Abstract
Purpose
We sought to determine whether a regimen of 70% ethanol locks could reduce the rate of central venous catheter (CVC) infections in parenteral nutrition-dependent children with intestinal failure.
Methods
We performed a retrospective review of 23 parenteral nutrition-dependent children in our multidisciplinary intestinal rehabilitation clinic who started ethanol lock therapy between September 2007 and June 2009. The treatment regimen consisted of a 70% ethanol lock instilled 3 times per week in each catheter lumen. The rate of CVC infections before and after initiation of ethanol lock therapy was compared using the Wilcoxon signed ranks test with significance set at P < .05.
Results
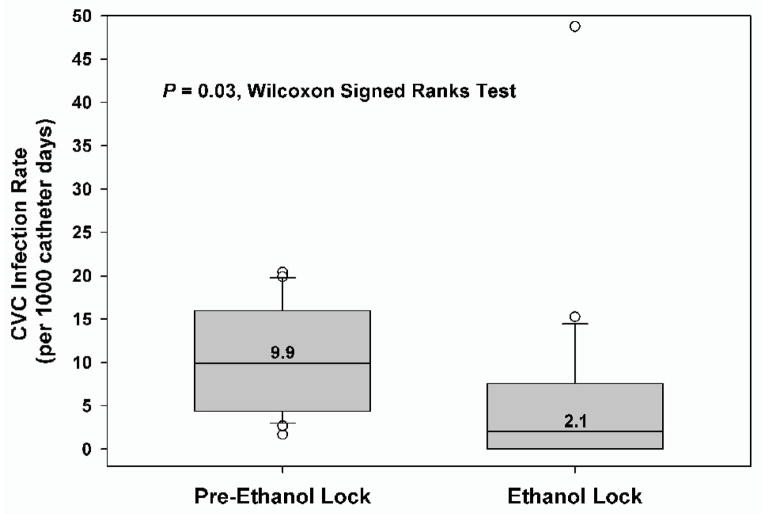
The most common diagnoses leading to intestinal failure were necrotizing enterocolitis (26.1%), gastroschisis (21.7%), and intestinal atresia (14.3%). Ethanol locks were well tolerated with no reported adverse side effects. The infection rate decreased from 9.9 per 1000 catheter days prior to initiation of ethanol locks to 2.1 per 1000 catheter days during therapy (P = .03).
Conclusions
A regimen of ethanol lock therapy administered three days per week appears to be a safe and effective means of reducing the rate of CVC infections in parenteral nutrition-dependent children with intestinal failure.
Keywords: Intestinal Failure, Ethanol locks, Catheter-related sepsis, Central Venous Catheter Infection
Purpose
Central venous catheter (CVC) infections are a major source of morbidity and mortality for children with intestinal failure. Parenteral nutrition (PN) remains a mainstay of therapy in the care of children with intestinal failure, and in these patients central venous catheters are a lifeline. Previously published reports have shown rates of catheter-related infections in children with intestinal failure ranging from 11.15 to 26.5 infections per 1000 catheter days [1, 2]. Although multidisciplinary management of intestinal failure can reduce the use of PN [3, 4], a substantial number of patients with indwelling central venous catheters continue to be develop line sepsis. Catheter associated sepsis can lead to line removal, loss of access sites, accelerated hepatic damage, hospitalization, and increased mortality.
Methods to reduce the number of infections in central venous catheters have become standard of care. These include insertion under sterile conditions, maintenance of sterile occlusive dressings, and close surveillance for signs of infections [5]. Antibiotic catheter lock solutions have also been shown to be effective in reducing catheter related bloodstream infections (CRBSI) in pediatric patients [6]. Concerns about the use of antibiotic lock therapy include the development of resistant bacteria strains, as well as hypersensitivity to or toxicity from the antibiotics themselves [5]. In many instances, the antibiotic-heparin combination has limited physicochemical stability which makes it impractical for homecare patients. In addition, the biofilm formed by bacteria on an indwelling catheter confers its own inherent resistance [7]. To penetrate the biofilm, antibiotic concentrations 20–1000 times stronger than those typically required to produce the same killing effect on planktonic, or free-floating, bacteria are required [7]. Recent studies of various catheter lock solutions led to the discovery of ethanol as an effective antibacterial agent [8, 9].
