Abstract
Background:
A majority of studies investigating the role of the ligamentum teres (LT) have focused primarily on anatomical and histological descriptions. To date, however, the structural properties of the LT have yet to be fully elucidated.
Purpose:
To investigate the structural properties of the native LT in a human cadaveric model.
Study Design:
Descriptive laboratory study.
Methods:
A total of 12 human cadaveric hemipelvises (mean age, 53.6 years; range, 34-63 years) were dissected free of all extra-articular soft tissues to isolate the LT and its acetabular and femoral attachments. A dynamic tensile testing machine distracted each femur in line with the fibers of the LT at a displacement-controlled rate of 0.5 mm/s. The anatomic dimensions, structural properties, and modes of failure were recorded.
Results:
The LT achieved a mean yield load of 75 N and ultimate failure load of 204 N. The LT had mean lengths of 38.0 and 53.0 mm at its yield and failure points, respectively. The most common (75% of specimens) mechanism of failure was tearing at the fovea capitis. On average, the LT had a linear stiffness of 16 N/mm and elastic modulus of 9.24 MPa. The mean initial length and cross-sectional area were 32 mm and 59 mm2, respectively.
Conclusion:
The human LT had a mean ultimate failure load of 204 N. Therefore, the results of this investigation, combined with recent biomechanical and outcomes studies, suggest that special consideration should be given to preserving the structural and corresponding biomechanical integrity of the LT during surgical intervention.
Clinical Relevance:
The LT may be more important as a static stabilizer of the hip joint than previously recognized. Further studies are recommended to investigate the appropriate indications to perform surgical repair or reconstruction of the LT for preservation of hip stability and function.
Keywords: hip, ligaments, lower extremity, tensile strength, ligamentum teres, biomechanics
Surgical treatment of the ligamentum teres (LT) is an option for addressing hip instability and pain that persists in the absence of more common intra-articular pathology.1,14,19,23 While multiple surgical reconstruction techniques have been proposed,1,14,17,19 there is controversy regarding the exact role played by the LT in preserving a stable hip joint. Several studies have attempted to clarify the characteristics of the LT; however, their results have yet to define a specific purpose or function.2,5,6,8,9,15,16,20,25
Anatomically, the LT is reported to be variable in length7,9,25 and absent in 10% of individuals,24 and it consists of either multiple bands or bundles.9,20 The functional properties of the LT are also not fully understood. Multiple studies have reported that the LT becomes most taut in flexion, adduction, and external rotation.2,9,11,20 In contrast, others have suggested that maximal tension occurs during flexion and abduction.12,16 Martin et al15 recently reported on the stabilizing role of the LT when capsular ligaments are present. In their study, an increase in internal and external rotation of the hip was observed after arthroscopic sectioning of the LT, especially with the hip in 90° of flexion. In a biomechanical investigation of the porcine LT, Wenger et al27 reported failure occurring at either the acetabulum or fovea capitis at a mean load of 882 N. Another study by Chen et al7 reported an ultimate failure load of isolated human LTs to be between 130 and 234 N. Their methodology focused primarily on testing the strength of the isolated LT fibers and did not analyze the LT with its native attachments to the acetabulum and femur left intact. As a result, the mechanism and site of LT rupture during biomechanical testing remains unknown.
Therefore, the purpose of the current study was to investigate the structural properties of the native LT in a human cadaveric model. We aimed to describe yield load, ultimate failure load, yield strength, ultimate tensile strength, displacement, linear stiffness, elastic modulus, and mode of failure. The results from this study will help elucidate the structural properties of the LT and provide a framework for future biomechanical reconstruction testing and clinical outcome studies.
Materials and Methods
Specimen Preparation
Twelve male human cadaveric hemipelvises (mean age, 53.6 years; range, 34-63 years) were used in this study. Male specimens were chosen to ensure consistent bone quality. Specimens had no history of reported hip injury or surgery. All extra-articular soft tissues were removed to expose the femoral head, acetabulum, labrum, transverse acetabular ligament, and LT. The transverse acetabular ligament was maintained due to the corresponding attachments of the LT. On visualization, the LT was inspected for abnormalities, and only intact ligaments were tested. Any specimen with evidence of a complete or partial LT tear was excluded. Specimens were excluded in 2 cases due to a complete lack of the LT (not included in specimen demographics). An oscillating bone saw was used to isolate the acetabulum from the remainder of the hemipelvis. Cuts along the proximal border of the acetabulum were initiated at the greater sciatic notch and extended anteriorly to the anterior inferior iliac spine. Distal cuts were made near the lower acetabular rim through the ischial spine, posteriorly, and through the superior ramus of the pubis, anteriorly. The bone saw was also used to transect the femoral diaphysis at a distance of 10 cm distal to the most lateral surface of the greater trochanter. This point was chosen to ensure that a consistent distance of 3 cm existed between the potting and greater trochanter across all tested specimens. Specimens were stored at –20°C until the day prior to testing. Specimens were thawed 24 hours prior to biomechanical testing, and both the acetabulum and femur were potted in a cylindrical mold using poly(methyl methacrylate) (PMMA; Fricke Dental).
