Abstract
Background:
Although anterior cruciate ligament (ACL) reconstruction techniques that preserve remnant tissues have been described, complete preservation may be difficult, with little known about its clinical advantages.
Purpose:
To compare clinical outcomes in patients undergoing ACL reconstruction with and without ACL remnant preservation.
Study Design:
Case-control study.
Methods:
Of 372 patients who underwent surgical treatment of an ACL injury between September 2006 and July 2010, 154 had no remaining identifiable ligament tissue and were excluded from this study. Attempts were made to preserve the ACL remnant as much as possible in the remaining 218 patients. These patients were divided into 2 groups: those in whom the remnant was preserved (group 1, n = 85) and those in whom the remnant was not preserved (group 2, n = 98). Patients were followed for at least 24 months. Outcomes, including graft rupture, were compared in the 2 groups.
Results:
Time from injury to surgery was significantly shorter (7.3 ± 16.3 vs 16.0 ± 30.3 months; P < .05) and the preinjury Tegner activity was significantly higher (7.6 ± 1.4 vs 7.1 ± 1.2; P < .05; 95% confidence interval, 1.2-13.7) in group 1 than in group 2. The postoperative negative ratio of the pivot-shift test was similar in the 2 groups (87% vs 81%). Anterior stability of the knee, as measured by a KT-2000 arthrometer, was significantly better in group 1 than in group 2 (1.0 ± 0.8 vs 1.3 ± 1.0 mm; P < .05). ACL graft rupture occurred in 1 patient (1.1%) in group 1 and in 7 patients (7.1%) in group 2 (P < .05). Regression analysis showed that preservation of the remnant decreased the likelihood of graft rupture (odds ratio, 11.2; 95% confidence interval, 1.2-101.7).
Conclusion:
These findings confirmed that preserving the remnant tissue of the ACL may facilitate recovery of function and decrease graft rupture after primary reconstruction.
Keywords: anterior cruciate ligament reconstruction, remnant preservation, prospective, hamstring autograft, reinjury
Successful anterior cruciate ligament (ACL) reconstruction depends on multiple factors, including anatomic graft placement with secure fixation, graft incorporation, graft revascularization, and ligamentization.2,5,7 In addition to stability, a high quality of proprioception is needed after ACL reconstruction.6,16,24 The presence of remnant tissues in the ruptured ACL, containing mechanoreceptors and free neural ends, can help reinnervate the ACL autograft.11,14,28 Histologic examination of human ACL remnants has revealed their healing potential, especially that due to intact vascular support by the synovial sheath.4,12 Thus, preservation of the mechanoreceptors and vascular network in an ACL remnant may improve recovery of joint positioning and enhance early revascularization of the graft.
The clinical results of ACL reconstruction techniques with preservation of the remnant tissues have been described.1,3,8,20–22,25,27,35,37 Most of them, termed as “tissue-preserving surgeries,” were performed with type 1, 2, or 3 ACL remnant tissue, as reported by Crain et al.10 However, complete preservation of the remnant may be difficult because little is known about the quantity and quality of the remnant before and after surgery. Remnant preservation, however, should involve minimally invasive procedures on most tissues in the joint.
Despite continuous improvements in ACL reconstruction techniques, these patients remain at risk for repeated ACL injury, which has devastating outcomes for many athletes.9,30,32,36 A systematic review of evidence level 1 and 2 studies with a minimum of 5 years of follow-up demonstrated that the risk of ACL graft rupture in the ipsilateral knee is 5.8%.36 Improvements in ACL reconstruction procedures may therefore restore normal function and prevent future injuries.
The finding that remnant tissues enhance mechanical stability and proprioceptive function suggests that preservation of these tissues may decrease the likelihood of repeat ACL injury.30 Furthermore, to our knowledge, no study to date has compared the incidence of repeat ACL injury after reconstruction with or without preservation of the remnant. We therefore hypothesized that preserving remnant tissues during ACL reconstruction with a hamstring autograft reduces the risks of autograft ruptures. Accordingly, we performed this study to test this hypothesis.
Materials and Methods
Patients
Between September 2006 and July 2010, a total of 372 patients underwent surgical treatment of an isolated unilateral ACL injury and met the following criteria: (1) closed femoral and tibial physes, (2) no history of surgery on either knee, (3) no or minimal osteochondral degeneration on radiographic examination (stage 0 or 1 in the Kellgren and Lawrence staging system18), and (4) were scheduled to undergo single-bundle ACL reconstruction using a hamstring autograft. Of the 372 patients, 154 could not be considered for remnant preservation because there was no identifiable remnant tissue. This procedure was performed in 218 patients who had ACL remnant tissue of type 1 (scarring to the posterior cruciate ligament [PCL]), type 2 (healed to the roof of the notch), or type 3 (healed to the lateral wall), as classified by Crain et al.10 We excluded 154 cases because there was no identifiable ligament tissue remaining (type 4: resorption).
