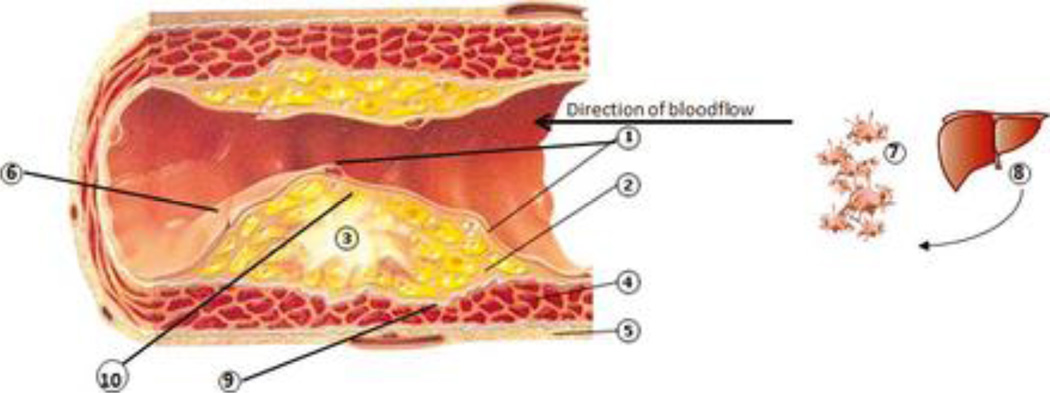
Figure 1. Inflammatory mechanisms linking periodontal diseases to cardiovascular diseases.
1. Dysfunctional endothelial lining: partial loss of integrity. ↑ adhesion molecules (ICAM-1, VCAM-1, E-selectin, P-selectin) and chemoattractants (e.g. IL-8, thrombin), increased platelet and leukocyte adhesion; diapedesis of monocytes, dendritic cells (both possibly with ingested bacteria) and T cells into the underlying inflammatory lesion. Activated platelets may form mini-thrombi. 2. Inflammatory lesion which may be in part initiated and/or propagated by bacteria originating from the periodontitis lesion, and also propagated by pro-inflammatory mediators (IL-1, IL-6, CRP, TNFα) and chemotactic factors (e.g. monocyte chemotactic protein-1) spilled over from the periodontal lesion, produced both in the liver and systemically. 3. Atheroma maturation. Lipid streaks and calcifications, comprised of modified low-density lipoproteins phagocytosed within macrophages/foam cells, resulting in ↑ pro-inflammatory cytokines (IL-6, IL-1, TNFa), ↑ chemoattractants (IL-8), ↑ matrix metalloproteinases (MMPs); the upregulated inflammatory lesion induces dysfunctional endothelial lining. CD4+ Th cells (↑IL-12,IL-18, IFN-γ) are also within the atheroma. 4. Smooth muscle cells (SMCs) and fibroblast with progressive fibrosis and loss of demarcation between inflammatory lesion and SMCs; development of a compensatory blood supply and increased outer muscle layer. 2 + 3 + 4 form the initimal layer of the artery. 5. Outer muscle layer. 6. Disintegrated endothelial lining (i.e. plaque rupture, exposition of underlying atherosclerotic plaque) generates thrombin from prothrombin, which in turn enzymatically generates fibrin from fibrinogen, →clotting cascade resulting in thrombosis, consequently to stroke or myocardial infarction. This process may be mediated by repeated bacteremias and pro-inflammatory state and activated inflammatory cells, such as from chronic periodontitis. 7. Activated platelets by bacteria in circulation from periodontal lesions, forming aggregates, the initiation of micro thrombus formation (out of scale with the whole picture). 8. ↑production of clotting factors in the liver due to inflammatory signals (IL-6), →pro-thrombotic state. Also increased production of acute phase reactants, including CRP, which will increase the pro-inflammatory state (out of scale with the whole picture). 9. Decreased collagen production and activation of MMPs resulting in reduction of SMC content and increased degradation of collagen that borders the fibrous cap, weakening the strength of the vessel, leading to fissuring of the atheroma. 10. In a progressed stage, the atheroma comprises of a large necrotic core which is exposed to the vasculature within the lesion, leading to contact with platelets, initiation of coagulation and ultimately, plaque rupture in so-called vulnerable lesions.