Ethanol acts as a bactericidal and fungicidal agent by denaturing the cell membrane. Its wide spectrum of antimicrobial action has led to diverse uses, such as mouthwashes, hand washes, and hospital disinfectants [10]. A 4 hour exposure to a concentration of 70% ethanol has been shown to be both bactericidal and fungicidal to Staphylococcus aureus, Streptococcus pyogenes, Escherichia coli, Pseudomonas aeruginosa, Klebsiella pneumonia, and Candida albicans in an experimental model of plastic-adherent biofilm [11]. Ethanol has the ability to penetrate the protective biofilm, and has not been shown to pose a risk for development of resistance [12].
We recognized the potential for a reduction in catheter-related sepsis in our pediatric intestinal failure patients, and instituted an outpatient regimen of ethanol locks. Our study aim was to assess if this intervention did indeed decrease the rate of central venous catheter infections in parenteral nutrition-dependent children with intestinal failure.
Methods
Intestinal failure patients with a history of one or more central venous catheter (CVC) infections in the previous year were eligible for the ethanol lock protocol. A regimen of 70% ethanol catheter locks was instituted on an outpatient basis, beginning in September 2007. A 70% ethanol in water solution was prepared in the Children’s Hospital Boston Pharmacy by dilution of Dehydrated Alcohol Injection, USP, which consists of not less than 98% by volume of ethanol (ethyl alcohol). The volume of lock solution delivered was determined for each patient individually, based on the volume of the catheter. Catheter volume was determined by aspirating from the catheter until blood return was noted, and then using the volume of the aspirated fluid as the volume of the lock solution. For each patient, the first administration of the ethanol lock was done in a monitored inpatient setting. The ethanol lock solution was instilled into the catheter between infusions of parenteral nutrition (PN), and left in place for a minimum dwell time of 4 hours. At the start of the patient’s next administration of PN, the ethanol solution was withdrawn from the catheter and discarded. Once the patient’s caregivers were instructed in the administration of ethanol locks, this process was executed three days per week on an outpatient basis, usually Monday, Wednesday, and Friday. All patients and their caregivers were questioned regarding tolerance of the ethanol locks as well as possible adverse events during outpatient clinic visits, which occurred at least every 3 months during the study period.
All patients included in this study were followed by the Center for Advanced Intestinal Rehabilitation (CAIR) at Children’s Hospital Boston. This is a multidisciplinary team of pediatric surgeons, gastroenterologists, nurses, pharmacists, dieticians, and social workers who specialize in the management of children with intestinal failure. This study was conducted as a retrospective review of patients” medical records under the direction of Children’s Hospital Boston Investigational Review Board protocol M06-01-0049.
Criteria for inclusion in this study included the presence of a silicone tunneled central venous catheter or silicone Peripherally Inserted Central Catheter (PICC) for administration of PN or intravenous hydration fluids to treat intestinal failure. All patients were 3 months to 18 years old and weighed at least 5 kilograms. All patients had at least one CVC infection in the previous year. Ethanol locks were stopped during any treatment intervals with metronidazole, due to possible disulfiram-like reactions. In addition, ethanol locks were withheld during any inpatient admission. Documented allergies to ethanol or social or religious objections to the use of ethanol were additional criteria for exclusion from ethanol lock therapy.
Demographic data collected included the following; gender, patient age at the initiation of ethanol locks, primary diagnosis leading to intestinal failure, and serum citrulline level. Dates of catheter placement and removal were also recorded. A catheter change was defined as a confirmed removal of one catheter and replacement by another. Infection data reviewed included the number of positive blood cultures isolated from the central venous catheter, and the organisms grown from those blood cultures. Central venous catheter infection was defined as at least one positive blood culture from the CVC in the absence of another confirmed source of infection such as a positive urine or sputum culture.