During surgery, we tried to preserve the remnant as much as possible. Patients were divided into 2 groups based on remnant preservation following surgery but were not randomized. After insertion of the graft, preservation of the remnant was considered possible if the following conditions were met: (1) the graft was covered with synovial tissues and had abundant blood vessels, (2) coverage of more than 75% of the graft from the tibial attachment, and (3) presence of a bridge between the femur and tibia. Group 1 consisted of 100 patients in whom we were able to preserve the ACL remnant, and group 2 consisted of 118 patients without ACL remnant preservation, defined as incomplete according to our definition. Of the 218 patients, 35 were lost to follow-up for unknown reasons. Thus, 85 (85%) patients in group 1 and 98 (83%) in group 2 were followed for a minimum of 24 months (mean, 32 months; range, 24-68 months). The 183 patients consisted of 124 males and 59 females (mean age, 25 years; range, 14-48 years). There were no statistically significant differences for mean age and follow-up period between the 2 groups (Table 1).
Table 1.
Patient Demographic and Clinical Characteristicsa
| Group 1 | Group 2 | P Value | |
|---|---|---|---|
| Total patients, n | 100 | 118 | |
| Lost to follow-up, n | 15 | 20 | |
| Patients reviewed, n | 85 | 98 | |
| Follow-up rate, % | 85 | 83 | |
| Age at surgery, y, mean ± SD | 24.3 ± 8.4 | 26.1 ± 8.3 | NS |
| Time from injury to surgery, mo, mean ± SD | 7.3 ± 16.3 | 16.0 ± 30.3 | <.01 |
| Mechanism of injury, contact/noncontact | 19/66 | 14/84 | NS |
| Preinjury Tegner activity level, mean ± SD | 7.6 ± 1.4 | 7.1 ± 1.2 | <.05 |
| Side-to side difference in KT-2000, mm, mean ± SD | 4.1 ± 1.9 | 4.6 ± 1.8 | NS |
| Meniscal treatment/reviewed patients (%) | 16/85 (18.8) | 24/83 (24.5) | NS |
| Follow-up period, mo, mean ± SD | 33.3 ± 10 | 31.0 ± 9.8 | NS |
aGroup 1, patients in whom the ACL remnant could be preserved; group 2, patients in whom the ACL remnant could not be preserved; ACL, anterior cruciate ligament; SD, standard deviation; NS, not significant.
Surgical Technique
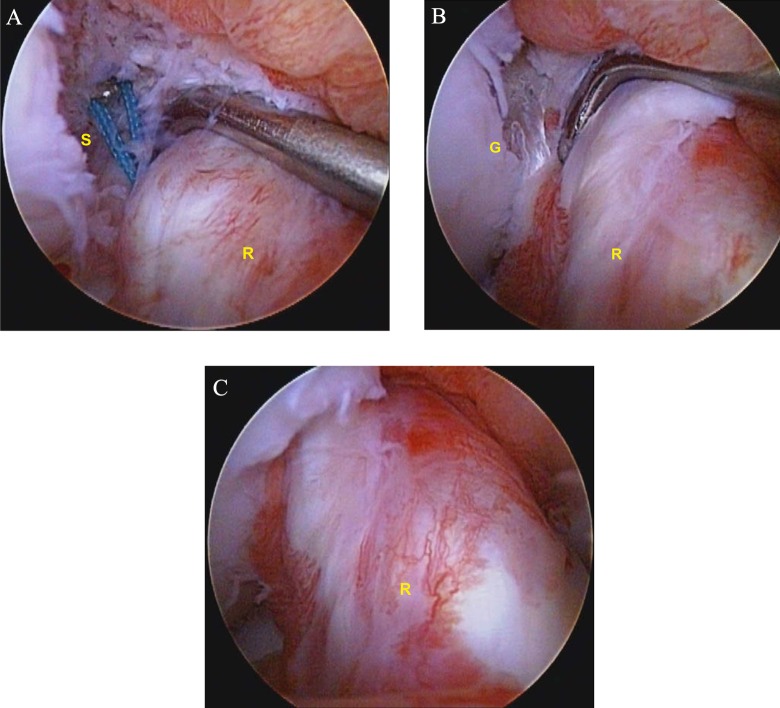
Three surgeons (Y.T., H.I., and H.K.) performed or supervised (made all important surgical decisions) operations on all patients. All patients were examined under general anesthesia (Lachman test, pivot-shift test). Before ACL reconstruction, routine diagnostic arthroscopy was performed through the far anteromedial (FAM) portal with a 30° oblique arthroscope. The status of each ACL remnant was assessed, and the surgeons decided whether ACL reconstruction could be performed using a remnant-preserving technique using previously described criteria.10 Patients without a remnant were excluded. Any meniscal injury or articular cartilage lesion was evaluated; if meniscal tears required treatment, a meniscal repair, meniscal rasping, or partial meniscectomy was performed. The semitendinosus tendons were harvested through a straight 3-cm skin incision over the medial aspect of the proximal tibia, and the muscle tissue of the harvested semitendinosus was removed. The 5 strands were utilized as a graft for augmentation, and Telos artificial ligaments (Ai-Medic, Tokyo, Japan) were connected at the distal and proximal ends of the graft loop, yielding 5 strands, each 8 to 11 mm in diameter.19 To preserve the remnant as much as possible, we cleaned the lateral wall carefully using a small bone curette and raspatory (see Video 1). After that, we determined the femoral insertion of the graft. A 2.4-mm Kirschner wire (K-wire) was inserted from the FAM portal into the femoral footprint