Description
A previously healthy 82-year-old lady presented with abnormal sensation in her fingers which she described as ‘feeling like bananas’. There was an additional history of deteriorating handwriting and a sense of imbalance when walking dating back 6 months. She obtained a score of 26 out of 30 on the mini mental state examination. She had gait ataxia, being unable to perform tandem gait. There was no convincing pseudoathetosis of the outstretched hands. She had slow, clumsy fine finger movements and her diary entries had become progressively illegible. Proprioception was abnormal in the toes and vibration sense was lost to the level of the costal margins. Reflexes were brisk in the arms but depressed in the legs. Plantar responses were flexor. Her serum vitamin B12 level was 83 (160–800) ng/l. Intrinsic factor antibodies were negative. Parietal cell antibodies were positive. Zinc and copper studies were satisfactory. Brain MRI revealed some cerebral atrophy and evidence of small vessel disease. Whole spine MRI revealed high-signal change in the dorsal columns, particularly in the cervical and upper thoracic cord (figures 1 and 2). There was an improvement in handwriting and gait following treatment.
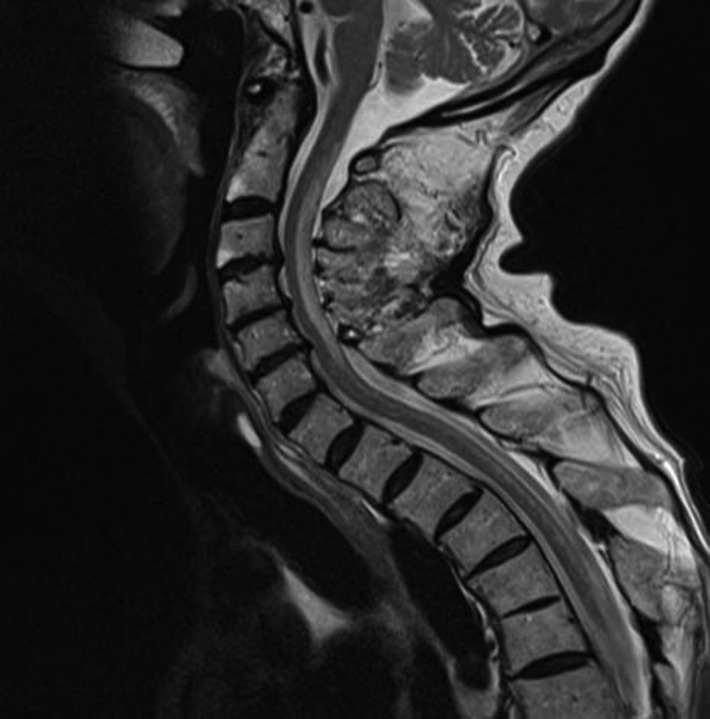
Figure 1.
Sagittal section of T2-weighted MRI of the cervical spine, showing patchy high-signal intensity in the posterior spinal cord, seen clearly extending from the C2 to C6 vertebrae.
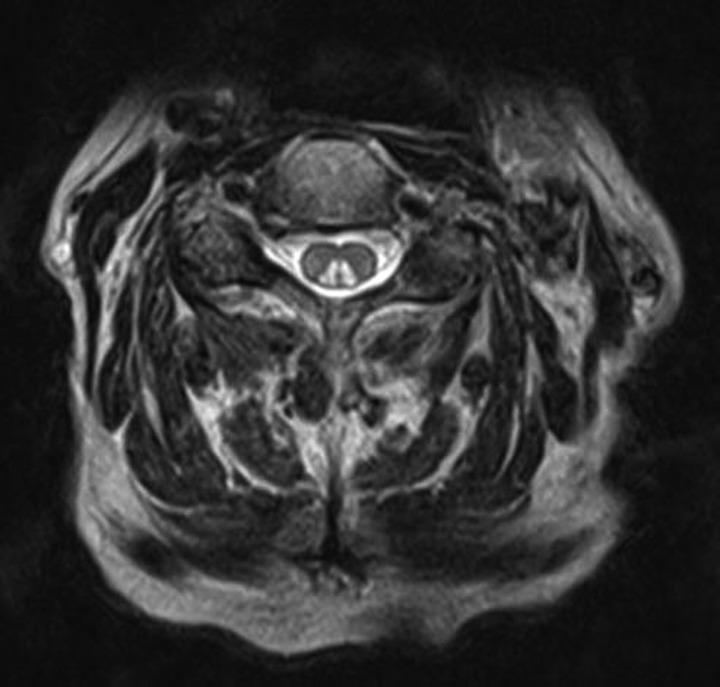
Figure 2.
Axial section of T2-weighted MRI of the cervical spine, demonstrating symmetrical high-signal intensity in the dorsal columns of the spinal cord.
Recognising subacute combined degeneration of the spinal cord due to vitamin B12 deficiency is an important treatable cause of progressive neurological disability. Symptom onset is often with a vague sensation of weakness and parasthaesia. The ‘pins and needles’ usually involve the hands more than the feet and tend to be progressive. As the illness progresses, an ataxic paraplegia develops.1 There may be additional affective/behavioural or cognitive changes and in a subgroup of patients, these symptoms may precede any cord symptoms.2 The initial neurological examination may be normal. Later, examination is consistent with a disorder of the dorsal and lateral columns of the spinal cord with loss of vibration sense and impaired proprioception being the most reliable signs.
The diagnosis is confirmed by means of blood tests that show a low serum vitamin B12 level and MRI of the spinal cord. Interestingly, there may not be a macrocytic anaemia and it is thought that the degree of anaemia may correlate inversely with any neurological signs and symptoms.2 A normal vitamin B12 level should raise the possibility of copper deficiency.3
Early replenishment of vitamin B12 body stores is associated with a better prognosis and reduces the likelihood of long-term residual disability.2 Many neurologists would treat immediately after taking a blood sample, that is, before the results became available, if the clinical diagnosis was suspected.
Acknowledgments
The authors wish to thank Dr Fatemeh Geranmayeh, Specialist Registrar in Neurology and Dr Sheldon Zheng, Foundation Year 1 doctor.
Footnotes
Competing interests: None.
Patient consent: Obtained.
References
- 1.Savage DG, Lindenbaum J. Neurological complications of acquired cobalamin deficiency: clinical aspects. Baillieres Clin Haematol 1995;8:657–78. [DOI] [PubMed] [Google Scholar]
- 2.Reynolds E. Vitamin B12, folic acid, and the nervous system. Lancet Neurology 2006;5:949–60. [DOI] [PubMed] [Google Scholar]
- 3.Jaiser SR, Winston GP. Copper deficiency myelopathy. J Neurol 2010;257:869–81. [DOI] [PMC free article] [PubMed] [Google Scholar]