Statistical analysis was done using the Statistical Package for Social Sciences (SPSS for Windows, SPSS Inc., Chicago, IL). CVC infection rates were expressed as number of infections per 1000 catheter days. Each patient was used as his own control, and rates of catheter infections pre-and post-ethanol lock therapy initiation were compared. Age, number of catheter days, and catheter infection rates were expressed as medians with interquartile ranges. The Wilcoxon signed ranks test was used to compare paired non-parametric data. The sign test was used to compare rate changes in non-parametric data. Significance was set at P < .05.
Results
A total of 31 patients started ethanol lock therapy between September 2007 and June 2009. Eight patients were excluded from analysis (2 patients left the country and were lost to follow-up, 3 patients did not meet inclusion criteria, and 3 patients were primarily managed at other institutions and did not have complete infection data). Demographic information from the 23 analyzed patients is shown in Table 1. Patients with potential motility disorders (including gastroschisis, pseudoobstruction, intestinal aganglionosis, and anal achalasia) accounted for 47.8% of all patients on ethanol lock therapy. The majority of patients had severe short bowel syndrome, with a mean serum citrulline (an index of intestinal mucosal mass) of 10.4 +/− 6.3 μmol/L [13].
Table 1.
Demographic data of the 23 patients receiving ethanol lock therapy
| Characteristic | |
|---|---|
| Median age at start of EtOH lock therapy | 18.3 mo (IQR, 11.2 – 31.4) |
| Sex | |
| Male | 16 (70%) |
| Female | 7 (30%) |
| Diagnosis | |
| Necrotizing enterocolitis | 6 (26%) |
| Gastroschisis | 5 (22%) |
| Intestinal atresias | 3 (13%) |
| Other a | 9 (39%) |
| Presence of motility disorder b | 11 (48%) |
| History of AIRS | 5 (22%) |
IQR indicates interquartile range; EtOH, ethanol; AIRS, autologous intestinal reconstruction surgery: serial transverse enteroplasty (4), longitudinal intestinal lengthening and tailoring (1).
Other diagnoses included: midgut volvulus, anal achalasia, intestinal pseudoobstruction, primary intestinal dysmotility disorder, intestinal aganglionosis, and microvillus inclusion disease.
Motility disorder included anal achalasia, intestinal aganglionosis, primary intestinal dysmotility disorder, and intestinal pseudoobstruction.
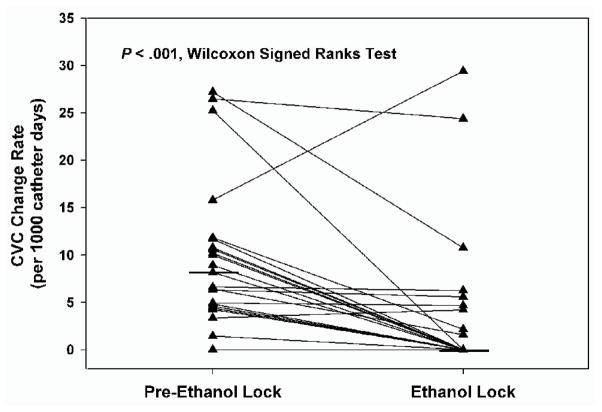
The rate of central venous catheter (CVC) infections and catheter changes (per 1000 catheter days) before and during ethanol lock therapy are shown in Table 2. The median rate of CVC infections prior to the initiation of ethanol lock therapy was 9.9 infections per 1000 catheter days (IQR 4.4, 17.3). After initiation of ethanol lock therapy, the median infection rate dropped to 2.1 infections per 1000 catheter days (IQR 0, 7.6). This statistically significant decrease (Wilcoxon signed ranks test, Z −2.159, P = .03) is shown in Figure 1. Eighteen of 23 patients had a decrease in their rate of CVC infections after the initiation of ethanol lock therapy. The median rate of CVC changes per 1000 catheter days also decreased significantly, from a median of 8.2 (IQR 4.6, 11.7) prior to initiation of ethanol locks to 0 (IQR 0, 4.7) while on ethanol lock therapy (Wilcoxon signed ranks test, Z −3.328, P < .001). Only 2 of the 23 patients had an increase in the rate of catheter changes after initiation of ethanol lock therapy, as shown in Figure 2.