behind the ridge while retracting the remnant. While viewing the tibial attachment of the ACL arthroscopically, a 2.4-mm K-wire was inserted using an ACL tibial guide (Linvatec, Largo, Florida, USA), positioned at the central portion of the remnant tissue, and set at a 40° sagittal angle from the tibial long axis. During these procedures, care was taken to minimize damage to the ACL remnant. The guide wire was advanced into the joint and carefully directed in line with the ACL remnant. Intraoperative radiographs were used to confirm the location of the guide wire tips. From the FAM portal, and using this K-wire as a guide, the femoral socket was drilled to a depth of 10 mm at a diameter equal to that of the graft, and a 4.5 mm–diameter tunnel was drilled over the guide wire to the lateral aspect of the femur. A tibial bone tunnel was made using a cannulated reamer of the same diameter as that of the distal portion of the graft. During tunnel creation, the reamer was advanced carefully to minimize damage to the remnant. After removing the bony debris in both tunnels, a string to guide the graft was passed from the tibial tunnel, posterolateral to the remnant, to the femur side. A graft composite was passed through the tibial and femoral tunnels, taking care to prevent damage to the remnant (Figure 1 and Video 2). The graft was then inserted into the knee joint through an anteromedial portal and was secured to the lateral femoral cortex by flipping the Telos Button (Ai-Mdic), introduced through a 1-cm incision on the lateral thigh at the femur side.19 The double-stapling technique38 was used for graft fixation on the tibial side at 30° of knee flexion.
Figure 1.
Arthroscopic lateral portal view of the right knee at 90° of flexion showing the remnant preservation technique. (A) A string is pulled intra-articularly through the tibial tunnel, the remnant, and the femoral socket under arthroscopic visualization. (B) The folded grafts are gently removed. (C) The grafts are covered with remnant. G, graft; R, remnant; S, string.
Postoperative Management
All patients followed the same postoperative rehabilitation protocol. Postoperative knee braces were not used, and all patients were allowed to bear full weight immediately. Range of motion, isometric muscle, and closed kinetic chain exercises were allowed from the first postoperative day. Jogging was encouraged after 2 months, and open kinetic chain exercises were allowed after 3 months. Jump landing, twisting, and cutting exercises were allowed at 4 months, and sprinting and other competitive exercises were allowed at 6 months. Subsequently, return to full sports activities was permitted stepwise.
Postoperative Clinical Evaluation
All objective evaluations were performed by experienced orthopaedic surgeons independently. Joint stability was assessed at final follow-up using a KT-2000 arthrometer (MED Metric, San Diego, California, USA) by performing Lachman, pivot-shift, and manual maximum displacement tests. Arthrometric measurement was recorded as side-to-side differences between the injured and uninjured knees. Pivot-shift test results were evaluated quantitatively as described.13 Subjective evaluations included time from surgery to return to sports activity and change in Tegner activity scale35 from before injury to return to sports activity. All patients who sustained an ACL graft rupture or subsequent contralateral ACL rupture after surgery were examined by an orthopaedic surgeon who confirmed the diagnosis. For these patients, the postoperative clinical data recorded immediately before the revision surgeries were regarded as final follow-up data.
