Abstract
A 23-year-old woman presented with bilateral papilloedema in a setting of Camurati-Engelmann disease (CED). She was investigated with neuroimaging showing no optic nerve canal stenosis or jugular vein canal compromise. Her MRI venogram was normal. Her opening pressure at lumbar puncture and serum alkaline phosphatase were raised. Her papilloedema resolved with long-term use of acetazolamide. We believe that our patient suffered from raised intracranial pressure directly as a result of decreasing intracranial volume secondary to CED.
Background
Camurati-Engelmann disease (CED), also known as progressive diaphyseal dysplasia, is a rare autosomal dominant condition causing progressive hyperostosis of diaphyses of long bones and cranium. Twenty-five per cent of patients suffer from symptoms related to skull base thickening.1 We discuss the aetiology of raised intracranial pressure leading to bilateral papilloedema in our patient.
Case presentation
A 23-year-old woman with CED but no other significant medical history presented with headaches and visual disturbances. Drug history was of oral painkillers but no previous oral steroids. Her visual acuity was 6/18 and 6/12 right and left, respectively, with no relative afferent pupillary defect (RAPD), normal colour vision (Ishihara plates) and no proptosis. Bilateral papilloedema and macular stars (figure 1) with corresponding enlarged blind spots and nasal defects on visual field tests (figure 2) were discovered on further examination.
