arrest in consecutive patients who underwent non-cardiac surgery and required general or regional anesthesia at Severance Hospital, a university teaching hospital, between January 2007 and December 2012.
For the purpose of this study, we defined cardiac arrest as the absence of cardiac rhythm or the presence of chaotic cardiac rhythm that required the initiation of any component of basic and/or advanced cardiac life support. Only cardiac arrests that occurred after anesthesia had been initiated in the operating room were included. Intraoperative cardiac arrest cases were identified from an anesthesia database and a central electronic medical records system. We reviewed these cases in detail and completed a quality assessment form for each patient. The form contained the date and location; patient demographic data according to the American Society of Anesthesiologists (ASA) physical status classification; surgical procedures; surgical area and intraoperative course; anesthesia provider information; and detailed descriptions of airway, respiratory, cardiocirculatory, neurological, renal, and miscellaneous events in the intraoperative period. The cause of the arrest was determined from these records, the electrocardiograms, and the laboratory values generated from the operating suites. In addition, we obtained the 12-item physiological and 6-item operative severity data sets for the POSSUM analysis (Supplementary Table 1 and 2, only online).10 These scoring assessments for the POSSUM calculation were completed by the surgeon and anesthesia staff responsible for each patient based on the results obtained at the time closest to surgery. The data were complete for all 51 patients with both physiological and operative severity scores. The mortality risk was calculated using the following POSSUM and P-POSSUM equations:10
The POSSUM equation: ln (R/1-R)=-7.04+(0.13×physiological score)+(0.16×operative severity score), where R is the predicted mortality rate.
The P-POSSUM equation: ln (R'/1-R')=-9.065+(0.1692×physiological score)+(0.1550×operative severity score), where R' is the predicted mortality rate.
We reviewed the postoperative course of each case of intraoperative cardiac arrest. Patient outcomes were classified as survival or mortality within 30 days after intraoperative cardiac arrest.
Statistical analysis
Considering that exponential analysis for POSSUM and linear analysis for P-POSSUM have been recommended as appropriate statistical methods,10 we used these methods to predict mortality for the 30-day postoperative period, replicating the analyses used by Wijesinghe, et al.11 The observed-to-predicted (O:E) ratio was also calculated for each analysis. Exponential analysis calculated the number of individuals expected to die within each probability group by subtracting those with a risk higher than the upper group limit from those with a risk higher than the lower group limit. Negative risk values were dealt with by widening the band until it contained a positive number of deaths. Linear analysis calculated the average individual risk within each risk band multiplied by the number of individuals in the band. A comparison was then made between the observed and expected death rate ratio. A ratio over 1.0 indicated an underprediction of death, and that below 1.0 indicated an overprediction of death. When the values of the observed and expected death rates were both 0, the ratio was 1.0. The χ2 test was used to detect differences between predicted and observed mortality. In addition to the above calculations, a receiver operating characteristic curve analysis was undertaken, and area-under-the-curve (AUC) values with confidence intervals were calculated for POSSUM, P-POSSUM, and ASA grade. The cut-off value of the ASA grade was ≥3 with a 0.3701 Youden index. The accuracy of the prediction was assessed by comparing AUC values using MedCalc (version 12.7.0; Med-Calc Software, Ostend, Belgium). The normality of data distribution was assessed using the Kolmogorov-Smirnov test. Ordinal data and continuous data that were not normally distributed are presented as medians with interquartile ranges. These data were compared between groups using the Wilcoxon rank-sum test. Categorical data are reported as the numbers of patients with percentages. Statistical analyses were performed using SAS (version 9.2; SAS Institute, Inc., Cary, NC, USA). A p value<0.05 was considered statistically significant.
RESULTS
In the 6 years of the study, anesthesia was administered in 190486 cases, general anesthesia in 171377 cases, and regional anesthesia in 19109 cases. Intraoperative cardiac arrest as defined by our study protocol was confirmed in 51 patients. Preoperative patient characteristics of the survival and 30-day mortality groups are listed in Table 1. There were 34 men and 17 women, ranging in age from 19 to 91 years (mean, 56 years). There were more patients with a poor ASA physical status in the mortality group than in the survival group. Patients with liver disease, poor functional status, preoperative intubated status, and non-alert mental status showed a higher mortality rate. Operative characteristics of the survival and 30-day mortality groups are listed in Table 2. All 51 patients had been given general anesthesia. Major surgery with high risk, use of vasopressors, and massive transfusion were significantly associated with high mortality.
