Abstract
Badminton is a famous sport usually played without any protective eyewear. Ocular injury from one's own partner in a doubles game, with the shuttlecock, is rare. Two untrained badminton players presented with severe ocular trauma during a smash shot from the partner in a ‘doubles’ game. Both the players developed blind eye (vision <3/60) in spite of immediate treatment. This article describes an unusual mode of severe blunt trauma with a shuttlecock while playing a ‘doubles’ game, leading to coup-countercoup injury. In addition, the article highlights the need for awareness of the fatal ocular complications and life-long visual disability, especially in untrained badminton enthusiasts.
Background
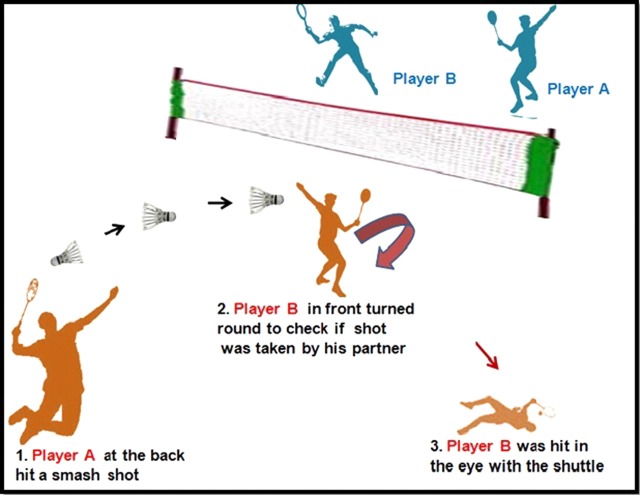
Badminton is a popular sport played by all age groups and socioeconomic segments. Shuttlecocks in badminton have been shown to be responsible for a high number of outpatient ocular sports-related injuries.1 Ocular trauma while returning the opponent's smash shot at the net is the most commonly reported mechanism of shuttlecock associated injury.2 A rare mechanism of eye injury is likely in ‘doubles’ during a smash shot from the player standing behind, to his partner standing in front by the net, who turns around to look at him (figure 1). A search of the literature produced the evidence of only one such case being reported so far.3 We report two incidental cases in different age groups, who were referred to us in a span of 6 months with this unusual mode of injury. Hence, the ‘not so common’ mechanism might be under-reported. Both the cases were playing badminton without the supervision of a coach. This highlights the role of proper training and awareness regarding serious ocular injury and its prevention in badminton players.
Figure 1.
Pictorial representation of an unusual mechanism of ocular trauma in badminton.
Case presentation
Case 1
A 55-year-old male badminton player with no history of ocular disease reported to our emergency department with blunt trauma to his right eye. He was injured by a shot from his doubles partner while playing badminton, in the manner described above. He presented with sudden onset severe pain in the right eye along with redness, watering, headache and diminution of vision. Ocular examination on the day of injury demonstrated a visual acuity of perception of light and accurate projection of rays in the right eye. Slit lamp examination (SLE) of the right eye revealed upper-lid and lower-lid oedema, conjunctival congestion and corneal stromal oedema with multiple descemet membrane folds. Anterior chamber (AC) showed cells (4+) and flare. It was deep and demonstrated vitreous and blood clots. There was iris sphincter tear at 11 o'clock position. Iridodialysis was noted from 10 to 11 o'clock position. The pupil was irregular, semidilated and not reacting to light. Reverse relative afferent pupillary defect (RAPD) was absent. Lens showed phacodonesis and subluxation from the 10 to 2 o'clock position (figure 2A). Applanation tonometry revealed a pressure of 4 mm Hg in the right eye. Extraocular movements were full in all directions and orbital margins were found to be normal. Fundus examination was difficult due to corneal oedema and vitreous haemorrhage (2+). Gonioscopy was deferred for 2 weeks. The left eye was normal. The injury was classified as closed globe injury, contusion type, grade 4, involving zones 1, 2 and 3 and RAPD negative according to the classification of the ocular trauma classification group.4
Figure 2.