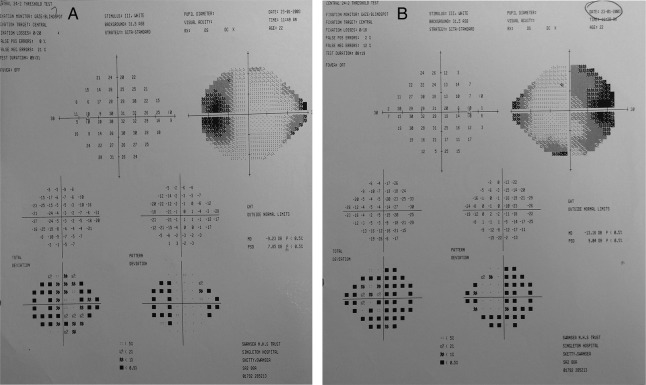
Figure 1.
(A) Right and (B) left papilloedema with macular stars at presentation.
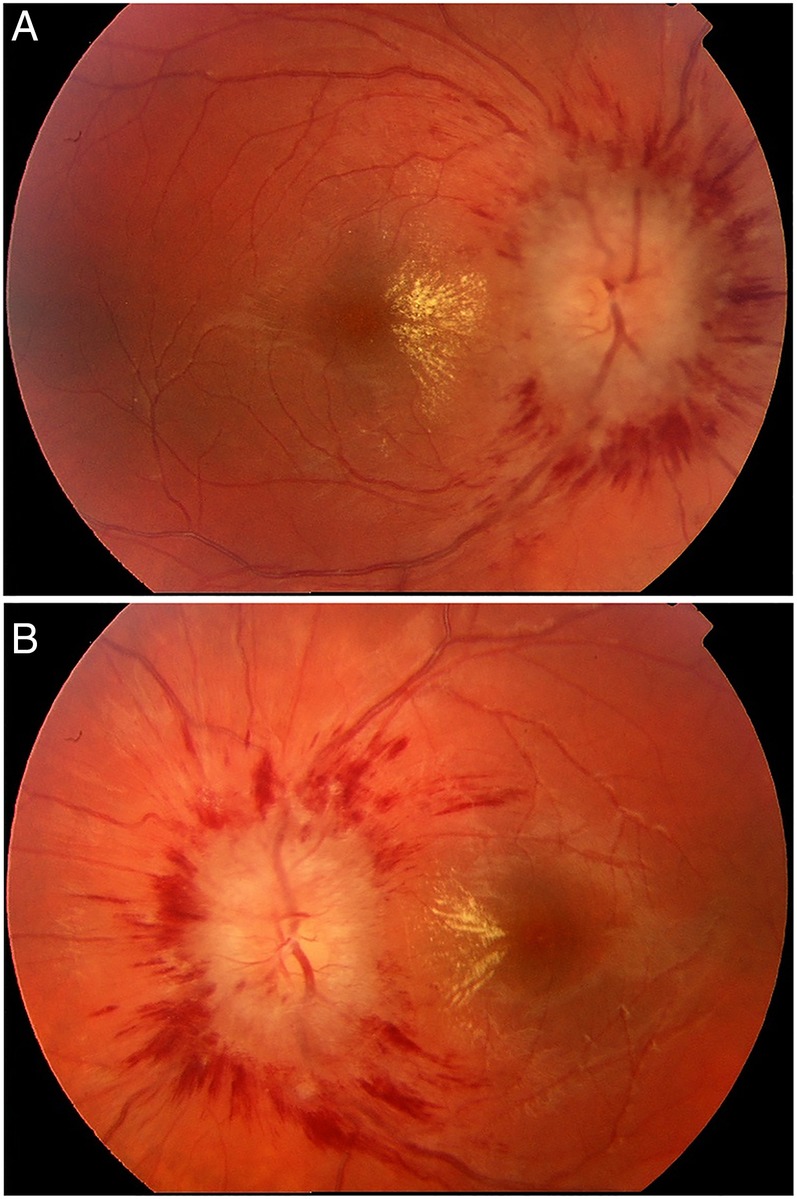
Figure 2.
Visual field plots (Humphrey visual field analyser test pattern 24–2) at presentation showing right (A) and left (B) eye visual field defects with enlarged blind spots and nasal defects, in keeping with diagnosis of papilloedema.
Investigations
Raised alkaline phosphatase (464 U/L) was noted, consistent with active CED.2 CT of the brain showed extensive thickening of skull and facial bones, with normal optic nerve canals (figure 3). Opening pressure of 40 cm cerebrospinal fluid (CSF) was recorded at lumbar puncture (LP) and CSF analysis was within normal limits. A MRI venogram was also normal.
Figure 3.
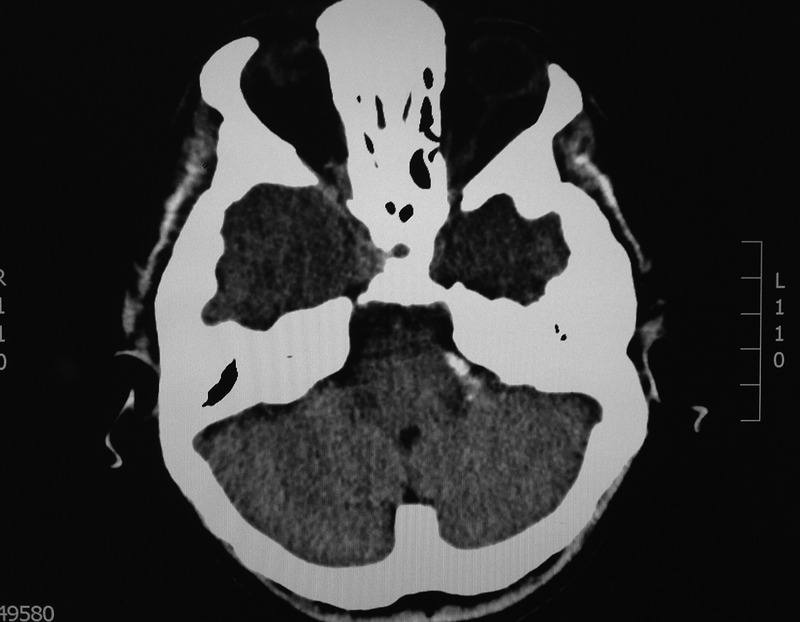
CT of the brain showing diffuse thickening of skull base.
Differential diagnosis
Bilateral papilloedema is caused by raised intracranial pressure.
The causes of raised intracranial pressure (ICP) include:
Mass effect: space occupying lesion, haemorrhage and cerebral oedema;
Increased CSF production;
Decreased CSF outflow: tumour, infection and congenital cysts;
Idiopathic intracranial hypertension;
Drug related: steroids, tetracycline and oral contraceptives.3
Treatment
Oral acetazolamide was started for raised ICP with resolution of papilloedema and visual field defects, leaving the patient with bilateral optic nerve atrophy (figure 4).
