Abstract
Objective
To estimate the burden of pregnancy-related mortality resulting from influenza A (H1N1) pdm09 virus infection during the 2009–2010 pandemic influenza season.
Methods
Data from the Centers for Disease Control and Prevention's Pregnancy Mortality Surveillance System were used to identify women whose death during or shortly after pregnancy was attributed or likely attributed to the influenza A (H1N1)pdm09 virus from April 15, 2009, through June 30, 2010. We report the characteristics of these women and enumerate cases resulting in death as the pandemic began, peaked, and resolved.
Results
During the pandemic season, we identified 915 pregnancy-related deaths and 4,911,297 live births. Seventy-five (8.2%) women died as a result of confirmed influenza A (H1N1) pdm09 infection deaths and 34 (3.7%) women as a result of possible influenza A (H1N1)pdm09 infection deaths. The pregnancy-related mortality ratio for confirmed and possible (combined) influenza A (H1N1) pdm09 infection deaths was 2.2 per 100,000 live births. Most deaths occurred during the 2009 calendar year with the peak of the distribution of deaths over time occurring in October 2009.
Conclusion
Twelve percent of pregnancy-related deaths were attributed to confirmed or possible influenza A (H1N1) pdm09 infection during the 2009–2010 pandemic season. Because prediction of pandemics is difficult, planning for prevention of influenza and care for those women affected are critical for preventing associated severe maternal morbidity and mortality.
In April of 2009, a novel strain of influenza of swine origin was first detected in the United States and characterized as influenza A (H1N1) pdm09 virus.1 By the end of April, the Centers for Disease Control and Prevention's (CDC) Emergency Operations Center was activated and a nationwide public health emergency was declared as a result of the outbreak of this pandemic strain.2 The second reported death from influenza A (H1N1)pdm09 virus infection occurred in an otherwise healthy pregnant woman.3,4 It subsequently became apparent that pregnant women were disproportionately affected by severe influenza disease resulting in significant morbidity and mortality.5–7 Surveillance data for influenza A (H1N1)pdm09 virus infection among pregnant women admitted to intensive care units reported to the CDC between April 2009 and December 31, 2009, identified 280 intensive care unit admissions, 56 of whom died.8
The CDC's Pregnancy Mortality Surveillance System has been providing nationwide information on pregnancy-related deaths since 1986. In light of the burden of influenza A (H1N1)pdm09 virus infection for pregnant and postpartum women previously reported,9 we used Pregnancy Mortality Surveillance System data to assess the contribution of the pandemic to pregnancy-related mortality. This report summarizes the information about influenza A (H1N1)pdm09 virus infection deaths during and shortly after pregnancy during the 2009-2010 influenza pandemic season using the most comprehensive data about pregnancy-related mortality in the United States.
Materials and Methods
Details of the Pregnancy Mortality Surveillance System have been described elsewhere.10–12 Briefly, the Pregnancy Mortality Surveillance System attempts to find all deaths to women who die during or within 1 year of pregnancy from any cause related to or aggravated by the pregnancy or its management. Information found on deidentified vital records represents the core data for this surveillance system. The CDC's Division of Reproductive Health asks Divisions of Vital Statistics in 52 reporting areas (ie, 50 states, New York City, and Washington, DC) to send copies of death certificates for all deaths occurring during or within 1 year of pregnancy, regardless of the cause of death or the duration of pregnancy, as well as matching birth and fetal death certificates when they are available. All information is reviewed by clinically trained epidemiologists and causes of death are determined and placed into one of 10 general categories. Descriptive data are published periodically for the purpose of reporting temporal trends in pregnancy-related deaths, broad categorical causes of death, and characteristics of women who die.10,12 In this system, influenza as a cause of death is embedded in the general category of “infections.” Although deaths from influenza during or within 3 months of the end of pregnancy are considered pregnancy-related and categorized as deaths resulting from “infection,” information regarding influenza infection as the contributing cause of death from “infection” is also retained and coded in the database. For this analysis we considered two groups of influenza deaths. The first group had influenza or “H1N1” denoted as the underlying cause of death on the death certificate and were considered confirmed influenza A (H1N1) pdm09 virus infection cases. The second group had acute respiratory distress syndrome or pneumonia listed as the underlying cause of death with no other associated conditions denoted on the death certificate or linked birth or fetal death certificate (eg, postpartum hemorrhage, preeclampsia) or causative organisms denoted; this second group of deaths was designated as possible influenza A (H1N1)pdm09 virus infection deaths. Deaths initially identified as resulting from confirmed or possible influenza A (H1N1)pdm09 were independently reviewed by two authors (W.M.C. and A.A.C.) and any discrepancies were resolved by discussion. Women who died with an indication of influenza A (H1N1)pdm09 virus infection within 3 months of the end of the pregnancy or who had evidence of becoming ill with influenza within 3 months of the end of pregnancy and who died beyond 3 months were considered to have a pregnancy-related death.