Statistical Analysis
Groups were compared using the Mann-Whitney U test, with statistical significance set at P < .05. The chi-square test was used to compare the graft rupture rates and other categorical variables between the 2 groups. Then, binary logistic regression was used to measure the association between each measured variable and the risk of graft rupture, with results considered significant at the 95% confidence interval (CI) level. All statistical analyses were performed using SPSS for Windows software version 21.0 (IBM, Armonk, New York, USA).
Results
The mean interval between ACL injury and reconstruction was significantly shorter (7.3 ± 16.3 vs 16.0 ± 30.3 months, P < .05) and preinjury Tegner activity was significantly higher (7.6 ± 1.4 vs 7.1 ± 1.2; P < .05; 95% CI, 1.2-13.7) in group 1 than in group 2. There were no between-group differences in the ratio of mechanism of injury (contact/noncontact), in the incidence of meniscus injury, or in treatment methods (Table 1). At the time of surgery, an attached ACL remnant was noted in 218 of 372 (59%) patients, with the lateral wall being completely empty in the other 154 patients (41%). Although we attempted to preserve the remnant, this was not achieved satisfactorily in all patients with identifiable tissue; preservation was incomplete in 118 of 218 patients (54%). None of these patients had a cartilage injury requiring supplemental surgical procedures. Postoperatively, there were no significant differences between groups 1 and 2 with regard to Tegner score change on return to sport activity (0.23 ± 0.6 vs 0.26 ± 0.6 points) and negative ratio on the pivot-shift test (87% vs 81%). Anterior stability of the knee, as measured by the KT-2000 arthrometer, was significantly better in group 1 than in group 2 (1.0 ± 0.8 vs 1.3 ± 1.0 mm, P < .05). In groups 1 and 2, a side-to-side difference of ≥3 mm was observed in 3% and 5% of patients, respectively. The difference was ≥5 mm in 1% of the patients in group 2 compared with none in group 1. Eight of the 183 patients (4.4%) sustained an ACL graft rupture during follow-up, including 1 of 85 patients (1.2%) in group 1 and 7 of 98 (7.1%) in group 2 (P < .05). Contralateral ACL ruptures occurred in 13 patients (7.1%): 5 (5.9%) in group 1 and 8 (8.1%) in group 2 (not significant, Table 2). Regression analysis showed that preservation of the remnant was a significant predictor of nonrupture of a graft (odds ratio, 11.2; 95% CI, 1.2-101.7). Other variables tested, including sex, age, time from injury to surgery, mechanism of primary ACL injury, meniscal treatment at index surgery, and postoperative Tegner activity level, were not predictive of graft rupture (Table 3).
Table 2.
Clinical Resultsa
| Group 1 | Group 2 | P Value | |
|---|---|---|---|
| Duration from surgery to return to sports activity, mo, mean ± SD | 9.5 ± 3.5 | 9.6 ± 3.4 | NS |
| Difference in Tegner activity, mean ± SD | 0.23 ± 0.6 | 0.26 ± 0.6 | NS |
| Side-to side difference in KT-2000, mm, mean ± SD | 1.0 ± 0.8 | 1.3 ± 1.0 | <.05 |
| Pivot-shift test (negative rate), % | 87 | 81 | NS |
| Graft rupture, No. of patients (%) | 1 (1.2) | 7 (7.1) | <.05 |
| Contralateral ACL injury, No. of patients (%) | 5 (5.9) | 8 (8.2) | NS |
aGroup 1, patients in whom the ACL remnant could be preserved; group 2, patients in whom the ACL remnant could not be preserved; ACL, anterior cruciate ligament; SD, standard deviation; NS, not significant.
Table 3.
Incidence and ORs of Graft Ruptures After Surgery With Measured Variablesa
| No. of Graft Ruptures/Total | Incidence (%) | OR | 95% CI for OR | P Value | ||
|---|---|---|---|---|---|---|
| Lower | Upper | |||||
| Age | 0.92 | 0.79 | 1.06 | .25 | ||
| Duration of injury to surgery | 0.97 | 0.86 | 1.08 | .56 | ||
| Mechanism of primary ACL injury | 0.44 | 0.04 | 4.33 | .48 | ||
| Contact | 1/33 | 3 | ||||
| Noncontact | 7/150 | 5 | ||||
| Tegner activity level | 1.59 | 0.83 | 3.07 | .17 | ||
| 3-7 | 4/117 | 3 | ||||
| 8-10 | 4/66 | 6 | ||||
| Patient sex | 1.75 | 0.25 | 12.11 | .57 | ||
| Male | 6/124 | 5 | ||||
| Female | 2/59 | 3 | ||||
| Meniscus treatment | 0.92 | 0.15 | 5.65 | .93 | ||
| Yes | 2/40 | 5 | ||||
| No | 6/143 | 4 | ||||
| Type of surgery | 11.24 | 1.24 | 101.66 | .03 | ||
| Group 1 | 1/85 | 1 | ||||
| Group 2 | 7/98 | 7 | ||||
aGroup 1, patients in whom the ACL remnant could be preserved; group 2, patients in whom the ACL remnant could not be preserved; ACL, anterior cruciate ligament; OR, odds ratio; CI, confidence interval.