Biomechanical Testing
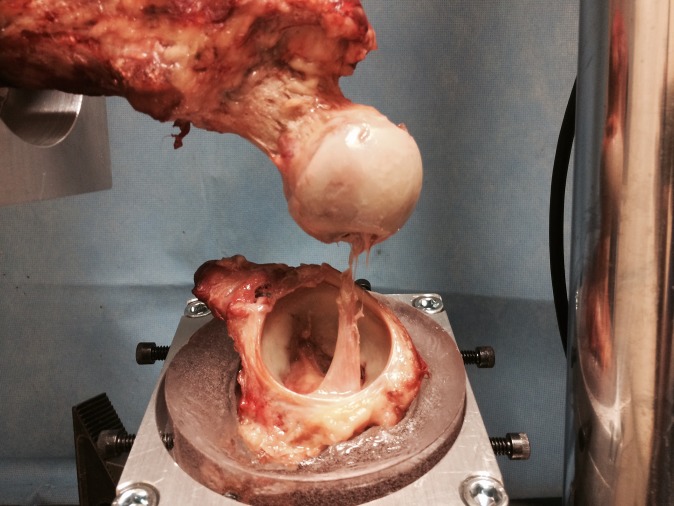
Structural properties of the LT were evaluated in response to a load-to-failure protocol using a dynamic tensile testing system (ElectroPuls E10000; Instron). Measurement error of the testing system was certified by Instron to be less than or equal to ±0.01 mm and ±0.3% of the indicated force. The potted acetabulum was secured within a custom ball and socket fixture rigidly clamped to the base platform of the testing system, and the potted femur was similarly secured to the actuator of the testing system (Figure 1). The location of the LT footprint on the femoral head and acetabulum was observed during pilot testing to vary considerably; therefore, custom ball and socket fixtures were fabricated to provide increased degrees of freedom during alignment positioning and ensured that the tensile force was applied in line with the fibers of the LT, placing these fibers in a position of maximal vulnerability throughout testing.
Figure 1.

Biomechanical testing setup for a right hip. The femur was attached to the actuator (A) of the dynamic tensile testing machine while secured within a custom ball and socket alignment fixture (B). Similarly, the acetabulum was secured within a custom ball and socket alignment fixture (C) rigidly mounted to the base platform. The use of ball and socket fixtures for alignment positioning ensured that the tensile force was applied in line with the fibers of the ligamentum teres, placing these fibers in a position of maximal vulnerability throughout testing.
Following alignment, a 5-N tensile preload was applied to the specimen to permit tissue equilibration. While under this load, the length and cross-sectional area of the LT were recorded using a coordinate measuring device (MicroScribe-MX; GoMeasure3D) with a single point accuracy of 0.358 mm. Initial length was determined by measuring the LT from its attachment to the acetabulum near the transverse ligament to its insertion on the fovea capitis of the femur. To calculate the cross-sectional area, 24 peripheral points were collected at a visually determined point halfway between the acetabular and femoral attachments. Heron's formula was then used to calculate the cross-sectional area.18 Data collection for the cross-sectional area was completed in triplicate at the same location on the LT, and the resulting calculated areas were averaged. The LT was then displaced under tension at 0.5 mm/s until failure.27 Yield load (N) and strength (MPa), displacement at yield (mm), ultimate failure load (N) and strength (MPa), displacement at failure (mm), stiffness (N/mm), and elastic modulus (MPa) were measured or calculated. The mode of failure was recorded and classified as failure at the fovea capitis, cotyloid fossa, or midsubstance.
Results
Qualitative and Quantitative Anatomic Analysis
The LT had a mean initial length of 32 ± 5 mm and cross-sectional area of 59 ± 22 mm2 (Table 1). By visual observation, all 12 LT specimens appeared as a ribbon-like structure at the acetabulum with anchoring points medially at the transverse ligament, anteriorly at the pubic side of the acetabular notch, and posteriorly at the ischial side of the acetabular notch (Figure 2). Moving distally, there was a confluence of the fibers at the fovea capitis of the femur. Throughout the midsubstance up to the attachment at the fovea capitis, no distinct bundles were visually observed or discerned on manual palpation.