Table 2.
Catheter days, CVC infection rates, and catheter change rates for study cohort of 23 patients before and after starting ethanol lock therapy
| Variable | Pre-EtOH lock therapy Median (IQR) |
EtOH lock therapy Median (IQR) |
P |
|---|---|---|---|
| Catheter days | 302 (207, 596) | 215 (41, 394) | .03 |
| CVC infection rate | 9.9 (4.4, 16.0) | 2.1 (0.0, 7.6) | .03 |
| Catheter change rate | 8.2 (4.6, 11.7) | 0.0 (0.0, 4.7) | <.001 |
CVC indicates central venous catheter; EtOH, ethanol; IQR, interquartile range. Infection and change rates were calculated per 1000 catheter days.
Figure 1.
Box plot showing decreased rate of central venous catheter (CVC) infections after starting ethanol lock therapy (median 9.9 versus 2.1 per 1000 catheter days, N = 23 patients). Grey boxes encompass interquartile ranges (IQR) and the median is shown as a horizontal line within each grey box. Whiskers represent 95% confidence intervals, and open circles indicate outliers. The difference in infection rates before and during ethanol locks was significant (Wilcoxon signed ranks test, Z −2.159, P = .03).
Figure 2.
Rate of CVC changes (per 1000 catheter days) prior to and after starting ethanol lock therapy. Black triangles and lines show CVC change rate for individual patients (N=23). Horizontal black lines indicate median rate of CVC changes. The rate of CVC changes was significantly reduced on ethanol lock therapy (Wilcoxon signed ranks test, Z −3.328, P < .001).
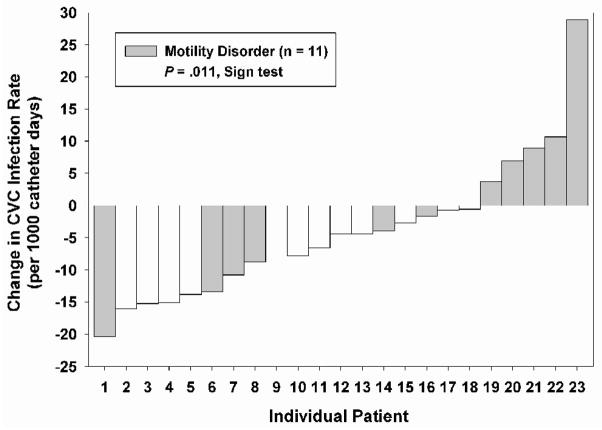
Subgroup analysis of patients with and without gastrointestinal motility disorders revealed that all five of the patients whose rate of CVC infections increased on ethanol lock therapy had an intestinal motility disorder (Figure 3). The change in CVC infection rate after starting ethanol lock therapy was significantly different for patients with and without motility disorders (Sign test, P = .011). After starting ethanol lock therapy, the cohort without a motility disorder had a drop in infection rate from a median of 9.9 per 1000 catheter days (IQR 4.8, 15.8) to a median of 0 per 1000 catheter days (IQR 0, 4.9). All patients without disordered motility had a decreased catheter infection rate on ethanol lock therapy. The cohort of children with motility disorders continued to have a high rate of infections (median 7.2 per 1000 catheter days, IQR 0, 13.3) after starting ethanol lock therapy, as shown in Table 3. The difference in infection rates before and after ethanol lock therapy in children with motility disorders was not significant (P = .79).
Figure 3.