Discussion
ACL reconstruction techniques that preserve an ACL remnant have been found to yield satisfactory results.1,3,8,20–22,25,27,34,38 However, the ability to preserve remnant tissues at the time of surgery was not evaluated because little was known about the quantity and quality of the remnant after surgery. A double-bundle ACL reconstruction method with remnant preservation, creating 4 tunnels at the attachment of the remnant, yielded good clinical results,38 as did a double-bundle reconstruction with remnant preservation that avoided impingement of the reconstructed graft against the ACL remnant or the roof of the intercondylar notch.27 This latter method involved the creation of a passage through the ACL remnant using a curved hemostat. However, double-bundle reconstruction requires 4 bone holes, which has been associated with a risk of destroying the site of remnant attachment, the most important site of native ACL.27,38 Furthermore, minimal debridement of the residual stump of the ruptured ACL was found to result in earlier revascularization of ACLR.15 We utilized 1 femoral and 1 tibial tunnel to preserve the maximal amount of remnant tissue. Preservation of the ACL tibial stump also significantly reduces the leakage of arthroscopy fluid through the tibial tunnel.17
Although double-bundle ACL reconstruction yields good clinical results, the creation of many tunnels can more easily result in nonpreservation of the remnant. Techniques to preserve the remnant should not only keep the remnant intact but also be minimally invasive, not only of remnant tissue but also of many structures within the joint. Although selective anteromedial bundle (AMB) and posterolateral bundle (PLB) reconstruction techniques have been described,25,26,29,33 distinguishing damage to the AMB or PLB selectively is very difficult. Moreover, selective AMB reconstruction without invasion of the anterior fiber does not meet our postoperative definition of preservation. None of our patients experienced extension loss, suggesting that our surgical method of creating only 1 bone tunnel at the tibial insertion to decrease the debris in the remnant and of never invading the anterior fibers of AMB may reduce the risk of impingement.
ACL remnant tissues were reported healed to the PCL, the roof of the notch, or the lateral wall in 28 of 48 (58%) patients, with no identifiable ligament tissue remaining in the other 20 (42%).10 Similarly, we observed that the ACL remnant had remained and was attached in 218 of 372 patients (59%), and the lateral wall was completely empty in 154 patients (41%). The previous classification system10 focuses on the morphology of the remnant but does not consider its volume, tension, or function. In some patients classified as having a remaining remnant, the remnant showed insufficient quality, such as loose tension, poor attachment to the femur, or a small quantity. These patients, in which the continuity of the remnant to a femur or synovial membrane covering was not complete, were classified as incomplete (group 2). To clarify the ability to predict preoperatively whether a remnant can be preserved, it is necessary to determine whether the quality and quantity of the remnant are appropriate.
Preoperative condition and postoperative outcome have been reported to differ depending on the remnant volume.23 These findings suggested that remnant volume may be an important preoperative condition and a predictor of operative outcome. Therefore, we excluded the 154 patients without a remnant in the postoperative evaluation of the clinical impact of remnant preservation. Interestingly, the 2 groups did not differ preoperatively; the period from injury to surgery was longer in group 2. A long interval from injury to surgery, even in patients with a preserved remnant, suggests that the morphology and function of the remnant were insufficient and that surgical preservation of a remnant was difficult. We suggest that a larger remnant volume in a preoperative condition may be an important factor for predicting the outcome. Furthermore, a longer interval after initial ACL injury could result in more giving-way, which may negatively affect the remnant volume.