Figure 4.
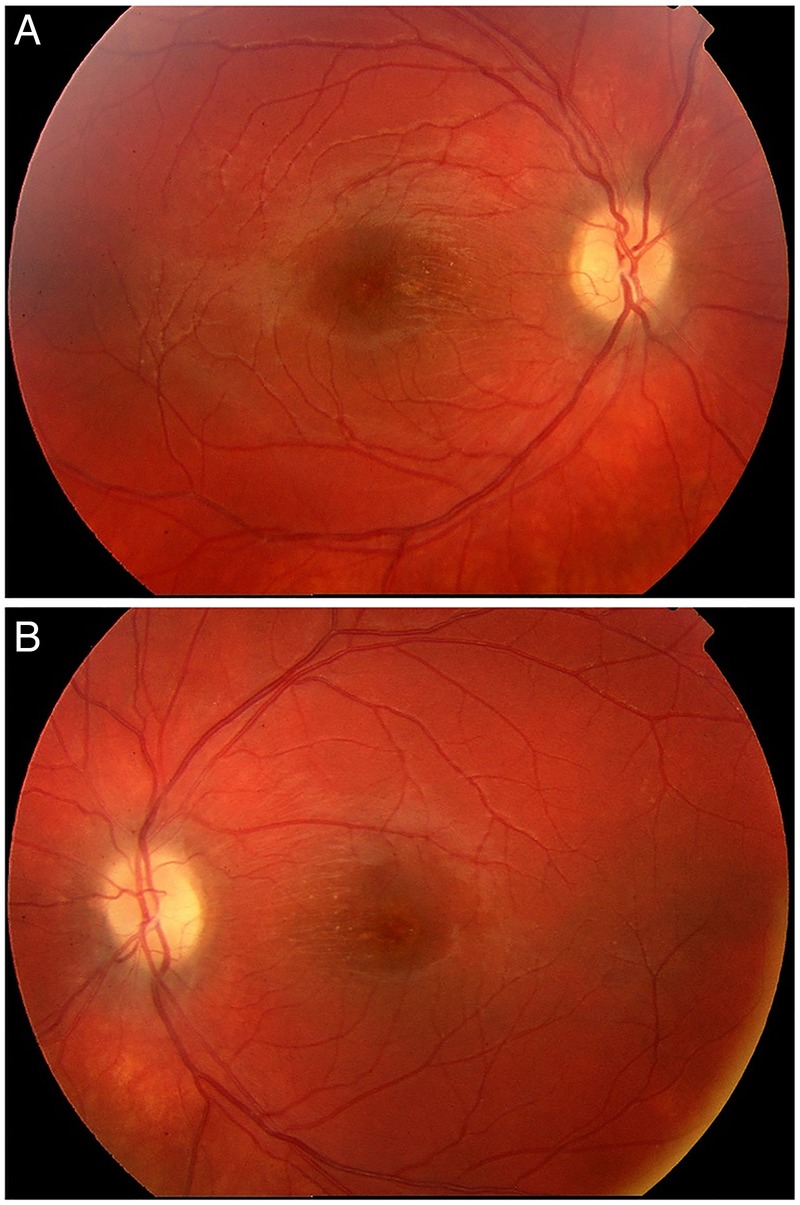
(A) Right and (B) left optic nerve atrophy following papilloedema resolution.
Outcome and follow-up
The patient's vision returned to 6/5 in both eyes following start of acetazolamide, however, the initial episode of severe papilloedema caused a mild degree of optic nerve atrophy given the pale appearance of both optic nerves (figure 4). In the following 10 years of follow-up, our patient suffered five recurrences of symptoms while off treatment, with reappearance of bilateral papilloedema, high opening pressures on repeated LPs and raised alkaline phosphatase with no clinical evidence of concurrent active bone disease. Her repeat imaging confirmed thickening of skull vault and base with preserved optic foramina. Long-term acetazolamide therapy is on-going and she remains free of symptoms and signs.