TABLE 1.
Anatomic and Structural Properties of the Ligamentum Teresa
| Dimension | |
| Length, mm | 32 ± 5 |
| Cross-sectional area, mm2 | 59 ± 22 |
| Structural property | |
| Yield load, N | 75 ± 30 |
| Yield strength, MPa | 1.36 ± 0.61 |
| Displacement at yield, mm | 5.69 ± 2.28 |
| Ultimate load, N | 204 ± 128 |
| Tensile strength, MPa | 3.30 ± 1.60 |
| Displacement at failure, mm | 20.56 ± 10.22 |
| Linear stiffness, N/mm | 16 ± 6 |
| Elastic modulus, MPa | 9.24 ± 3.14 |
aValues are reported as mean ± SD.
Figure 2.

Attachment locations of the ligamentum teres on the acetabulum in a right hip. Arrows denote the attachment band. (A) Superficial medial attachment to the transverse ligament. (B) Deep posterior attachment to the ischial side of the acetabular notch. (C) Deep anterior attachment to the pubic side of the acetabular notch.
Load to Failure
At its yield point, the LT displaced 5.69 ± 2.28 mm and reached a load of 75 ± 30 N. The LT displaced 20.56 ± 10.22 mm and reached a mean ultimate failure load of 204 ± 128 N prior to failure. Additional structural properties of the native LT are provided in Table 1. The most common mode of failure was intrasubstance tearing of the LT at the fovea capitis (9 of 12 specimens) (Figure 3); however, additional mechanisms were also observed (Table 2).
Figure 3.
A left hip displaying the most common mode of failure during biomechanical testing. Of 12 tested specimens, 9 failed due to intrasubstance tearing of the ligamentum teres at a location near the fovea capitis.
TABLE 2.
Mechanism of Failure for Each Specimen
| Specimen | Mechanism of Failure |
|---|---|
| 1 | Avulsion at fovea capitis |
| 2 | Intrasubstance tearing at fovea capitis |
| 3 | Acetabular peel-off |
| 4 | Acetabular peel-off followed by intrasubstance tearing at fovea capitis |
| 5 | Intrasubstance tearing at fovea capitis |
| 6 | Acetabular peel-off followed by midsubstance tear |
| 7 | Intrasubstance tearing at fovea capitis |
| 8 | Intrasubstance tearing at fovea capitis |
| 9 | Intrasubstance tearing at fovea capitis |
| 10 | Acetabular peel-off followed by intrasubstance tearing at fovea capitis |
| 11 | Acetabular peel-off followed by intrasubstance tearing at fovea capitis |
| 12 | Intrasubstance tearing at fovea capitis |
Discussion
The most important finding of the current study was that the native, human LT could withstand a mean ultimate failure load of 204 N when subjected to tensile loading in line with its fibers. Additionally, the mean lengths at yield and failure were 38.0 and 53.0 mm, respectively, suggesting that the minimal displacement that occurs during distraction for arthroscopic hip surgery would likely not injure the LT. The manner in which the LT was tested, with its acetabular and femoral attachments intact, provided unique insight into the mechanism of injury during the load-to-failure testing protocol. The most common failure mechanism observed was intrasubstance tearing of the LT near the fovea capitis.
The mean ultimate failure load (204 N) observed in the current study for human cadaveric specimens was similar to that reported in a previous ex vivo study.7 During their investigation of the LT in patients with acute fracture of the femoral neck and ischemic necrosis of the femoral head, Chen et al7 reported ultimate failure loads of 234 and 130 N, respectively. However, there are several notable differences between our study and theirs. For example, Chen et al7 isolated and tested the LT within mechanical clamps, thus precluding the additional modes of failure observed in our study (eg, acetabular peel-off, avulsion at the fovea capitis). Notably, by keeping the distinct attachments intact, the current study detected yield loads in all specimens prior to complete rupture. Additionally, in contrast to our study, the intracapsular hematoma of a femoral neck fracture or avascular necrosis of the femoral head may have altered the intrinsic, biomechanical properties of the tested LT specimens from Chen et al.7 Nevertheless, the structural properties and dimensions were quite similar between our study and prior investigations.7,9,25
The relatively low ultimate failure load of the LT suggests that it may be easily injured if other important primary stabilizers are also injured. A technique described by Ganz et al10 involved purposefully disrupting the LT during surgical dislocation of the hip in open management of femoroacetabular impingement when gaining access to the acetabular rim. However, the results of this current study suggest that surgical distraction should not cause complete rupture of the LT. During surgical distraction, a traction force of 110 to 225 N is commonly used to separate the joint up to 10 mm.3,4 Although the mean yield and ultimate failure loads were below the upper end of the range for applied traction load, the average length of the LT at yield (38.0 mm) and failure (53.0 mm) exceeded the reported separation distance (10 mm) of the joint during distraction. Additionally, it is important to note that the femur was disarticulated in a lateral direction during load-to-failure testing in this study, which is different than inferior displacement of the femur during surgical distraction. Furthermore, the capsular ligaments and other soft tissue stabilizers present in vivo likely reduce the magnitude of the force transmitted to the LT during hip distraction.