Cases of influenza A (H1N1)pdm09 virus infection were first reported in the United States in April 2009. The U.S. Public Health Emergency for the pandemic expired on June 23, 2010.13 Hence, we considered all confirmed and possible influenza deaths from April 15, 2009, through June 30, 2010, as deaths that occurred during the pandemic season. The cause-specific pregnancy mortality ratio (deaths/100,000 live births) was calculated using live births identified from U.S. natality files for the pandemic season as the denominator. Cause-specific proportionate mortality (percentage of all pregnancy-related deaths resulting from influenza A [H1N1] pdm09 virus infection) was calculated using all pregnancy-related deaths in the Pregnancy Mortality Surveillance System for the pandemic season as the denominator. Basic characteristics of women who died were obtained from the demographic and obstetric data available on birth and death certificates. Characteristics of women who died from confirmed and possible influenza A (H1N1)pdm09 virus infection were compared using Fisher's exact or χ2 tests.
The data are derived from death certificates and hence fall outside the definition of human subjects. Therefore, analyses involving Pregnancy Mortality Surveillance System data are not subject to institutional review.
Results
Between April 15, 2009, and June 30, 2010, 915 pregnancy-related deaths were identified and there were 4,911,297 live births. Of the pregnancy-related deaths, 75 were classified as confirmed influenza A (H1N1)pdm09 virus infection deaths and 34 were classified as possible influenza A (H1N1)pdm09 virus infection deaths. Correspondingly, confirmed influenza A (H1N1)pdm09 virus infection deaths represented 8.2% and possible influenza A (H1N1)pdm09 virus infection deaths accounted for 3.7% of all pregnancy-related deaths. The pregnancy-related mortality ratio for confirmed and possible (combined measure) influenza A (H1N1)pdm09 virus infection deaths was 2.2 per 100,000 live births.
Among the 55 women who had live births and who died as a result of confirmed influenza A (H1N1)pdm09 virus infection, 50 had documentation of gestational age; 19 births occurred at less than 32 weeks of gestation and 12 between 32 and 36 weeks of gestation (62% preterm birth rate). Among the 24 women who had live births and who died from possible influenza A (H1N1)pdm09 virus infection, 22 had documentation of gestational age; four births occurred less than 32 weeks of gestation and six between 32 and 36 weeks of gestation (45% preterm birth rate).
There were no differences in demographic characteristics or pregnancy outcomes between women who died from confirmed or possible influenza A (H1N1)pdm09 virus infection. More than one third of women who died from influenza A (H1N1)pdm09 virus infection (using the combined measure) were 35 years old or older. Nearly one third of women who died were Hispanic. Although almost three fourths of women died after having a live birth, 12% died undelivered. Most deaths occurred during or within 6 weeks of the end of pregnancy (Table 1).