A comparison of clinical results between ACL reconstructions with and without a preserved remnant21 defined 20% of the distance from the tibial attachment as the basis point because mechanoreceptors reside mainly in the tibial attachment.31 We focused not only on the role of mechanoreceptors but also on the vascular and tensional support of the remnant tissue. Although the previous study reported no significant difference in mechanical stability between ACL reconstructions with and without a preserved remnant, there were significant differences in functional outcome and proprioception.21 Using an arthrometer, we found that the anterior stability of the knee was significantly better in patients with than without a preserved remnant. Although we could not determine whether the difference in remnant volume affected these 2 sets of results, our findings suggested that preservation of ≥75% of a remnant contributed to anterior stability.
The loss of proprioception after a ligament injury results in changes in gait and deterioration of position sense. Altered biomechanics and neuromuscular function resulting from the initial ACL injury can affect leg kinematics. Patients are greatly dismayed to face repeat surgery and the long process of rehabilitation after having successfully completed this process previously. At a 2-year follow-up, the risk of ACL graft rupture has been found to range from 2% to 5%.34,37 In corroboration with these reports, in our study, ACL graft rupture was found in 8 of 183 patients (4.3%), 1 (1.1%) in group 1 and 7 (7.1%) in group 2, over a 2-year follow-up period. Regression analysis revealed that the only significant predictor of graft rupture was nonpreservation of the remnant (odds ratio, 11.2; 95% CI, 1.1-94.5). Mechanoreceptors have been observed 3 years after injury in patients with an ACL remnant adapted to the PCL.14 We did not measure proprioception, but a possible explanation for the lower rate of graft rupture that we found in the remnant preserving group is that better proprioception reduced the risk of rerupture.
This study had several limitations. First, the 2-year follow-up period was insufficient, although Salmon et al30 reported that ACL graft ruptures were found to occur in 39 of 675 patients (6%) at a median 20 months (95% CI, 15-25 months) after the index surgery. A longer term follow-up may reveal additional clinical results. Second, several surgeons made intraoperative observations during reconstruction involving remnant preservation However, all the surgeons in this study had ≥10 years of experience as a knee surgery specialist at the same hospital. Third, our definition of the ability to preserve the remnant was not completely objective, and there was inherent selection bias in dividing the patients between 2 groups. It was difficult to be objectively quantified but that might have influenced the rerupture rate. Future studies should evaluate the quality and quantity of the remnant before surgery. Fourth, we did not measure functional outcome scores. However, postoperative Tegner score changes on return to sport activity in both groups were 0.5 points or less. Nevertheless the rate of graft rupture was lower in the remnant preserving group. Finally, we did not evaluate proprioception or the graft remodeling process in analyzing the function and morphology of the remnant.
Despite these limitations, however, this study has clarified that preserving the ACL remnant tissue has several clinical advantages, such as decreasing graft rupture after primary reconstruction, thereby decreasing the likelihood of repeat injury in athletes.
Supplementary Material
Footnotes
A Video Supplement for this article is available at http://ojsm.sagepub.com/supplemental.
The authors declared that they have no conflicts of interest in the authorship and publication of this contribution.
References
- 1. Adachi N, Ochi M, Uchio Y, Sumen Y. Anterior cruciate ligament augmentation under arthroscopy. A minimum 2-year follow-up in 40 patients. Arch Orthop Trauma Surg. 2000;120:128–133. [DOI] [PubMed] [Google Scholar]
- 2. Aglietti P, Giron F, Buzzi R, Biddau F, Sasso F. Anterior cruciate ligament reconstruction: bone-patellar tendon-bone compared with double semitendinosus and gracilis tendon grafts. A prospective, randomized clinical trial. J Bone Joint Surg Am. 2004;86:2143–2155. [PubMed] [Google Scholar]