Change in CVC infection rate after starting ethanol lock therapy for each of the 23 patients. Boxes below the X-axis indicate a decrease in CVC infection rate, while boxes above the X-axis represent an increase in CVC infection rate. Patients with motility disorders are shown in grey, while those without motility disorders are in white. 18 of 23 patients had a decrease in infection rate on ethanol lock therapy, while 5 of 23 patients had an increased infection rate. All patients with an increased rate of CVC infections had dysmotility disorders. The decrease in CVC infection rate after starting ethanol lock therapy was significantly greater for the cohort with normal motility (Sign test, P = .011).
Table 3.
CVC infection rates and catheter change rates for patients with (n = 11) and without (n = 12) motility disorders before and after starting ethanol lock therapy
| Variable | Pre-EtOH therapy Median (IQR) |
During EtOH therapy Median (IQR) |
P |
|---|---|---|---|
| CVC infection rate | |||
| Normal motility | 9.9 (4.8, 15.0) | 0.0 (0.0, 4.9) | .002 |
| Motility disorder | 4.6 (4.0, 17.8) | 7.2 (0.0, 13.3) | .79 |
| Catheter change rate | |||
| Normal motility | 6.5 (4.7, 10.3) | 0.0 (0.0, 1.2) | .003 |
| Motility disorder | 10.2 (4.3, 15.8) | 2.2 (0.0, 10.8) | .06 |
CVC indicates central venous catheter; EtOH, ethanol; IQR, interquartile range. Infection and change rates were calculated per 1000 catheter days.
The entire cohort of 23 patients had a total of 122 CVC infections for the duration of the study. 93 infections (76.2%) were due to a single organism; 29 (23.8%) were polymicrobial. The most frequently isolated organisms were Staphylococcus (25%), Klebsiella (35%), and Enterococcus (19%). A listing of the bacterial and fungal genera isolated from the CVC cultures is shown in Table 4.
Table 4.
Microorganisms identified in CVC infections of the 23 patients in the cohort
| Organism genus | Absolute number and percentage |
|---|---|
| Staphylococcus | 37 (25%) |
| Klebsiella | 35 (23%) |
| Enterococcus | 29 (19%) |
| Candida | 13 (9%) |
| Eschericia | 8 (5%) |
| Enterobacter | 6 (4%) |
| Streptococcus | 4 (3%) |
| Lactobacillus | 3 (2%) |
| Other a | 12 (8%) |
| Unspeciated gram negative rods | 2 (1%) |
| Type of infection | |
| Single organism | 93 (76%) |
| Polymicrobial | 29 (24%) |
CVC indicates central venous catheter.
Other organisms included: Rhodococcus, Gordonia, Corynebacterium, Clostridium, Actinomyces, Bacillus, Serratia, Bifidobacteria, Citrobacter, and Neisseria.
Potential adverse events including dizziness, lethargy or altered mental status, and intravenous catheter breakage were monitored during scheduled outpatient visits. There were no adverse events reported.
Discussion
While the multidisciplinary care of pediatric patients with intestinal failure continues to improve [4], central venous catheter (CVC) infections remain a major source of morbidity and mortality. In addition to the need for prolonged intravenous antibiotics and costly hospitalization related to the infection itself, recurrent CVC infections contribute directly to the progression of parenteral nutrition associated liver disease (PNALD) [14], and may lead to catheter removal and loss of venous access sites. These factors can lead to liver and intestinal transplantation [15], which in itself is associated with potential morbidity and mortality.
Sterile insertion technique and intensive family and caregiver education are cornerstones of CVC care in our multidisciplinary intestinal failure program. We began using a regimen of ethanol lock therapy in September 2007 with the goal of reducing the CVC infection rate in our highest risk patients – those with at least one prior CVC infection – as these children had the greatest potential benefit from this intervention. The initiation of ethanol lock therapy was the only change in our approach to CVC care during this time period.