(A) Anterior segment photograph taken within few hours of injury in Case 1 showing cilliary congestion, corneal stromal oedema (3+) with vitreous and blood clot in the anterior chamber. (B) Anterior segment photograph taken after clearing of corneal oedema showing subluxation of lens superiorly and blood clot in anterior chamber.
B-scan ultrasonography (7.5 MHz) of right eye showed vitreous haemorrhage and minimal choroidal effusion. There was no retinal detachment (figure 3).
Figure 3.

B scan ultrasound of right eye in Case 1, showing subluxated lens, vitreous haemorrhage and choroidal effusion. There is no retinal detachment.
The right eye was initially treated with cycloplegic eye drops, topical and oral steroids and antibiotic ointment. The patient was re-examined after 2 weeks. His vision was perception of light (PL) and projection of rays (PR) accurate. SLE showed no lid oedema, conjunctival congestion was minimal, corneal was clear without stromal oedema, AC was deep, pupil was semidilated and sluggishly reacting to light. The AC reaction was 1+ with minimal flare. The lens showed posterior and inferior subluxation with traumatic cataract. There was phacodonesis and a small blood clot mixed with vitreous in front of the lens (figure 2B). His intraocular pressure (IOP) was 12 mm Hg. Fundus examination was difficult due to vitreous haemorrhage .B scan ultrasonography revealed the presence of low reflective intragel echoes suggestive of vitreous haemorrhage with posterior vitreous detachment. There was no retinal detachment. Ultrasound biomicroscopy revealed a cyclodialysis cleft from 8 and 3 o'clock position which was wider between the 9 and 12 o'clock position. Thus, the patient had traumatic subluxation of lens with iridodialysis, vitreous haemorrhage and cyclodialysis cleft.
Thus, after the control of initial inflammation with medical line of therapy, pars plana vitrectomy with lensectomy and scleral fixated intraocular lens (SF IOL) was done in right eye after 2 weeks of injury. Scleral buckling with trans-scleral cryo application was also done in the same sitting. Postoperatively he was treated with topical cycloplegic and steroid—antibiotic eye drops which were tapered over 8 weeks.
The patient was under close follow-up after surgery. His best-corrected visual acuity was counting fingers at 1 ft with intraocular pressure of 14 mm Hg at the end of 1 year. He had good eyeball integrity and well-centred SF IOL. Media was clear with no evidence of retinal detachment. There were subretinal pigmentary changes in the macula.
Case 2
A 21-year-old female badminton player was struck on the left eye with a shuttlecock by the same mechanism as described in Case 1. She was referred to our hospital for management of secondary glaucoma after 6 weeks of injury. She had a history of sudden onset of painful diminution of vision in the left eye after shuttlecock injury. On the day of injury, her visual acuity was reduced to perception of light and projection of rays. She had conjunctival and cilliary congestion with grade 4 hyphema. Her intraocular pressure was noted to be greater than 60 mm Hg for which she was treated by a private practitioner. She was advised bed rest with no strenuous activity. She was treated with topical steroids (prednisolone acetate 1% eye drops, eight times per day) cycloplegic (1% Atropine drops, three times a day) and antiglaucoma (Timolol 0.5%, twice a day) medications. On the day of the injury she was given hyperosmotic agent (IV Mannitol, 20% in the dose of 1–2 g/kg intravenous over 45 min) and oral carbonic anhydrase inhibitor (tablet Acetazolamide 250 mg twice a day). Her laboratory test results were normal and there was no evidence of sickle-cell disease or any clotting disorder. She was re-examined by the same consultant on day 3. Her visual acuity and anterior segment findings were the same. As her IOP remained high (>60 mm Hg) in spite of the above treatment, an AC wash was done on day 3 of injury after administration of IV Mannitol. Subsequently, systemic steroids were added in tapering doses. She was under close monitoring for control of IOP after AC wash but her IOP remained constantly high (40–50 mm Hg), in spite of the above treatment for 6 weeks postsurgery (AC wash) she was referred to our hospital for further management.