Table 1. Characteristics of Women Who Died as a Result of Confirmed and Possible Influenza A (H1N1) pdm09 Virus Infection, United States, April 15, 2009, Through June 30, 2010.
| Influenza A (H1N1)pdm09 Virus Infection | ||||
|---|---|---|---|---|
|
|
||||
| Characteristic | Confirmed (n=75) | Possible (n=34) | P | Combined Total Influenza A (H1N1)pdm09 Virus Infection (N=109) |
| Age (y) | ||||
| 20–24 | 2 (2.7) | 1 (2.9) | .941 | 3 (2.8) |
| 25–29 | 23 (30.7) | 12 (35.3) | 35 (32.1) | |
| 30–34 | 23 (30.7) | 9 (26.5) | 32 (29.4) | |
| 35 or older | 27 (36) | 12 (35.3) | 39 (35.8) | |
| Race–ethnicity | ||||
| Non-Hispanic white | 28 (37.3) | 17 (50.0) | .287 | 45 (41.3) |
| Non-Hispanic black | 17 (22.7) | 5 (14.7) | 22 (20.2) | |
| Hispanic | 26 (34.7) | 8 (23.7) | 34 (31.2) | |
| Non-Hispanic other | 4 (5.3) | 4 (11.8) | 8 (7.3) | |
| Nativity | ||||
| U.S.-born | 58 (77.3) | 26 (76.5) | .825 | 84 (77.1) |
| Foreign-born | 16 (21.3) | 8 (23.5) | 24 (22.0) | |
| Unknown | 1 (1.3) | 0 (0) | 1 (0.9) | |
| Education (y) | ||||
| Less than 12 | 16 (21.3) | 8 (23.5) | .947 | 24 (22.0) |
| 12 | 31 (41.3) | 13 (38.2) | 44 (40.4) | |
| More than 12 | 23 (30.7) | 10 (29.4) | 33 (30.3) | |
| Unknown | 5 (6.7) | 3 (8.8) | 8 (7.3) | |
| Marital status | ||||
| Married | 30 (40.0) | 20 (58.8) | .077 | 50 (45.9) |
| Unmarried | 44 (58.7) | 14 (41.2) | 58 (53.1) | |
| Unknown | 1 (1.3) | 0 (0) | 1 (0.9) | |
| Pregnancy outcome | ||||
| Undelivered | 9 (12.0) | 4 (11.7) | .733 | 13 (11.9) |
| Abortion | 0 (0) | 1 (2.9) | 1 (0.9) | |
| Live birth | 55 (73.3) | 24 (70.6) | 79 (72.5) | |
| Stillbirth | 2 (2.7) | 1 (2.9) | 3 (2.8) | |
| Ectopic | 1 (1.3) | 0 (0) | 1 (0.9) | |
| Unknown | 8 (10.7) | 4 (11.8) | 12 (11.0) | |
| Interval between end of pregnancy and death (d) | ||||
| 0–6 | 23 (30.7) | 12 (35.3) | .305 | 35 (32.1) |
| 7–41 | 32 (42.7) | 16 (47.1) | 48 (44.0) | |
| 42 or greater | 13 (17.3) | 2 (5.9) | 15 (13.8) | |
| Unknown | 7 (9.3) | 4 (11.8) | 11 (10.1) | |
Data are n (%) unless otherwise specified.
During the pandemic season, most deaths occurred during the 2009 calendar year with the peak of the distribution occurring in October and a distinct fall off beginning in December 2009 and continuing through the winter months of 2010 (Fig. 1). The small number of deaths that occurred after February 2010 (n58) were all classified as possible cases.
Fig. 1.