Discussion
Patients with CED usually present in childhood, with bone pain, proximal muscle weakness and waddling gait. Frontal bossing of the skull, enlargement of the mandible as well as cranial nerve impingement resulting in facial palsy, visual and hearing impairments, can also occur. Involvement of the orbit can lead to proptosis, papilloedema, epiphora, glaucoma and globe subluxation.1 4 Reducing intracranial volume, secondary to skull base bony thickening together with jugular foramen stenosis, leading to neurovascular compromise, is responsible for raised ICP.1 5 The other mechanisms for papilloedema are either related to optic nerve compression at the optic foramina, or the use of steroids for relief of bone pain.6 Our patient had a normal MRI venogram with no evidence of jugular foramen narrowing and no optic canal stenosis on repeated CT scans, excluding neurovascular compromise and optic nerve compression as causative mechanisms of her papilloedema. She has never received steroids. Each recurrence of her symptoms was associated with raised alkaline phosphatase, indicating bone activity in CED. She is also unable to stop acetazolamide, which reduces the CSF production. These factors would suggest that our patient with CED is suffering from episodes of raised ICP, manifesting with papilloedema and headaches, solely as a result of acute skull bone thickening leading to decreasing intracranial space. Wright et al6 previously suggested this mechanism of papilloedema in three patients with CED. Given the Monro-Kellie volume–pressure hypothesis,7 it is feasible to suggest decreasing intracranial volume as a sole cause of raised ICP in CED. All intracranial components need to fit into a smaller rigid space. Autoregulatory mechanism, which initially copes by displacing blood and CSF to maintain physiological ICP in this new situation, fails before further insult from jugular vein foramen stenosis.
Steroids, calcitonin and biphosphonates can be used to control symptoms of bone pain in CED with steroids capable of correcting the radiographic abnormalities.4 Cranial nerve dysfunction in CED results from combination of nerve foramina stenosis and raised intracranial pressure. Internal auditory canal and facial nerve canal decompressions each have 50% success rates with long-term symptomatic improvement.5 Treatment of optic nerve dysfunction with optic nerve fenestration or ventriculoperitoneal shunts seem to have limited long-term success rates. Given the progressive nature of bone thickening in CED, aggressive cranial decompression with craniotomy is required in advanced disease to control raised intracranial pressure.1 5 6 Resolution of papilloedema with acetazolamide therapy has been described in one patient with CED by Wright et al.6 We report another case of bilateral papilloedema as a result of raised ICP secondary to reducing intracranial volume as part of skull base thickening in CED, treated successfully with medical therapy of acetazolamide over 10 years of follow-up.
Patient's perspective.
As an infant I had flat feet and knock-knees, and always had an awkward gait when I walked, but I was otherwise a happy, healthy child. At the age of 3 years, I began experiencing pain in my lower right leg bones. Approximately 18 months later, I was sent for a muscle biopsy to try and diagnose my condition. All muscle and nerve tests conducted showed no abnormalities, but some last resort X-rays of my lower legs showed up the abnormalities in my bones. It was then that I was given the diagnosis of Camurati-Engelmann's disease (CED).
When I was 23 years old I began ‘seeing stars’ in my vision, just like the ones you see if you stand up too fast, or if you have been rubbing your eyes, only, I was seeing them when I lay in bed or sat watching television. These episodes became more and more frequent, and within a month I was seeing stars in my peripheral vision constantly, and in the later stages my vision would black out completely for 20–30 s a few times a day. During the later stages I had no depth perception whatsoever, for example, I could see that there was a kerb at the side of the road, but I was not able to tell if it was a step-up or a step-down. I was unable to read or watch television as the more I would try to focus on something, it would simply disappear. An ophthalmologist reviewed me around 3 months after my visual symptoms began and I was admitted to hospital immediately. I was given a lumbar puncture (LP) where the opening pressure was 40 mm Hg and several millilitres of cerebrospinal fluid were drained off to reduce the pressure. A sample was also sent away for tests, but no abnormalities were found. I was immediately started on acetazolamide (Diamox). I underwent various scans and tests, including a visual fields test—it was incredibly difficult to distinguish the test-lights from the constant stars in my vision. My symptoms had begun improving and my vision gradually cleared, although it is not as good as it used to be. My pain and hearing loss also improved once the pressure was lowered.