We performed a detailed eye examination of this case. Her visual acuity in the left eye was counting fingers at 3 ft on presentation. SLE showed pigment deposition on the corneal endothelium, deep AC, a mid-dilated pupil, atrophic patches on the iris with multiple sphincter tears and posterior subcapsular cataract (figure 4). Reverse RAPD was absent. Gonioscopy demonstrated more than 180° angle recession with pigments (3+) in the inferior angle. There were no peripheral anterior synechiae. The right eye was normal.
Figure 4.
Anterior segment photograph taken 8 weeks following injury in Case 2 showing mid-dilated pupil, iris atrophic patches, multiple sphincter tears and posterior subcapsular cataract.
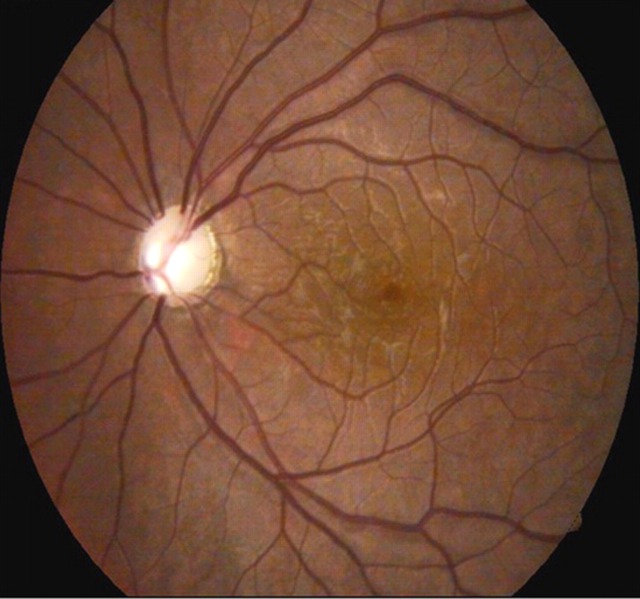
Fundus examination of the left eye showed a normal size optic disc with cup: disc ratio of 0.9 and thinning of the neuro-retinal rim suggestive of advanced glaucomatous cupping. There was resolving Berlin's oedema in the macular region (figure 5). Hence, she was classified as closed globe injury, contusion type, grade 4, zones 1, 2 and 3 and RAPD negative.4
Figure 5.
Fundus photograph of left eye in Case 2, showing advanced glaucomatous cupping with pallor and resolving Berlin's oedema.
Thus, Case 2 had secondary glaucoma with traumatic cataract and resolving macular oedema in the left eye.
She was treated with Mitomycin C augmented phaco-trabeculectomy and foldable intraocular lens implantation. Postoperatively she was treated with tapering doses of topical steroids, antibiotics, cycloplegic and antiglaucoma medications over 6 weeks.
She was under close observation postoperatively. At 1 year follow-up her best-corrected visual acuity was counting fingers at 6 ft with intraocular pressure of 12 mm Hg without antiglaucoma medications. She had good diffuse bleb with posterior chamber intraocular lens.
Outcome and follow-up
Case 1: Best-corrected visual acuity was counting fingers at 1 ft with intraocular pressure of 14 mm Hg at the end of 1 year. He had good eyeball integrity and well-centred SF IOL. Media was clear with no evidence of retinal tear or detachment. There were subretinal pigmentary changes in the macula.
Case 2: At 1 year follow-up her best-corrected visual acuity was counting fingers at 6 ft with intraocular pressure of 12 mm Hg without anti-glaucoma medications. She had good diffuse bleb with posterior chamber intraocular lens.
Discussion
Non-penetrating ocular injuries can result in severe ocular damage and significant loss of vision. Around 25–40% of patients being admitted to hospital with ocular trauma have sports-related injury.5 Barr et al6 reported 12.5% of ocular trauma from all causes to sports. A total of 14.3% of sports-related injuries can be attributed to badminton.7 Shuttlecock and racquet are responsible for 6 and 7% of badminton-related ocular injuries, respectively.3 A doubles game is shown to be associated with more injuries than a singles game.7 Shuttlecocks can attain extreme velocities during its projectile trajectory with the current advances in the racquet technology. Injury with a shuttlecock can lead to significant damage to the ocular structures as compared with tennis ball owing to the small size of the base of the shuttlecock and its hard nature which leads to direct impact on the unprotected eyeball. The different mechanisms of injuries associated with badminton are, injury due to: (1) a smash shot from opponent with player at the net, (2) shuttle glancing off the player's own racquet and hitting the eye, (3) racquet of doubles partner hitting the player and (4) an uncommon mechanism due to shuttle injury during a smash shot from the doubles partner when the player turns around to look at the miss-hit shot.3 The impact of shuttle depends on the distance of the player from the other player hitting the shot.