- 3. Ahn JH, Lee YS, Ha HC. Anterior cruciate ligament reconstruction with preservation of remnant bundle using hamstring autograft: technical note. Arch Orthop Trauma Surg. 2009;129:1011–1015. [DOI] [PubMed] [Google Scholar]
- 4. Arnoczky SP. Blood supply to the anterior cruciate ligament and supporting structures. Orthop Clin North Am. 1985;16:15–28. [PubMed] [Google Scholar]
- 5. Bach BR, Jr, Tradonsky S, Bojchuk J, Levy ME, Bush-Joseph CA, Khan NH. Arthroscopically assisted anterior cruciate ligament reconstruction using patellar tendon autograft. Five- to nine-year follow-up evaluation. Am J Sports Med. 1998;26:20–29. [DOI] [PubMed] [Google Scholar]
- 6. Barrett DS. Proprioception and function after anterior cruciate reconstruction. J Bone Joint Surg Br. 1991;73:833–837. [DOI] [PubMed] [Google Scholar]
- 7. Beynnon BD, Johnson RJ, Fleming BC, et al. Anterior cruciate ligament replacement: comparison of bone-patellar tendon-bone grafts with two-strand hamstring grafts. A prospective, randomized study. J Bone Joint Surg Am. 2002;84-A:1503–1513. [DOI] [PubMed] [Google Scholar]
- 8. Buda R, Ferruzzi A, Vannini F, Zambelli L, Di Caprio F. Augmentation technique with semitendinosus and gracilis tendons in chronic partial lesions of the ACL: clinical and arthrometric analysis. Knee Surg Sports Traumatol Arthrosc. 2006;14:1101–1107. [DOI] [PubMed] [Google Scholar]
- 9. Corry IS, Webb JM, Clingeleffer AJ, Pinczewski LA. Arthroscopic reconstruction of the anterior cruciate ligament. A comparison of patellar tendon autograft and four-strand hamstring tendon autograft. Am J Sports Med. 1999;27:444–454. [DOI] [PubMed] [Google Scholar]
- 10. Crain EH, Fithian DC, Paxton EW, Luetzow WF. Variation in anterior cruciate ligament scar pattern: does the scar pattern affect anterior laxity in anterior cruciate ligament-deficient knees? Arthroscopy. 2005;21:19–24. [DOI] [PubMed] [Google Scholar]
- 11. Denti M, Monteleone M, Berardi A, Panni AS. Anterior cruciate ligament mechanoreceptors. Histologic studies on lesions and reconstruction. Clin Orthop Relat Res. 1994;(308):29–32. [PubMed] [Google Scholar]
- 12. Dhillon MS, Bali K, Vasistha RK. Immunohistological evaluation of proprioceptive potential of the residual stump of injured anterior cruciate ligaments (ACL). Int Orthop. 2010;34:737–741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Galway HR, MacIntosh DL. The lateral pivot shift: a symptom and sign of anterior cruciate ligament insufficiency. Clin Orthop Relat Res. 1980;(147):45–50. [PubMed] [Google Scholar]
- 14. Georgoulis AD, Pappa L, Moebius U, et al. The presence of proprioceptive mechanoreceptors in the remnants of the ruptured ACL as a possible source of re-innervation of the ACL autograft. Knee Surg Sports Traumatol Arthrosc. 2001;9:364–368. [DOI] [PubMed] [Google Scholar]
- 15. Gohil S, Annear PO, Breidahl W. Anterior cruciate ligament reconstruction using autologous double hamstrings: a comparison of standard versus minimal debridement techniques using MRI to assess revascularization. A randomized prospective study with a one-year follow-up. J Bone Joint Surg Br. 2007;89:1165–1171. [DOI] [PubMed] [Google Scholar]
- 16. Gomez-Barrena E, Nunez A, Ballesteros R, Martinez-Moreno E, Munuera L. Anterior cruciate ligament reconstruction affects proprioception in the cat’s knee. Acta Orthop Scand. 1999;70:185–193. [DOI] [PubMed] [Google Scholar]
- 17. Junkin DM, Jr, Johnson DL. ACL tibial remnant, to save or not? Orthopedics. 2008;31:154–159. [DOI] [PubMed] [Google Scholar]
- 18. Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16:494–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Kim S-G, Kurosawa H, Sakuraba K, Ikeda H, Takazawa S, Takazawa Y. Development and application of an inside-to-out drill bit for anterior cruciate ligament reconstruction. Arthroscopy. 2005;21:1012.e1–1012.e4. [DOI] [PubMed] [Google Scholar]
- 20. Lee BI, Min KD, Choi HS, Kim JB, Kim ST. Arthroscopic anterior cruciate ligament reconstruction with the tibial-remnant preserving technique using a hamstring graft. Arthroscopy. 2006;22:340 e1–340.e7. [DOI] [PubMed] [Google Scholar]
- 21. Lee BI, Kwon SW, Kim JB, Choi HS, Min KD. Comparison of clinical results according to amount of preserved remnant in arthroscopic anterior cruciate ligament reconstruction using quadrupled hamstring graft. Arthroscopy. 2008;24:560–568. [DOI] [PubMed] [Google Scholar]