In cases of traumatic posterior dislocation or chronic subluxation due to dysplasia, it may be necessary to evaluate the integrity of the LT during arthroscopic intervention. In a recent study, Martin et al15 reported that complete rupture of the LT leads to substantial increases in internal (12°) and external rotation (18°) range of motion, especially at 90° and 120° of flexion. In addition to providing stability to the hip, it has been suggested that the LT also plays a role in nociception and proprioception due to the presence of free nerve endings.13,22 As a result, there should be consideration toward maintaining the LT during surgical intervention to preserve native hip kinematics and function. Traditionally, the LT was considered a vestigial structure lacking a pivotal role in the hip and was commonly excised during open reduction of dysplastic pediatric patients,21,26 but in light of our results and recent biomechanical and surgical reconstruction outcomes studies,1,2,9,14,15,17,19 it may have a larger role than previously recognized.
We acknowledge the presence of limitations in the current study. First, the older population of cadaveric specimens may underestimate the strength of the LT in younger populations. Additional investigations into the biomechanical properties of the LT from a younger population, as well as those from dysplastic hips, would be informative to discern whether the LT has a larger role in development and early childhood. Second, the manner in which the tensile force was applied to the LT may not be entirely representative of the functional nature of the LT in vivo, which has only recently been suggested to be a restraint to internal and external rotation during deep flexion.15 However, the aim of this study was to provide a biomechanical foundation on which further studies could be based. In addition, these forces may not represent the vector of force applied to the LT during a physiologic dislocation event. Future studies should focus on defining the exact in vivo anatomical nature of the LT during injury, and specifically while the hip is in traction during hip arthroscopy. Finally, given that our study used a cadaveric model, continued assessments of the in vivo biomechanical role should be pursued to refine the understanding of the LT’s role in a normal hip.
Conclusion
The human LT was able to withstand a mean ultimate failure load of 204 N. The results of this investigation, combined with recent biomechanical and outcomes studies, suggest that special consideration should be given to preserving the structural and corresponding structural integrity of the LT during surgical intervention.
Acknowledgment
The authors thank Barry Eckhaus for his assistance with medical photography.
Footnotes
The authors declared that they have no conflicts of interest in the development and publication of this contribution.
References
- 1. Amenabar T, O’Donnell J. Arthroscopic ligamentum teres reconstruction using semitendinosus tendon: surgical technique and an unusual outcome. Arthrosc Tech. 2012;1:e169–e174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Bardakos NV, Villar RN. The ligamentum teres of the adult hip. J Bone Joint Surg Br. 2009;91:8–15. [DOI] [PubMed] [Google Scholar]
- 3. Byrd JW. Hip arthroscopy. The supine position. Clin Sports Med. 2001;20:703–731. [PubMed] [Google Scholar]
- 4. Byrd JW, Chern KY. Traction versus distension for distraction of the joint during hip arthroscopy. Arthroscopy. 1997;13:346–349. [DOI] [PubMed] [Google Scholar]
- 5. Byrd JW, Jones KS. Traumatic rupture of the ligamentum teres as a source of hip pain. Arthroscopy. 2004;20:385–391. [DOI] [PubMed] [Google Scholar]
- 6. Cerezal L, Kassarjian A, Canga A, et al. Anatomy, biomechanics, imaging, and management of ligamentum teres injuries. Radiographics. 2010;30:1637–1651. [DOI] [PubMed] [Google Scholar]
- 7. Chen HH, Li AF, Li KC, Wu JJ, Chen TS, Lee MC. Adaptations of ligamentum teres in ischemic necrosis of human femoral head. Clin Orthop Relat Res. 1996;(328):268–275. [DOI] [PubMed] [Google Scholar]