Owing to the small distance between the two partners, the shuttle strikes the eye with a great velocity culminating in severe ocular trauma. This mechanism of injury highlights the importance of facing the net and not turning the face around to check if the partner has taken the shot. The coaches and players need to be aware of this risk during competitive ‘doubles’ sports. The use of spectacles is associated with increased frequency of injury related to glass shattering. Hence, glass spectacles are dangerous and should never be worn by sportsmen. If refractive correction must be worn then it should ideally be incorporated into polycarbonate protective spectacles.8
A variety of injuries can occur because of momentary anatomical deformation of the globe by blunt trauma. As the cornea and sclera are suddenly compressed at the site of impact, a compensatory expansion occurs at the equator of the eye. We reported immediate consequences of blunt trauma like hyphema, traumatic cataract, cyclodialysis, iridodialysis, sphincter tears, subluxation of lens, vitreous haemorrhage and Berlins oedema in our case series. Some of the late onset complications of closed globe injuries are cystoid macular oedema, retinal detachment, optic atrophy, pigmentary changes in macula and angle recession glaucoma. Retinal detachments after blunt trauma may present late and is associated with retinal breaks because of secondary changes in the vitreous gel (vitreous liquefaction with posterior vitreous separation) causing vitreo-retinal traction.9 Severe contusion from blunt ocular trauma can result in Sphincter tear, subluxation of lens, cyclodialysis clefts and hypotony.10 Hypotony (IOP<5 mm Hg) and choroidal effusion after injury may be due to cilliary body shutdown and severe inflammatory reaction as in Case 1 which resolved after the use of topical steroids and cycloplegics. In a study by Chandran et al,11 shuttlecock injuries have been shown to account for 53.3% of hyphemas from all causes. A total of 27% of such patients develop impaired vision of 6/60 or less due to macular oedema, traumatic cataract or glaucoma.11 We also reported hyphema and early post-traumatic glaucoma leading to significant loss of vision possibly due to iritis and trabeculitis in our second case.
The management of trauma cases involving anterior and posterior segment is critical. Case 1 had vitreous strands in front of lens and vitreous haemorrhage in posterior segment for which vitrectomy was performed. There was traumatic cataract and the lens was subluxated inferiorly which was managed by lensectomy and SF IOL after control of inflammation. The above procedures were combined with scleral buckling and cryo to prevent risk of late onset retinal detachment and iatrogenic postoperative sclerotomy-related complications, respectively.10 The decision of doing multiple surgeries in same sitting was taken due to absence of inflammatory reaction, clear cornea, stable IOP, availability of high-quality vitreo-retinal set-up and experienced surgeon. Doing multiple procedures in the same sitting carries a small risk of postoperative complications such as bleeding and infection but in competent hands it lessens the psychological stress of undergoing several ocular surgeries and reduces hospital stay and economical burden on the patient.
The surgical management of second case was by Mitomycin augmented trabeculectomy and implantation of posterior chamber IOL as patient had secondary glaucoma and traumatic cataract.
Both the patients developed blind eye due to severe sports-related blunt injury (V/A<3/60). Macewan et al12 reported majority of serious eye injuries to be due to sporting or leisure activities. More than 90% of sports-related injury is preventable.8 13
Prospect for prevention of sports-related trauma can be addressed with vigorous education among the players, coaches and parents. The Ontario Badminton Association (OBA) has made the use of special eye protectors (manufactured according to American Society for Testing and Materials F803 specifications) mandatory for all junior racquet players in OBA-sanctioned tournament. Taking cue from the OBA, eye protectors should be made compulsory for racquet sports players all over the world.14–16
The Protective Eyewear Promotion (PEP) model should be adopted for all badminton players. The model recommends appropriate education of the players with respect to protective eyewear, tailoring the advice for each individual player, making the eyewear more available to them and providing incentives for using protective eyewear to potentiate safe-behaviour.17 18 This model has been shown to reduce the risk of eye injury in squash players.19
Prevention is the best option for management and it has been suggested that more than 90% of sports-associated eye injuries can be avoided.5 Even with advanced microsurgical treatment, the result of severe eye injuries is usually unsatisfactory.