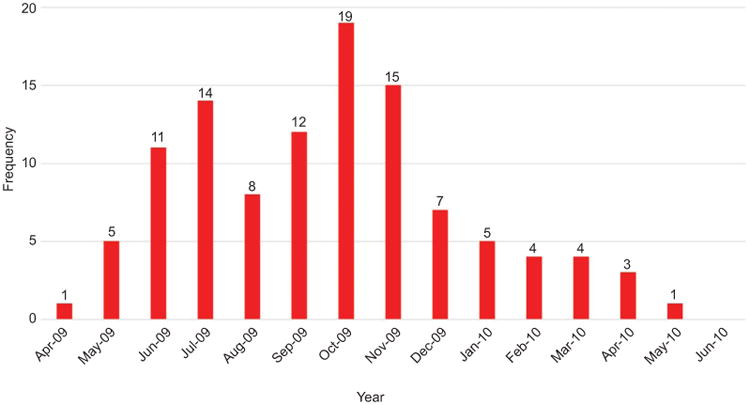
Confirmed and possible pregnancy-related deaths resulting from influenza A (H1N1)pdm09 virus infection by month, April 15, 2009, through June 30, 2010.
Discussion
The 2009–2010 influenza A (H1N1)pdm09 virus pandemic resulted in a significant burden of morbidity and mortality on pregnant women. The 109 deaths during that influenza season were more than 20 times greater than the mean number (five) of annual possible influenza deaths reported in a 1998–2005 cohort of pregnancy-related deaths resulting from seasonal influenza.14 Moreover, the 1998–2005 analysis was done during the pandemic in an effort to understand the background risk of death from influenza in non-pandemic seasons. As such, a very inclusive definition of potential seasonal influenza mortality was used to avoid underestimation in a time of widespread publicity about pandemic influenza. For the current analysis, we included only deaths in which influenza was explicitly stated on the death certificate and included a category of possible influenza only when the death was certified as resulting from a severe pulmonary cause with no mention of other organisms or acute respiratory distress syndrome without mention of contributing factors to be more certain about the attributing cause. Confirmed and possible deaths resulting from influenza A (H1N1)pdm09 virus infection constituted one in eight pregnancy-related deaths during the pandemic influenza season and represented the leading cause of pregnancy-related deaths during the 15 months considered here (12% of all pregnancy-related deaths). Information concerning the circumstances surrounding birth is limited in vital records, but the high preterm birth rate suggests that intervention may have occurred for fetal reasons, maternal reasons, or both.
The effects of the pandemic strain on pregnant women have been documented in previous pandemics including the 1918 (Spanish) influenza and the 1957 (Asian) influenza.15–19 In addition, our findings are consistent with early reports of morbidity and mortality among pregnant and postpartum women during the 2009–2010 pandemic season.3,5–7 Deaths among pregnant women resulting from influenza were reported retrospectively to the CDC by state and local health departments for the period from April through August 2009 and both retrospectively and in real time between October and December 2009 through the CDC Pregnancy Flu Line. Fifty-six such deaths occurred from April through December 2009.8
The reduction in influenza deaths beginning most strikingly in December 2009 suggests that vaccine availability and the educational campaigns by the CDC, public health agencies, and the American College of Obstetricians and Gynecologists may have had a substantial effect. Before the pandemic, in 2008, the CDC convened a meeting of experts and key partners to consider clinical management and public health actions for pregnant women during an influenza pandemic.20 The summary of this meeting was published approximately 6 months into the pandemic and informed the guidance published by the CDC highlighting the risk to pregnant women. This guidance recommended early empiric treatment with antiviral medication and reemphasized the importance of immunization.21 In addition, the American College of Obstetricians and Gynecologists used the power of their web site, e-mail, and snail mail communications and partnered with the CDC and other clinical groups to send “Dear Colleague” letters that advocated for immunization and prompt treatment of suspected cases. Data gathered through the Pregnancy Risk Assessment Monitoring System subsequently demonstrated substantially higher vaccination rates for pregnant women during the 2009 influenza pandemic compared with previous influenza seasons and that the uptake of vaccination was associated with recommendations for immunization from health care providers.22 In addition, cases in the general population peaked in late 2009 and fell off dramatically in early 2010.23
Misclassification of deaths resulting from 2009 H1N1 influenza may have occurred. The Pregnancy Mortality Surveillance System uses death certificates and, in most circumstances, linked birth and fetal death certificates to ascertain the temporal and causal relationships of death to pregnancy. However, information on vital records is rarely as precise or as clinically nuanced as information found in medical records. Hence, it is possible that some cases we classified as possible influenza A (H1N1)pdm09 deaths were the result of another cause. On the other hand, it is possible that deaths occurred and were not diagnosed as influenza or that some deaths resulting from influenza A (H1N1)pdm09 virus infection were missed because they were not appropriately attributed to pregnant or postpartum women.