- 8. Delcamp DD, Klaaren HE, Pompe van Meerdervoort HF. Traumatic avulsion of the ligamentum teres without dislocation of the hip. Two case reports. J Bone Joint Surg Am. 1988;70:933–935. [PubMed] [Google Scholar]
- 9. Demange MK, Kakuda CMS, Pereira CAM, Sakaki MH, Albuquerque RFM. Influence of the femoral head ligament on hip mechanical function. Acta Ortop Bras. 2007;15:187–190. [Google Scholar]
- 10. Ganz R, Gill TJ, Gautier E, Ganz K, Krugel N, Berlemann U. Surgical dislocation of the adult hip a technique with full access to the femoral head and acetabulum without the risk of avascular necrosis. J Bone Joint Surg Br. 2001;83:1119–1124. [DOI] [PubMed] [Google Scholar]
- 11. Kelly BT, Williams RJ, 3rd, Philippon MJ. Hip arthroscopy: current indications, treatment options, and management issues. Am J Sports Med. 2003;31:1020–1037. [DOI] [PubMed] [Google Scholar]
- 12. Kivlan BR, Richard Clemente F, Martin RL, Martin HD. Function of the ligamentum teres during multi-planar movement of the hip joint. Knee Surg Sports Traumatol Arthrosc. 2013;21:1664–1668. [DOI] [PubMed] [Google Scholar]
- 13. Leunig M, Beck M, Stauffer E, Hertel R, Ganz R. Free nerve endings in the ligamentum capitis femoris. Acta Orthop Scand. 2000;71:452–454. [DOI] [PubMed] [Google Scholar]
- 14. Lindner D, Sharp KG, Trenga AP, Stone J, Stake CE, Domb BG. Arthroscopic ligamentum teres reconstruction. Arthrosc Tech. 2013;2:e21–e25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Martin HD, Hatem MA, Kivlan BR, Martin RL. Function of the ligamentum teres in limiting hip rotation: a cadaveric study. Arthroscopy. 2014;30:1085–1091. [DOI] [PubMed] [Google Scholar]
- 16. Martin RL, Kivlan BR, Clemente FR. A cadaveric model for ligamentum teres function: a pilot study. Knee Surg Sports Traumatol Arthrosc. 2013;21:1689–1693. [DOI] [PubMed] [Google Scholar]
- 17. Mei-Dan O, McConkey MO, Brick M. Catastrophic failure of hip arthroscopy due to iatrogenic instability: can partial division of the ligamentum teres and iliofemoral ligament cause subluxation? Arthroscopy. 2012;28:440–445. [DOI] [PubMed] [Google Scholar]
- 18. Nelsen RB. Heron’s formula via proofs without words. Coll Math J. 2001;32:290–292. [Google Scholar]
- 19. Philippon MJ, Pennock A, Gaskill TR. Arthroscopic reconstruction of the ligamentum teres: technique and early outcomes. J Bone Joint Surg Br. 2012;94:1494–1498. [DOI] [PubMed] [Google Scholar]
- 20. Rao J, Zhou YX, Villar RN. Injury to the ligamentum teres. Mechanism, findings, and results of treatment. Clin Sports Med. 2001;20:791–799. [DOI] [PubMed] [Google Scholar]
- 21. Salter RB. Role of innominate osteotomy in the treatment of congenital dislocation and subluxation of the hip in the older child. J Bone Joint Surg Am. 1966;48:1413–1439. [PubMed] [Google Scholar]
- 22. Sarban S, Baba F, Kocabey Y, Cengiz M, Isikan UE. Free nerve endings and morphological features of the ligamentum capitis femoris in developmental dysplasia of the hip. J Pediatr Orthop B. 2007;16:351–356. [DOI] [PubMed] [Google Scholar]
- 23. Shetty VD, Villar RN. Hip arthroscopy: current concepts and review of literature. Br J Sports Med. 2007;41:64–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Tan CK, Wong WC. Absence of the ligament of head of femur in the human hip joint. Singapore Med J. 1990;31:360–363. [PubMed] [Google Scholar]
- 25. Walker JM. Growth characteristics of the fetal ligament of the head of femur: significance in congenital hip disease. Yale J Biol Med. 1980;53:307–316. [PMC free article] [PubMed] [Google Scholar]
- 26. Weinstein SL, Ponseti IV. Congenital dislocation of the hip. J Bone Joint Surg Am. 1979;61:119–124. [PubMed] [Google Scholar]
- 27. Wenger D, Miyanji F, Mahar A, Oka R. The mechanical properties of the ligamentum teres: a pilot study to assess its potential for improving stability in children’s hip surgery. J Pediatr Orthop. 2007;27:408–410. [DOI] [PubMed] [Google Scholar]