The use of ethanol locks to treat CVC infections was first reported by Dannenberg in 2003 [16]. Their group used ethanol locks as an adjunct to standard treatment of catheter infections in pediatric hematology/oncology patients. In 2004, Metcalf reported the first use of ethanol locks in an adult on cyclic home PN [12]. This patient had 3 infection-free years after the initiation of ethanol locks. In 2008, Mouw reported the first use of ethanol locks in a group of pediatric intestinal failure patients with a favorable reduction in infection rates after the initiation of ethanol locks, though no statistical significance could be garnered from this study due to its small size. [2] The aforementioned studies, while small, suggested that ethanol lock therapy may be an important factor in reducing the risk of CVC infections.
In our study, the initiation of ethanol lock therapy significantly reduced the rate of CVC infections in our cohort, from a median of 9.9 infections per 1000 catheter days prior to ethanol locks to 2.1 infections per 1000 catheter days during ethanol lock therapy (P = .03). The median baseline infection rate of 9.9 per 1000 catheter days was comparable to other studies in similar patient populations [1, 2]. The almost five-fold reduction in catheter infection rates seen with ethanol lock therapy supports the clinical utility of this intervention.
In order to quantify the severity of intestinal failure in our patients, we examined serum citrulline levels. Citrulline concentrations have been shown to correlate with enterocyte mass, and are predictive of the ability of a patient to achieve enteral autonomy [13, 17]. The serum citrulline level of the patients in our cohort (mean ±S.D.) was 10.4±6.3 μmol/L. Earlier studies from our group have demonstrated that patients with serum citrulline level less than 12 μmol/L are unlikely to wean from parenteral nutrition [13], indicating that the study cohort of patients did have severe intestinal failure.
An unexpected finding was that the efficacy of ethanol lock therapy was affected by the presence or absence of diagnoses associated with intestinal motility disorders. Only 5 of the 23 patients had an increased rate of infection while on ethanol lock therapy, and all 5 of these patients had an intestinal motility disorder. The one patient who had a drastically increased rate of CVC infection had a short follow-up period (41 days) on ethanol lock therapy, and had 2 infections during that time interval. Subgroup analysis revealed that 100% of patients without disordered intestinal motility had a decreased rate of CVC infection on ethanol lock therapy, while only 55% of children with a motility disorder had a lower rate of CVC infection. The change in infection rates after starting ethanol lock therapy for those patients with intestinal motility disorders was not statistically significant.
Previous reports have shown that some children with chronic intestinal pseudoobstruction may have concomitant immune deficiencies, including IgG, natural killer cell, and other antibody deficiencies [18]. Since two of the patients in this study had a primary diagnosis of intestinal pseudoobstruction, it is possible that an immune deficiency contributed to the increased infection rate in these patients. In addition, we hypothesize that disordered intestinal motility in these patients led to increased intestinal bacterial overgrowth and translocation of gut flora, which then caused CVC infections.
The rate of CVC changes also decreased after starting ethanol lock therapy, from a median of 8.2 (IQR 4.6, 11.7) to 0 (IQR 0, 4.7) per 1000 catheter days (P < .001). Only 2 of 23 patients had a higher rate of CVC changes after starting ethanol locks. The preservation of catheters associated with ethanol lock therapy is important, as previous investigations have suggested that ethanol may decrease catheter durability [19]. It is evident that this factor, if present, did not affect the overall improvement in catheter longevity.
Previous studies have reported dyspnea, dizziness, nausea, and intravenous catheter breakage with embolism of catheter fragments associated with ethanol lock therapy [16, 20, 21]. There were no such reported complications in this cohort of 23 patients. Some studies that have reported dizziness and altered mental status in association with ethanol locks have flushed the solution through the lumen at the end of the dwell time, rather than withdrawing it. Intravenous catheter breakage with embolization of catheter fragments with ethanol lock therapy has been described with daily therapy and use of a catheter type other than silicone [22]. It is possible that we averted these complications by using a three day per week ethanol lock regimen, placing only silicone catheters, and withdrawing the ethanol solution at the end of the dwell time whenever possible. We also may have reduced problems by specifying a minimum patient weight of 5 kg, to ensure that if the ethanol lock was flushed intraluminally, the patient’s blood alcohol level would theoretically not exceed a level of 0.08%. To avoid possible disulfiram-like reactions, ethanol locks were withheld from patients who were being treated with metronidazole.