Table 1. Preoperative Patient Characteristics of the Survival and 30-Day Mortality Groups.
| Survival (n=19) | Mortality (n=32) | p value | |
|---|---|---|---|
| Age (%) | 0.563 | ||
| <65 | 10 (34) | 20 (66) | |
| ≥65 | 9 (43) | 12 (57) | |
| Gender (%) | 0.543 | ||
| Men | 14 (42) | 20 (58) | |
| Women | 5 (30) | 12 (70) | |
| ASA PS (%) | 0.010 | ||
| I, II | 10 (67) | 5 (33) | |
| III, IV, V | 9 (25) | 27 (75) | |
| Trauma (%) | 0.739 | ||
| Yes | 2 (40) | 3 (60) | |
| No | 17 (37) | 29 (63) | |
| Diabetes mellitus (medication or insulin) (%) | 0.392 | ||
| No | 18 (40) | 27 (60) | |
| Yes | 1 (17) | 5 (83) | |
| Hypertension (medication) (%) | 0.547 | ||
| No | 9 (28) | 24 (72) | |
| Yes | 10 (56) | 8 (44) | |
| Renal insufficiency (%)* | 1.000 | ||
| No | 15 (39) | 24 (61) | |
| Yes | 4 (34) | 8 (66) | |
| Liver disease (%)† | 0.037 | ||
| No | 19 (44) | 25 (56) | |
| Yes | 0 (0) | 7 (100) | |
| Cerebrovascular disease (%)‡ | 1.000 | ||
| No | 18 (39) | 29 (61) | |
| Yes | 1 (25) | 3 (75) | |
| Heart disease (%)§ | 0.236 | ||
| No | 18 (41) | 26 (59) | |
| Yes | 1 (25) | 6 (85) | |
| SIRS/sepsis (%) | 0.074 | ||
| No | 18 (43) | 24 (57) | |
| Yes | 1 (12) | 8 (88) | |
| Functional status (%) | 0.019 | ||
| ≥4 METS | 13 (57) | 10 (43) | |
| <4 METS | 6 (22) | 22 (78) | |
| Consciousness (%) | 0.006 | ||
| Alert | 17 (52) | 16 (48) | |
| Not alert | 2 (12) | 16 (88) | |
| Intubated status (%) | 0.027 | ||
| No | 17 (49) | 18 (51) | |
| Yes | 2 (13) | 14 (87) |
ASA PS, American Society of Anesthesiologists physical status; SIRS, systemic inflammatory response syndrome; METS, metabolic equivalents.
Values are number of patients (%).
*Acute/chronic renal failure and/or on dialysis, †Primary liver disease, ‡History of diagnosed cerebrovascular events, §Congestive heart failure.
Table 2. Operative Characteristics of the Survival and 30-Day Mortality Groups.
| Survival (n=19) | Mortality (n=32) | p value | |
|---|---|---|---|
| Operative severity (%)* | 0.018 | ||
| Major | 4 (19) | 18 (81) | |
| Moderate/minor | 15 (52) | 14 (48) | |
| Urgency (%) | 0.365 | ||
| Elective | 8 (48) | 9 (52) | |
| Emergency | 11 (33) | 23 (67) | |
| Time (%) | 0.547 | ||
| Day, Mon-Fri | 12 (35) | 23 (65) | |
| Night, holiday | 7 (44) | 9 (56) | |
| Re-operation (%)† | 0.543 | ||
| No | 14 (42) | 20 (58) | |
| Yes | 5 (30) | 12 (70) | |
| Use of vasopressors (%) | 0.004 | ||
| No | 14 (59) | 10 (41) | |
| Yes | 5 (19) | 22 (81) | |
| ≥10 PRBC transfusion (%) | 0.001 | ||
| No | 18 (55) | 15 (45) | |
| Yes | 1 (6) | 17 (94) | |
| Duration of surgery (%) | 0.132 | ||
| <2 hr | 4 (24) | 13 (76) | |
| ≥2 hr | 17 (50) | 17 (50) |
PRBC, packed red blood cell.
Values are number of patients (%).
*Operative severity was classified according to Physiological and Operative Severity Score for enUmeration of Mortality and morbidity score.8 Major surgery includes any laparotomy, bowel resection, cholecystectomy with choledochotomy, pancreatic or liver surgery, esophagogastrectomy, and vascular procedures, †Reoperation due to any surgical complication within 7 days after the initial operation.
The overall incidence of intraoperative cardiac arrest due to all causes was 2.67 per 10000 anesthetic cases. The main cause of cardiac arrest was hypovolemia (43.1%), followed by cardiac origin (39.2%), sepsis or multi-organ failure (15.6%), and hypoxic event (1.9%) (Table 3). With regard to initial electrocardiogram rhythm in arrest cases, ventricular tachycardia or fibrillation, pulseless electrical activity, and asystole were observed in 24 (47.0%), 21 (41.1%), and 6 patients (11.7%), respectively. Intraoperative cardiac arrest due to hypovolemia and non-shockable rhythm showed a poor survival rate. All patients immediately received cardiopulmonary resuscitation according to recommended guidelines, and delayed detection or improper treatment of arrest was not observed in our study. After resuscitation, spontaneous circulation was recovered in most of the patients; however, three patients died on the operating table. Of the resuscitated patients, 35 were transferred to the surgical intensive care unit after surgery. Among 51 patients with arrest, 24 (47.0%) died within 24 h and 32 (62.7%) died within 30 days. Most of the deaths observed within 24 h postoperatively, including the three deaths on the operating table, involved patients who were in an extremely high-risk group (mortality risk of more than 90%). Additionally, two patients died due to cancer progression 4 and 18 months after the arrest, respectively, and one patient experienced neurologic deficit requiring rehabilitation.
