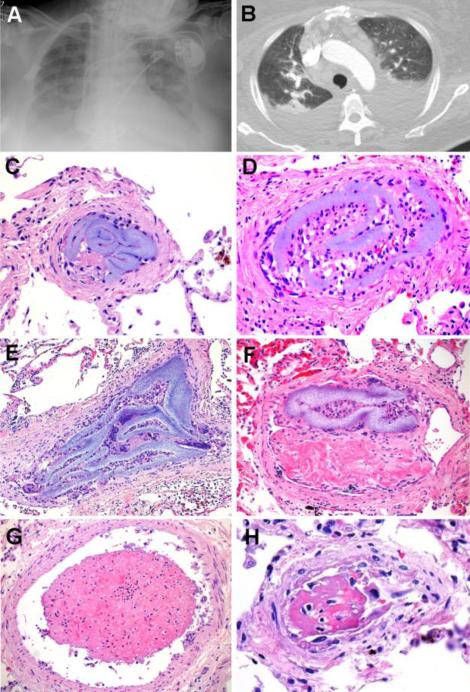
Figure 1. Summary, Patient 1.
A 73-year-old woman with hypertrophic cardiomyopathy, sinus node dysfunction, hypertension, diabetes mellitus type 2 and chronic renal disease presented with pulmonary edema. Cardiac enzymes were negative; BNP and creatinine were elevated. Initially, the patient was improving with diuresis, intravenous fluids and dialysis. After admission, a CVC was placed and broad-spectrum antibiotics were administered for suspected pneumonia. The patient's respiratory symptoms subsequently worsened; however, transthoracic echocardiography and right and left cardiac catheterization revealed no definite cardiac etiology for her symptoms. During her hospitalization, she developed suspected PE, elevated ESR, p-ANCA+ vasculitis, coagulopathy of unknown cause, and prominent mediastinal lymphadenopathy. Chest X-Ray (A) and pulmonary CT angiography (B) showed pleural effusions and areas of pulmonary consolidation, with no evidence of PE. Despite multiple negative cultures, the patient developed multiple organ dysfunction syndrome and suspected sepsis, progressing to death. Autopsy, performed 1 month after admission, failed to reveal any natural etiology for her terminal symptoms. Retrospective histopathological analysis, however, showed multifocal HPE involving the bilateral peripheral pulmonary arteries (C-F), as well as the heart and central nervous system (not shown). Intravascular histiocytes (D), giant cells (E), and fibrous reaction (F) were associated with HPE. Adjacent vessels showed microthrombus formation (G) and areas of vascular injury (H). The cause of death was retrospectively attributed to widespread pulmonary HPE in the setting of hypertrophic cardiomyopathy [C-H: H&E, original matnification 600X].