The limitations of this retrospective study are recognized. For instance, clinical variables such as the reasons for central line replacement were not uniformly documented. However its size (the largest pediatric intestinal failure cohort treated with ethanol locks reported) has allowed for some important analyses.
It is possible to conclude that ethanol lock therapy was associated with a statistically and clinically significant decrease in the rate of central venous catheter infections as well as reduced catheter replacements in a cohort of pediatric patients with severe intestinal failure. Additionally, adverse reactions to the ethanol lock therapy were not seen. Based on these results, we now utilize outpatient ethanol lock therapy in all of our pediatric intestinal failure patients with a history of central venous catheter infections. Subgroup analyses indicated that the benefits of ethanol lock therapy seemed greatest in children without intestinal motility disorders. We hypothesize that this difference was due to intestinal bacterial overgrowth leading to bacterial translocation in the patients with disordered motility. Overall, ethanol lock therapy appears to be of utility in reducing central venous catheter infections in pediatric patients with intestinal failure. Further prospective investigations are warranted.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Onder AM, Kato T, Simon N, et al. Prevention of catheter-related bacteremia in pediatric intestinal transplantation/short gut syndrome children with long-term central venous catheters. Pediatr Transplant. 2007;11:87–93. doi: 10.1111/j.1399-3046.2006.00634.x. [DOI] [PubMed] [Google Scholar]
- 2.Mouw E, Chessman K, Lesher A, et al. Use of an ethanol lock to prevent catheter-related infections in children with short bowel syndrome. J Pediatr Surg. 2008;43:1025–1029. doi: 10.1016/j.jpedsurg.2008.02.026. [DOI] [PubMed] [Google Scholar]
- 3.Sudan D, DiBaise J, Torres C, et al. A multidisciplinary approach to the treatment of intestinal failure. J Gastrointest Surg. 2005;9:165–176. doi: 10.1016/j.gassur.2004.10.014. discussion 176-167. [DOI] [PubMed] [Google Scholar]
- 4.Modi BP, Langer M, Ching YA, et al. Improved survival in a multidisciplinary short bowel syndrome program. J Pediatr Surg. 2008;43:20–24. doi: 10.1016/j.jpedsurg.2007.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.O’Grady NP, Alexander M, Dellinger EP, et al. Guidelines for the prevention of intravascular catheter-related infections. Centers for Disease Control and Prevention. MMWR Recomm Rep. 2002;51:1–29. [PubMed] [Google Scholar]
- 6.Henrickson KJ, Axtell RA, Hoover SM, et al. Prevention of central venous catheter-related infections and thrombotic events in immunocompromised children by the use of vancomycin/ciprofloxacin/heparin flush solution: A randomized, multicenter, double-blind trial. J Clin Oncol. 2000;18:1269–1278. doi: 10.1200/JCO.2000.18.6.1269. [DOI] [PubMed] [Google Scholar]
- 7.Donlan RM, Costerton JW. Biofilms: survival mechanisms of clinically relevant microorganisms. Clin Microbiol Rev. 2002;15:167–193. doi: 10.1128/CMR.15.2.167-193.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sherertz RJ, Boger MS, Collins CA, et al. Comparative in vitro efficacies of various catheter lock solutions. Antimicrob Agents Chemother. 2006;50:1865–1868. doi: 10.1128/AAC.50.5.1865-1868.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Raad I, Hanna H, Dvorak T, et al. Optimal antimicrobial catheter lock solution, using different combinations of minocycline, EDTA, and 25-percent ethanol, rapidly eradicates organisms embedded in biofilm. Antimicrob Agents Chemother. 2007;51:78–83. doi: 10.1128/AAC.00154-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sissons CH, Wong L, Cutress TW. Inhibition by ethanol of the growth of biofilm and dispersed microcosm dental plaques. Arch Oral Biol. 1996;41:27–34. doi: 10.1016/0003-9969(95)00103-4. [DOI] [PubMed] [Google Scholar]