Table 3. Characteristics of Cardiac Arrests in the Survival and 30-Day Mortality Groups.
| Survival (n=19) | Mortality (n=32) | p value | |
|---|---|---|---|
| Causes (%) | 0.005 | ||
| Cardiac | 12 (60) | 8 (40) | |
| Hypovolemic | 3 (14) | 19 (86) | |
| Sepsis/MOF | 3 (38) | 5 (62) | |
| Hypoxic | 1 (100) | 0 (0) | |
| Initial electrocardiogram rhythm (%) | 0.023 | ||
| Shockable (VT/VF) | 13 (55) | 11 (45) | |
| Non-shockable (PEA/asystole) | 6 (23) | 21 (77) |
MOF, multi-organ failure; VT, ventricular tachycardia; VF, ventricular fibrillation; PEA, pulseless electrical activity.
Values are number of patients (%).
Among the 51 patients who experienced intraoperative cardiac arrest, the overall predicted 30-day mortality rates using POSSUM and P-POSSUM were 65.5% and 57.5%, respectively. Table 4 shows the POSSUM physiological and operative severity scores and the mortality rates predicted by POSSUM and P-POSSUM in the survival and mortality groups. The POSSUM physiological and operative severity scores were significantly higher in the mortality group than in the survival group. The predicted mortality rates calculated by both POSSUM and P-POSSUM equations were significantly higher in the mortality group than in the survival group.
Table 4. POSSUM Scores and 30-Day Mortality Predicted by POSSUM and P-POSSUM in the Survival and Mortality Groups.
| Survival (n=19) | Mortality (n=32) | p value | |
|---|---|---|---|
| Physiological score | 24.00 (20.00-38.00) | 51.50 (31.75-56.50) | <0.001 |
| Operative severity score | 18.00 (11.00-23.00) | 23.00 (17.50-25.75) | 0.019 |
| Total score | 47.00 (31.00-56.00) | 73.00 (51.00-78.75) | <0.001 |
| POSSUM mortality (%) | 44.02 (6.06-68.56) | 95.02 (56.03-98.10) | <0.001 |
| P-POSSUM mortality (%) | 19.16 (1.84-54.21) | 95.46 (31.73-97.84) | <0.001 |
POSSUM, Physiological and Operative Severity Score for enUmeration of Mortality and morbidity; P-POSSUM, Portsmouth modification POSSUM.
Values are median (interquartile range) or number of patients.
The number of deaths predicted by POSSUM with exponential analysis is shown in Table 5. The O:E ratio for 30-day mortality was 1.07, and there was no significant difference between the observed and predicted values (χ2=4.794; df=8; p=0.779). P-POSSUM predicted 30-day mortality equally well when the linear analysis was used, with an O:E ratio of 1.10 and no significant difference between the predicted and observed values (χ2=8.905; df=8; p=0.350) (Table 6).
Table 5. POSSUM Prediction of Mortality Using Exponential Analysis.
| Predictive mortality rate (%) | No. of patients | Predicted number of deaths | Actual number of deaths within 30 days | O:E ratios for 30-day mortality |
|---|---|---|---|---|
| <10 | 8 | 0 | 1 | 0 |
| 10-29 | 3 | 0 | 2 | 0 |
| 20-29 | 1 | 0 | 0 | 1 |
| 30-49 | 5 | 2 | 4 | 2 |
| 40-49 | 4 | 2 | 3 | 1.50 |
| 50-89 | 12 | 7 | 7 | 1 |
| 60-89 | 8 | 5 | 3 | 0.60 |
| 70-89 | 3 | 2 | 2 | 1 |
| 80-89 | 2 | 2 | 1 | 0.50 |
| 90-100 | 23 | 21 | 18 | 0.86 |
| 0-100 | 51 | 30 | 32 | 1.07 |
O:E, observed-to-predicted; POSSUM, Physiological and Operative Severity Score for enUmeration of Mortality and Morbidity.