- 22. Löcherbach C, Zayni R, Chambat P, Sonnery-Cottet B. Biologically enhanced ACL reconstruction. Orthop Traumatol Surg Res. 2010;96:810–815. [DOI] [PubMed] [Google Scholar]
- 23. Muneta T, Koga H, Ju YJ, Horie M, Nakamura T, Sekiya I. Remnant volume of anterior cruciate ligament correlates preoperative patients’ status and postoperative outcome. Knee Surg Sports Traumatol Arthrosc. 2013;21:906–913. [DOI] [PubMed] [Google Scholar]
- 24. Noyes FR, Butler DL, Paulos LE, Grood ES. Intra-articular cruciate reconstruction. I: Perspectives on graft strength, vascularization, and immediate motion after replacement. Clin Orthop Relat Res. 1983;(172):71–77. [PubMed] [Google Scholar]
- 25. Ochi M, Adachi N, Deie M, Kanaya A. Anterior cruciate ligament augmentation procedure with a 1-incision technique: anteromedial bundle or posterolateral bundle reconstruction. Arthroscopy. 2006;22:463 e1–5. [DOI] [PubMed] [Google Scholar]
- 26. Ochi M, Adachi N, Uchio Y, et al. A minimum 2-year follow-up after selective anteromedial or posterolateral bundle anterior cruciate ligament reconstruction. Arthroscopy. 2009;25:117–122. [DOI] [PubMed] [Google Scholar]
- 27. Ochi M, Abouheif MM, Kongcharoensombat W, Nakamae A, Adachi N, Deie M. Double bundle arthroscopic anterior cruciate ligament reconstruction with remnant preserving technique using a hamstring autograft. Sports Med Arthrosc Rehabil Ther Technol. 2011;3:30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Ochi M, Iwasa J, Uchio Y, Adachi N, Sumen Y. The regeneration of sensory neurones in the reconstruction of the anterior cruciate ligament. J Bone Joint Surg Br. 1999;81:902–906. [DOI] [PubMed] [Google Scholar]
- 29. Ohsawa T, Kimura M, Kobayashi Y, Hagiwara K, Yorifuji H, Takagishi K. Arthroscopic evaluation of preserved ligament remnant after selective anteromedial or posterolateral bundle anterior cruciate ligament reconstruction. Arthroscopy. 2012;28:807–817. [DOI] [PubMed] [Google Scholar]
- 30. Salmon L, Russell V, Musgrove T, Pinczewski L, Refshauge K. Incidence and risk factors for graft rupture and contralateral rupture after anterior cruciate ligament reconstruction. Arthroscopy. 2005;21:948–957. [DOI] [PubMed] [Google Scholar]
- 31. Schutte MJ, Dabezies EJ, Zimny ML, Happel LT. Neural anatomy of the human anterior cruciate ligament. J Bone Joint Surg Am. 1987;69:243–247. [PubMed] [Google Scholar]
- 32. Shelbourne KD, Gray T, Haro M. Incidence of subsequent injury to either knee within 5 years after anterior cruciate ligament reconstruction with patellar tendon autograft. Am J Sports Med. 2009;37:246–251. [DOI] [PubMed] [Google Scholar]
- 33. Sonnery-Cottet B, Lavoie F, Ogassawara R, Scussiato RG, Kidder JF, Chambat P. Selective anteromedial bundle reconstruction in partial ACL tears: a series of 36 patients with mean 24 months follow-up. Knee Surg Sports Traumatol Arthrosc. 2010;18:47–51. [DOI] [PubMed] [Google Scholar]
- 34. Spindler KP, Kuhn JE, Freedman KB, Matthews CE, Dittus RS, Harrell FE., Jr Anterior cruciate ligament reconstruction autograft choice: bone-tendon-bone versus hamstring: does it really matter? A systematic review. Am J Sports Med. 2004;32:1986–1995. [DOI] [PubMed] [Google Scholar]
- 35. Tegner Y, Lysholm J. Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res. 1985;(198):43–49. [PubMed] [Google Scholar]
- 36. Wright RW, Magnussen RA, Dunn WR, Spindler KP. Ipsilateral graft and contralateral ACL rupture at five years or more following ACL reconstruction: a systematic review. J Bone Joint Surg Am. 2011;93:1159–1165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Wright RW, Dunn WR, Amendola A, et al. Risk of tearing the intact anterior cruciate ligament in the contralateral knee and rupturing the anterior cruciate ligament graft during the first 2 years after anterior cruciate ligament reconstruction: a prospective MOON cohort study. Am J Sports Med. 2007;35:1131–1134. [DOI] [PubMed] [Google Scholar]
- 38. Yasuda K, Kondo E, Kitamura N, Kawaguchi Y, Kai S, Tanabe Y. A pilot study of anatomic double-bundle anterior cruciate ligament reconstruction with ligament remnant tissue preservation. Arthroscopy. 2012;28:343–353. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.