I was taken off the acetazolamide about 12 months later, when my doctors were satisfied that everything had settled down, and all was well for a while, but eventually I began experiencing headaches and ‘stars’ in my vision again, and had to undergo further LPs and treatment with acetazolamide.
Each time the medication has been stopped, or significantly lowered, the symptoms of raised pressure return. I have undergone eight LPs since the initial diagnosis. My last LP (around 4 years ago) had an opening pressure of 41 mm Hg, but there had been no visual symptoms, only severe headaches.
I continue to take 500 mg acetazolamide daily and attend neurology and ophthalmology (including visual fields) outpatient appointments every 6 months. I am vigilant for any signs that the pressure is increasing and seek immediate advice should I experience any visual problems or severe headaches.
My CED symptoms continue to spread through my body and now I experience pain in all areas of all limbs, plus in my skull and jaw bones. The pain is still as erratic as ever and managed only with daily pain medication. The bone thickening is now physically visible at the ends of my long bones and restricts some movements at my joints. It has exacerbated the effect of misalignment in my knock-knees and flat feet making certain movements incredibly painful.
In 2005, I started an online support group for sufferers of CED; we now have over 150 members from all across the world. We all vary in the ways in which we are affected by CED, but the increased intracranial pressure is a common factor among many of us. We hope that, by joining forces, we will attract more attention from those wishing to study this disease, than we would as individuals. Our group can be found at https://www.facebook.com/groups/CamuratiEngelmannDisease/
Learning points.
Camurati-Engelmann disease (CED) is a rare condition leading to progressive hyperostosis of diaphyses of long bones and cranium. Less than 25% of patients suffer from cranial nerve dysfunction.
Papilloedema in CED can result from optic foramen stenosis, raised intracranial pressure (ICP) or use of steroids. Patients with papilloedema need urgent imaging to ascertain its cause.
Raised ICP in CED is thought to be related to the neurovascular compromise from jugular vein canal stenosis in conjunction with decreasing intracranial volume. Our case demonstrates that raised intracranial pressure in CED can result solely from decreased intracranial volume.
Acetazolamide can be considered as first-line therapy for raised intracranial pressure manifesting with papilloedema in CED before surgical treatments are required.
Footnotes
Contributors: MA is the supervising consultant, involved in patient care and responsible for editing of first author’s text.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Carlson ML, Beatty CW, Neff BA et al. . Skull base manifestations of Camurati-Engelmann disease. Arch Otolaryngol Head Neck Surg 2010;136:566–75. 10.1001/archoto.2010.68 [DOI] [PubMed] [Google Scholar]
- 2.Hernández MV, Peris P, Guañabens N et al. . Biochemical markers of bone turnover in Camurati-Engelmann disease: a report on four cases in one family. Calcif Tissue Int 1997;61:48–51. 10.1007/s002239900293 [DOI] [PubMed] [Google Scholar]
- 3.Kanski J. Neuro-opthalmology. In: Clinical ophthalmology a systemic approach. 6th edn Elsevier Limited, 2007:799–802. [Google Scholar]
- 4.Janssens K, Vanhoenacker F, Bonduelle M et al. . Camurati-Engelmann disease: review of the clinical, radiological, and molecular data of 24 families and implications for diagnosis and treatment. J Med Genet 2006;43:1–11. 10.1136/jmg.2005.033522 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mocco J, Komotar RJ, Zacharia BE et al. . Aggressive cranial vault decompression for cranial hyperostosis: technical case report of two cases. Neurosurgery 2005;57(1 Suppl):E212 10.1227/01.NEU.0000163686.75095.B8 [DOI] [PubMed] [Google Scholar]
- 6.Wright M, Miller NR, McFadzean RM et al. . Papilloedema, a complication of progressive diaphyseal dysplasia: a series of three case reports. Br J Ophthalmol 1998;82:1042–8. 10.1136/bjo.82.9.1042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dunn LT. Raised intracranial pressure. J Neurol Neurosurg Psychiatry 2002;73:i23–7. [DOI] [PMC free article] [PubMed] [Google Scholar]