Table 6. P-POSSUM Prediction of Mortality Using Linear Analysis.
| Predictive mortality rate (%) | No. of patients | Predicted number of deaths | Actual number of deaths within 30 days | O:E ratios for 30-day mortality |
|---|---|---|---|---|
| <10 | 10 | 0 | 3 | 0 |
| 10-19 | 3 | 0 | 1 | 0 |
| 20-29 | 4 | 1 | 4 | 4 |
| 30-39 | 4 | 1 | 3 | 3 |
| 40-49 | 2 | 1 | 1 | 1 |
| 50-59 | 2 | 1 | 0 | 0 |
| 60-69 | 1 | 1 | 1 | 1 |
| 70-79 | 0 | 0 | 0 | 1 |
| 80-89 | 3 | 3 | 1 | 0.33 |
| 90-100 | 22 | 21 | 18 | 0.86 |
| 0-100 | 51 | 29 | 32 | 1.10 |
O:E, observed-to-predicted; P-POSSUM, Portsmouth Modification Physiological and Operative Severity Score for enUmeration of Mortality and Morbidity.
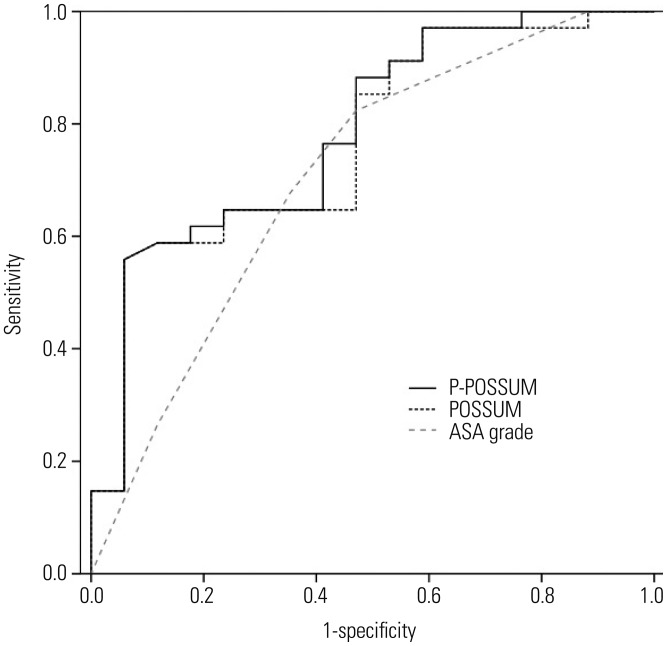
Receiver operating characteristic curves of POSSUM, P-POSSUM, and the ASA grade for predicting 30-day mortality following intraoperative cardiac arrest are shown in Fig. 1. The AUC values with 95% CIs were 0.771 (0.634-0.908), 0.785 (0.651-0.918), and 0.708 (0.549-0.866) for POSSUM, P-POSSUM, and the ASA grade, respectively. There were no statistical differences in the accuracy of the predictions between ASA grade and POSSUM (z=1.208; p=0.227), and P-POSSUM (z= 1.502; p=0.133).
Fig. 1. Receiver operator characteristic curves for the POSSUM, P-POSSUM, and American Society of Anesthesiologists (ASA) grade in the prediction of 30-day mortality after intraoperative cardiac arrest. The areaunder-the-curve values with 95% confidence intervals were 0.771 (0.634-0.908), 0.785 (0.651-0.918), and 0.708 (0.549-0.866) for POSSUM, P-POSSUM, and ASA grade, respectively. POSSUM, Physiological and Operative Severity Score for enUmeration of Mortality and morbidity; P-POSSUM, Portsmouth modification POSSUM.
DISCUSSION
The 30-day mortality rate of 62.7% following intraoperative cardiac arrest in the present study is similar to the 62.6% mortality rate reported in a recent study of 262 cases of intraoperative cardiac arrest.1 In this study, the predicted risks of mortality calculated by POSSUM and P-POSSUM were 65.5% and 57.5%, respectively, and these predicted values were close to the observed value. Furthermore, the predictive powers of the two systems were similar, with O:E ratios of 1.07 and 1.10 and AUC values of 0.771 and 0.785, respectively, indicating a high accuracy in predicting overall mortality.