- 11.Chambers ST, Peddie B, Pithie A. Ethanol disinfection of plastic-adherent micro-organisms. J Hosp Infect. 2006;63:193–196. doi: 10.1016/j.jhin.2006.01.009. [DOI] [PubMed] [Google Scholar]
- 12.Metcalf SC, Chambers ST, Pithie AD. Use of ethanol locks to prevent recurrent central line sepsis. J Infect. 2004;49:20–22. doi: 10.1016/j.jinf.2003.08.010. [DOI] [PubMed] [Google Scholar]
- 13.Fitzgibbons S, Ching YA, Valim C, et al. Relationship between serum citrulline levels and progression to parenteral nutrition independence in children with short bowel syndrome. J Pediatr Surg. 2009;44:928–932. doi: 10.1016/j.jpedsurg.2009.01.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Aprahamian CJ, Chen M, Yang Y, et al. Two-hit rat model of short bowel syndrome and sepsis: independent of total parenteral nutrition, short bowel syndrome is proinflammatory and injurious to the liver. J Pediatr Surg. 2007;42:992–997. doi: 10.1016/j.jpedsurg.2007.01.071. [DOI] [PubMed] [Google Scholar]
- 15.Goulet O, Ruemmele F, Lacaille F, et al. Irreversible intestinal failure. J Pediatr Gastroenterol Nutr. 2004;38:250–269. doi: 10.1097/00005176-200403000-00006. [DOI] [PubMed] [Google Scholar]
- 16.Dannenberg C, Bierbach U, Rothe A, et al. Ethanol-lock technique in the treatment of bloodstream infections in pediatric oncology patients with broviac catheter. J Pediatr Hematol Oncol. 2003;25:616–621. doi: 10.1097/00043426-200308000-00006. [DOI] [PubMed] [Google Scholar]
- 17.Crenn P, Coudray-Lucas C, Thuillier F, et al. Postabsorptive plasma citrulline concentration is a marker of absorptive enterocyte mass and intestinal failure in humans. Gastroenterology. 2000;119:1496–1505. doi: 10.1053/gast.2000.20227. [DOI] [PubMed] [Google Scholar]
- 18.Forchielli ML, Young MC, Flores AF, et al. Immune deficiencies in chronic intestinal pseudo-obstruction. Acta Paediatr. 1997;86:1077–1081. doi: 10.1111/j.1651-2227.1997.tb14811.x. [DOI] [PubMed] [Google Scholar]
- 19.McHugh GJ, Wild DJ, Havill JH. Polyurethane central venous catheters, hydrochloric acid and 70% ethanol: a safety evaluation. Anaesth Intensive Care. 1997;25:350–353. doi: 10.1177/0310057X9702500404. [DOI] [PubMed] [Google Scholar]
- 20.Sanders J, Pithie A, Ganly P, et al. A prospective double-blind randomized trial comparing intraluminal ethanol with heparinized saline for the prevention of catheter-associated bloodstream infection in immunosuppressed haematology patients. J Antimicrob Chemother. 2008;62:809–815. doi: 10.1093/jac/dkn284. [DOI] [PubMed] [Google Scholar]
- 21.Opilla MT, Kirby DF, Edmond MB. Use of ethanol lock therapy to reduce the incidence of catheter-related bloodstream infections in home parenteral nutrition patients. JPEN J Parenter Enteral Nutr. 2007;31:302–305. doi: 10.1177/0148607107031004302. [DOI] [PubMed] [Google Scholar]
- 22.Kayton ML, GE, Ishill NM, et al. Adverse catheter-related events in a phase I trial of prophylactic ethanol administration to prevent central venous catheter infections. Presented at the 40th annual meeting of the American Pediatric Surgical Association Fajardo; Puerto Rico. 2009. [Google Scholar]