Learning points.
Shuttlecock injuries can be serious and sight threatening.
Untrained badminton enthusiasts should be educated about the mechanisms and fatal consequences of ocular trauma due to this sport.
Severe closed injuries, especially those involving the posterior segment, may cause permanent visual impairment.
Both the patients developed blind eye due to severe blunt injury (V/A<3/60).
Footnotes
Competing interests: None.
Patient consent: Obtained.
References
- 1.Barrell GV, Cooper PJ, Elkington AR, et al. Squash ball to eye ball: the likelihood of squash players incurring an eye injury. BMJ (Clin Res Ed) 1981;283:893–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hensley LD, Paup DC. A survey of badminton injuries. Br J Sports Med 1979;13:156–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kelly SP. Serious eye injury in badminton players. Br J Ophthalmol 1987;71:746–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pieramici DJ, Sternberg P, Jr, Aaberg TM, Sr, et al. Ocular trauma classification group. A system for classifying mechanical injuries of the eye (globe). Am J Ophthalmol 1997;123:820–31. [DOI] [PubMed] [Google Scholar]
- 5.MacEwen CJ, McLatchie GR. Eye injuries in sport. Scott Med J 2010;55:22–4. [DOI] [PubMed] [Google Scholar]
- 6.Barr A, Baines PS, Desai P, et al. Ocular sports injuries: the current picture. Br J Sports Med 2000;34:456–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jones NP. Eye Injuries in sport: an increasing problem. Br J Sports Med 1987;21:168–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cass SP. Ocular injuries in sports. Curr Sports Med Rep 2010;11:11–15. [DOI] [PubMed] [Google Scholar]
- 9.Rouberol F, Denis P, Romanet JP, et al. Comparative study of 50 early- or late-onset retinal detachments after open or closed globe injury. Retina 2011;31:1143–9. [DOI] [PubMed] [Google Scholar]
- 10.Alexander S. Ioannidis and Keith Barton. Cyclodialysis cleft: causes and repair. Curr Opin Ophthalmol 2010;21:150–4. [DOI] [PubMed] [Google Scholar]
- 11.Chandran S. Ocular hazards of playing badminton. Br J Ophthalmol 1974;58:757–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Macewan CJ. Eye injuries: a prospective survey of 5671 cases. Br J Ophthalmol 1989;73:888–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Goldstein MH, Wee D. Sports injuries: an ounce of prevention and a pound of cure. Eye Contact Lens 2011;37:160–3. [DOI] [PubMed] [Google Scholar]
- 14. Ontario Badminton Association guidelines: OBA (Web site) http://www.kiernander.com/badminton/eye_injuries_and_protective_eyewear_for_badminton.html.
- 15.ASTM Standard specification for eye protectors for selected sports. ASTM F803. West Conshohocken, PA: American Society for Testing and Materials, 2003. [Google Scholar]
- 16.ANSI American National Standard Practice for Occupational and Educational Personal Eye and Face Protective Devices. ANSI Z87.1– 2003 . New York: American National Standards Institute Inc, 2003. [Google Scholar]
- 17.Eime R, Owen N, Fnch C. Protective eyewear promotion: applying principles of behaviour change in the design of squash injury prevention programme. Sports Med 2004;34:629–38. [DOI] [PubMed] [Google Scholar]
- 18.McLean CP, DiLillo D, Bornstein BH, et al. Predictors of goggle use among racquetball players. Int J Inj Contr Saf Promot 2008;15:167–70. [DOI] [PubMed] [Google Scholar]
- 19.Eime R, Finch C, Wolfe R, et al. The effectiveness of squash eyewear promotion strategy. Br J Sports Med 2005;39:681–5. [DOI] [PMC free article] [PubMed] [Google Scholar]