POSSUM, as originally developed by Copeland, et al.,8 uses exponential analysis, which has been criticized for not being a standard statistical method and for the difficulties in assigning a risk score to an individual patient using this method.10 P-POSSUM using linear analysis was proposed by Whiteley, et al.9 to counter this shortcoming of POSSUM in overestimating mortality, especially in low-risk patients. POSSUM and P-POSSUM are generally known to overestimate the mortality rate for low-risk surgical procedures.10 However, P-POSSUM might be more accurate in specific procedures involving a high degree of difficulty, whereas POSSUM shows a tendency to overpredict the risk of death.12,13 In several studies, both POSSUM and P-POSSUM were reported to be good predictors of mortality following emergency surgery, with similar predictive powers.14,15 Collectively, previous studies indicate that the accuracy of these two systems can be affected by various patient characteristics and the clinical settings in which the surgeries are performed. The majority of previous studies regarding POSSUM and P-POSSUM have concentrated on surgical patients at low risk (mortality risk of less than 10%), whereas our study included a large number of predominantly higher-risk patients. This distinguishing distribution of the study population may diminish the tendency of mortality risk overestimation by the two systems, particularly by POSSUM. The reported O:E mortality ratio varied at each risk band in this study, similar to the findings of previous studies. This variation is mainly because the actual observed mortality is relatively low and, in smaller populations, one or two deaths can change the O:E ratio significantly. However, despite the small number of patients in each risk band, it should be recalled that both POSSUM and P-POSSUM showed a tendency of underestimation, particularly in the predicted 30-day mortality rate of less than 50%, contrasting with other studies. Thus, considering the potentially fatal outcome of intraoperative cardiac arrest, there is a possibility of unexpected mortality within 30 days after surgery in the low-risk group.
A recent multicenter study involving over 400 participating hospitals demonstrated that several patient characteristics and medical conditions were associated with lower survival rates after perioperative arrest.4 These predictors included older age and the presence of congestive heart failure, shock, metabolic abnormality, metastatic malignancy, renal insufficiency, sepsis, myocardial infarction, and neurologic disability. Interestingly, the POSSUM scoring system developed over 20 years ago reflects most of these predictors. In the present study, the POSSUM physiological score was nearly twice as high in the mortality group as it was in the survival group, and critically-ill patients with a high ASA grade had a higher mortality rate after arrest. A higher ASA grade is known as a predictor of both a higher incidence of intraoperative cardiac arrest and a poorer outcome.2 In this study, we could not find a statistical difference in the accuracy of prediction for mortality after cardiac arrest between ASA grade and POSSUM systems. Some physicians may argue that ASA grade is simpler to apply; however, ASA grading has the potential disadvantage of subjective fitness assessment. In addition, the ASA grade does not account for any operative severity components, and it cannot provide the predictive mortality rate as a percentage. Our results suggest that POSSUM systems provide useful information to physicians that can be used to identify high-risk patients (especially those with a mortality risk of more than 90%) who need close attention during perioperative care, and they may also be helpful in clinical decision-making related to a "do not resuscitate" order in cases of intraoperative cardiac arrest. Previous studies have shown that the POSSUM and P-POSSUM systems have been more reliable for mortality risk assessment than the ASA grade alone in patients undergoing high-risk surgery.16,17,18
Intraoperative blood loss, as indicated by the amount of blood transfused, is the single most important factor related to intraoperative cardiac arrest among various risk factors.1 Moreover, shockable arrest rhythms accompanied by massive surgical exsanguination showed a very poor response to defibrillation.4 In the current study, hypovolemia was the most common cause of intraoperative cardiac arrest (22 of 51 patients), and most of the patients were given a massive transfusion of more than 10 erythrocyte units during surgery (18 of 22 patients). Unfortunately, these cases resulted in high case fatality rate of 86% within 30 days postoperatively (19 of 22 patients). With the POSSUM physiological score, certain parameters such as low hemoglobin, low systolic blood pressure, and high pulse rate indicated a preexisting hypovolemic condition. However, with the POSSUM operative severity score, intraoperative blood loss of more than 1000 mL accounted for only 8 of 44 scores, as this score was derived from the general surgical population.8 This underweighted blood loss score may have led to a degree of inaccuracy in the POSSUM predictions in our study, although the POSSUM operative severity score included major surgery involving a high degree of difficulty and emergency surgery, which is closely associated with higher rates of surgical morbidity and mortality.
With regard to the type of anesthesia, no cases received a regional anesthesia in this study. Cardiac arrest due solely to anesthesia mainly related to anesthetics overdose and airway problems that may have been associated closely with general anesthesia.3 In this study, there were no cardiac arrest cases due solely to anesthesia. However, despite a low incidence, cardiac arrest wholly or partially attributable to anesthesia occurred in the operating room or the post-anesthesia care unit.3,19 In this study, one patient experienced cardiac arrest due to a loss of airway patency during a tracheostomy tube change in the operating room. In addition, three patients experienced cardiac arrest due to respiratory distress caused by narcotic overdose or inadequate reversal of muscle relaxants in the post-anesthesia care unit. We excluded these three cases of anesthesia-attributable arrests in the post-anesthesia care unit, as this study focused on patient and operative factors representing the POSSUM scoring system during surgery. All cases of intraoperative cardiac arrest, including those attributable to anesthesia, were in patients with a high ASA grade and other challenges, with cardiovascular problems being the predominant issues.3,19 Unfortunately, anesthesia-related factors are not included in the POSSUM systems. However, even if some contributory factors induced by anesthesia affect the occurrence and outcome of arrest in this study, our results still demonstrated that POSSUM and P-POSSUM performed satisfactorily in predicting mortality following cardiac arrest under general anesthesia.
This study is limited by the fact that it was a single-center study involving a small number of select patients. In a retrospective power analysis using a two-sided z-test, the power required to detect a difference in AUC values between POSSUM/P-POSSUM and the null hypothesis of 0.500 was 92.8% and 95.3% at a significance level of 0.05, respectively. Sample size, distribution, and different clinical settings may affect the ac curacies of the scoring systems.12,20 Thus, further research including a larger population may be needed to verify the value of POSSUM and P-POSSUM as indicators of outcome after cardiac arrest in surgical patients.
In conclusion, both POSSUM and P-POSSUM showed high accuracy in predicting overall 30-day mortality following intraoperative cardiac arrest in adults undergoing non-cardiac surgery at a university teaching hospital in Korea. Thus, in a research setting with adequate resources, POSSUM systems, as a basis for making clinical decisions, appear to be suitable risk assessment tools for predicting mortality following intraoperative cardiac arrest, especially in high-risk patients.
ACKNOWLEDGEMENTS
This study was supported by a new faculty research seed money grant of Yonsei University College of Medicine for 2015 (2015-32-0013).
Footnotes
The authors have no financial conflicts of interest.
Supplementary Materials
Supplementary Table 1. POSSUM Physiological Score.
| Score | ||||
|---|---|---|---|---|
| 1 | 2 | 4 | 8 | |
| Age, yrs | ≤60 | 61-70 | ≥71 | |
| Cardiac signs (chest radiograph) | No failure | Diuretic, digoxin, antianginal, or hypertensive therapy | Peripheral edema; warfarin therapy | Raised jugular venous pressure |
| Borderline cardiomegaly | Cardiomegaly | |||
| Respiratory signs (chest radiograph) | No dyspnea | Dyspnea on exertion | Limiting dyspnea | Dyspnea at rest |
| Mild COPD | Moderate COPD | Fibrosis or consolidation | ||
| Systolic blood pressure, mm Hg | 110-130 | 131-170 | ≥170 | ≤89 |
| 100-109 | 90-99 | |||
| Pulse, beats/min | 50-80 | 81-100 | 101-120 | ≥121 |
| 40-49 | ≤39 | |||
| Glasgow coma scale | 15 | 12-14 | 9-11 | ≤8 |
| Hemoglobin, g/100 mL | 13-16 | 11.5-12.9 | 10.0-11.4 | ≤9.9 |
| 16.1-17.0 | 17.1-18.0 | ≥18.1 | ||
| White cell count, ×1012/L | 4-10 | 10.1-20.0 | ≥20.1 | |
| 3.1-4.0 | ≤3.0 | |||
| Urea, mmol/L | ≤7.5 | 7.6-10.0 | 10.1-15.0 | ≥15.1 |
| Sodium, mmol/L | ≥136 | 131-135 | 126-130 | ≤125 |
| Potassium, mmol/L | 3.5-5.0 | 3.2-3.4 | 2.9-3.1 | ≤2.8 |
| 5.1-5.3 | 5.4-5.9 | ≥6.0 | ||
| Electrocardiogram | Normal | Atrial fibrillation (rate 60-90) | Any other abnormal rhythm or ≥5 ectopics/min | |
| Q wave or ST/T wave changes | ||||
COPD, chronic obstructive pulmonary disease; POSSUM, Physiological and Operative Severity Score for enUmeration of Mortality and morbidity.
Supplementary Table 2. POSSUM Operative Severity Score.
| Score | ||||
|---|---|---|---|---|
| 1 | 2 | 4 | 8 | |
| Operative severity | Minor | Moderate | Major | Major+ |
| Multiple procedures | 1 | 2 | >2 | |
| Total blood loss, mL | ≤100 | 101-500 | 501-999 | ≥1000 |
| Peritoneal soiling | None | Minor, serous fluid | Local pus | Free bowel content, pus or blood |
| Presence of malignancy | None | Primary only | Nodal metastasis | Distant metastasis |
| Mode of surgery | Elective | Emergency resuscitation of >2 hrs possible | Emergency | |
| Operation <24 hrs after admission | Immediate surgery <2 hrs needed | |||
POSSUM, Physiological and Operative Severity Score for enUmeration of Mortality and morbidity.
References
- 1.Goswami S, Brady JE, Jordan DA, Li G. Intraoperative cardiac arrests in adults undergoing noncardiac surgery: incidence, risk factors, and survival outcome. Anesthesiology. 2012;117:1018–1026. doi: 10.1097/ALN.0b013e31827005e9. [DOI] [PubMed] [Google Scholar]
- 2.Sprung J, Warner ME, Contreras MG, Schroeder DR, Beighley CM, Wilson GA, et al. Predictors of survival following cardiac arrest in patients undergoing noncardiac surgery: a study of 518,294 patients at a tertiary referral center. Anesthesiology. 2003;99:259–269. doi: 10.1097/00000542-200308000-00006. [DOI] [PubMed] [Google Scholar]
- 3.Newland MC, Ellis SJ, Lydiatt CA, Peters KR, Tinker JH, Romberger DJ, et al. Anesthetic-related cardiac arrest and its mortality: a report covering 72,959 anesthetics over 10 years from a US teaching hospital. Anesthesiology. 2002;97:108–115. doi: 10.1097/00000542-200207000-00016. [DOI] [PubMed] [Google Scholar]
- 4.Ramachandran SK, Mhyre J, Kheterpal S, Christensen RE, Tallman K, Morris M, et al. Predictors of survival from perioperative cardiopulmonary arrests: a retrospective analysis of 2,524 events from the Get With The Guidelines-Resuscitation registry. Anesthesiology. 2013;119:1322–1339. doi: 10.1097/ALN.0b013e318289bafe. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chan PS, Spertus JA, Krumholz HM, Berg RA, Li Y, Sasson C, et al. A validated prediction tool for initial survivors of in-hospital cardiac arrest. Arch Intern Med. 2012;172:947–953. doi: 10.1001/archinternmed.2012.2050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Aschauer S, Dorffner G, Sterz F, Erdogmus A, Laggner A. A prediction tool for initial out-of-hospital cardiac arrest survivors. Resuscitation. 2014;85:1225–1231. doi: 10.1016/j.resuscitation.2014.06.007. [DOI] [PubMed] [Google Scholar]
- 7.Poldermans D, Bax JJ, Boersma E, De Hert S, Eeckhout E, Fowkes G, et al. Guidelines for pre-operative cardiac risk assessment and perioperative cardiac management in non-cardiac surgery: the Task Force for Preoperative Cardiac Risk Assessment and Perioperative Cardiac Management in Non-cardiac Surgery of the European Society of Cardiology (ESC) and endorsed by the European Society of Anaesthesiology (ESA) Eur J Anaesthesiol. 2010;27:92–137. doi: 10.1097/EJA.0b013e328334c017. [DOI] [PubMed] [Google Scholar]
- 8.Copeland GP, Jones D, Walters M. POSSUM: a scoring system for surgical audit. Br J Surg. 1991;78:355–360. doi: 10.1002/bjs.1800780327. [DOI] [PubMed] [Google Scholar]
- 9.Whiteley MS, Prytherch DR, Higgins B, Weaver PC, Prout WG. An evaluation of the POSSUM surgical scoring system. Br J Surg. 1996;83:812–815. doi: 10.1002/bjs.1800830628. [DOI] [PubMed] [Google Scholar]
- 10.Neary WD, Heather BP, Earnshaw JJ. The Physiological and Operative Severity Score for the enUmeration of Mortality and morbidity (POSSUM) Br J Surg. 2003;90:157–165. doi: 10.1002/bjs.4041. [DOI] [PubMed] [Google Scholar]
- 11.Wijesinghe LD, Mahmood T, Scott DJ, Berridge DC, Kent PJ, Kester RC. Comparison of POSSUM and the Portsmouth predictor equation for predicting death following vascular surgery. Br J Surg. 1998;85:209–212. doi: 10.1046/j.1365-2168.1998.00709.x. [DOI] [PubMed] [Google Scholar]
- 12.Chen T, Wang H, Wang H, Song Y, Li X, Wang J. POSSUM and P-POSSUM as predictors of postoperative morbidity and mortality in patients undergoing hepato-biliary-pancreatic surgery: a metaanalysis. Ann Surg Oncol. 2013;20:2501–2510. doi: 10.1245/s10434-013-2893-x. [DOI] [PubMed] [Google Scholar]
- 13.Dutta S, Horgan PG, McMillan DC. POSSUM and its related models as predictors of postoperative mortality and morbidity in patients undergoing surgery for gastro-oesophageal cancer: a systematic review. World J Surg. 2010;34:2076–2082. doi: 10.1007/s00268-010-0685-z. [DOI] [PubMed] [Google Scholar]
- 14.Hobson SA, Sutton CD, Garcea G, Thomas WM. Prospective comparison of POSSUM and P-POSSUM with clinical assessment of mortality following emergency surgery. Acta Anaesthesiol Scand. 2007;51:94–100. doi: 10.1111/j.1399-6576.2006.01167.x. [DOI] [PubMed] [Google Scholar]
- 15.Mohil RS, Bhatnagar D, Bahadur L, Rajneesh, Dev DK, Magan M. POSSUM and P-POSSUM for risk-adjusted audit of patients undergoing emergency laparotomy. Br J Surg. 2004;91:500–503. doi: 10.1002/bjs.4465. [DOI] [PubMed] [Google Scholar]
- 16.Neary WD, Prytherch D, Foy C, Heather BP, Earnshaw JJ. Comparison of different methods of risk stratification in urgent and emergency surgery. Br J Surg. 2007;94:1300–1305. doi: 10.1002/bjs.5809. [DOI] [PubMed] [Google Scholar]
- 17.Parmar CD, Torella F. Prediction of major adverse cardiac events in vascular surgery: are cardiac risk scores of any practical value? Vasc Endovascular Surg. 2010;44:14–19. doi: 10.1177/1538574409349320. [DOI] [PubMed] [Google Scholar]
- 18.Donati A, Ruzzi M, Adrario E, Pelaia P, Coluzzi F, Gabbanelli V, et al. A new and feasible model for predicting operative risk. Br J Anaesth. 2004;93:393–399. doi: 10.1093/bja/aeh210. [DOI] [PubMed] [Google Scholar]
- 19.Ellis SJ, Newland MC, Simonson JA, Peters KR, Romberger DJ, Mercer DW, et al. Anesthesia-related cardiac arrest. Anesthesiology. 2014;120:829–838. doi: 10.1097/ALN.0000000000000153. [DOI] [PubMed] [Google Scholar]
- 20.Bennett-Guerrero E, Hyam JA, Shaefi S, Prytherch DR, Sutton GL, Weaver PC, et al. Comparison of P-POSSUM risk-adjusted mortality rates after surgery between patients in the USA and the UK. Br J Surg. 2003;90:1593–1598. doi: 10.1002/bjs.4347. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Table 1. POSSUM Physiological Score.
| Score | ||||
|---|---|---|---|---|
| 1 | 2 | 4 | 8 | |
| Age, yrs | ≤60 | 61-70 | ≥71 | |
| Cardiac signs (chest radiograph) | No failure | Diuretic, digoxin, antianginal, or hypertensive therapy | Peripheral edema; warfarin therapy | Raised jugular venous pressure |
| Borderline cardiomegaly | Cardiomegaly | |||
| Respiratory signs (chest radiograph) | No dyspnea | Dyspnea on exertion | Limiting dyspnea | Dyspnea at rest |
| Mild COPD | Moderate COPD | Fibrosis or consolidation | ||
| Systolic blood pressure, mm Hg | 110-130 | 131-170 | ≥170 | ≤89 |
| 100-109 | 90-99 | |||
| Pulse, beats/min | 50-80 | 81-100 | 101-120 | ≥121 |
| 40-49 | ≤39 | |||
| Glasgow coma scale | 15 | 12-14 | 9-11 | ≤8 |
| Hemoglobin, g/100 mL | 13-16 | 11.5-12.9 | 10.0-11.4 | ≤9.9 |
| 16.1-17.0 | 17.1-18.0 | ≥18.1 | ||
| White cell count, ×1012/L | 4-10 | 10.1-20.0 | ≥20.1 | |
| 3.1-4.0 | ≤3.0 | |||
| Urea, mmol/L | ≤7.5 | 7.6-10.0 | 10.1-15.0 | ≥15.1 |
| Sodium, mmol/L | ≥136 | 131-135 | 126-130 | ≤125 |
| Potassium, mmol/L | 3.5-5.0 | 3.2-3.4 | 2.9-3.1 | ≤2.8 |
| 5.1-5.3 | 5.4-5.9 | ≥6.0 | ||
| Electrocardiogram | Normal | Atrial fibrillation (rate 60-90) | Any other abnormal rhythm or ≥5 ectopics/min | |
| Q wave or ST/T wave changes | ||||
COPD, chronic obstructive pulmonary disease; POSSUM, Physiological and Operative Severity Score for enUmeration of Mortality and morbidity.
Supplementary Table 2. POSSUM Operative Severity Score.
| Score | ||||
|---|---|---|---|---|
| 1 | 2 | 4 | 8 | |
| Operative severity | Minor | Moderate | Major | Major+ |
| Multiple procedures | 1 | 2 | >2 | |
| Total blood loss, mL | ≤100 | 101-500 | 501-999 | ≥1000 |
| Peritoneal soiling | None | Minor, serous fluid | Local pus | Free bowel content, pus or blood |
| Presence of malignancy | None | Primary only | Nodal metastasis | Distant metastasis |
| Mode of surgery | Elective | Emergency resuscitation of >2 hrs possible | Emergency | |
| Operation <24 hrs after admission | Immediate surgery <2 hrs needed | |||
POSSUM, Physiological and Operative Severity Score for enUmeration of Mortality and morbidity.