The 2009–2010 influenza pandemic severely affected pregnant and postpartum women and serves as a clarion call to reinforce the efforts of public health and professional organizations to provide immunization and prompt treatment to this vulnerable group. Although influenza pandemics are not the norm, pregnant women are still at risk of morbidity and mortality from seasonal influenza; we cannot predict when the next pandemic strain will emerge. Therefore, regular annual planning for care during outbreaks of seasonal influenza is a critical strategy for ongoing prevention and preparation for subsequent pandemics.
Footnotes
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Financial Disclosure: The authors did not report any potential conflicts of interest.
References
- 1.Novel SwineOrigin Influenza A (H1N1) Virus Investigation Team. Dawood FS, Jain S, Finelli L, Shaw MW, Lindstrom S, et al. Emergence of a novel swine-origin influenza a (H1N1) virus in humans. N Engl J Med. 2009;360:2605–15. doi: 10.1056/NEJMoa0903810. [DOI] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention. The 2009 H1N1 pandemic: summary highlights, April 2009 – April 2010. Available at: http://www.cdc.gov/h1n1flu/cdcresponse.htm. Retrieved February 20, 2015.
- 3.Jamieson DJ, Honein MA, Rasmussen SA, Williams JL, Swerdlow DL, Biggerstaff MS, et al. H1N1 2009 influenza virus infection during pregnancy in the USA. Lancet. 2009;374:451–8. doi: 10.1016/S0140-6736(09)61304-0. [DOI] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention (CDC) Novel influenza A (H1N1) virus infections in three pregnant women– United States, April–May, 2009. MMWR Morb Mortal Wkly Rep. 2009;58:497–500. [PubMed] [Google Scholar]
- 5.Louie JK, Acosta M, Jamieson DJ, Honein MA California Pandemic (H1N1) Working Group . Severe 2009 H1N1 influenza in pregnant and postpartum women in California. N Engl J Med. 2010;362:27–35. doi: 10.1056/NEJMoa0910444. [DOI] [PubMed] [Google Scholar]
- 6.Saleeby E, Chapman J, Morse J, Bryant A. H1N1 influenza in pregnancy. Cause for concern. Obstet Gynecol. 2009;114:885–91. doi: 10.1097/AOG.0b013e3181bb44bb. [DOI] [PubMed] [Google Scholar]
- 7.Creanga AA, Johnson TF, Graitcer SB, Hartman LK, Al-Samarrai T, Schwarz AG, et al. Severity of 2009 pandemic influenza A (H1N1) virus infection in pregnant women. Obstet Gynecol. 2010;115:717–26. doi: 10.1097/AOG.0b013e3181d57947. [DOI] [PubMed] [Google Scholar]
- 8.Siston AM, Rasmussen SA, Honein MA, Fry AM, Seib K, Callaghan WM, et al. Pandemic 2009 influenza a (H1N1) virus illness among pregnant women in the United States. JAMA. 2010;303:1517–25. doi: 10.1001/jama.2010.479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Louie JK, Jamieson DJ, Rasmussen SA. 2009 pandemic influenza A (H1N1) virus infection in postpartum women in California. Am J Obstet Gynecol. 2011;204:144.e1–6. doi: 10.1016/j.ajog.2010.08.057. [DOI] [PubMed] [Google Scholar]
- 10.Callaghan WM. Overview of maternal mortality in the United States. Semin Perinatol. 2012;36:2–6. doi: 10.1053/j.semperi.2011.09.002. [DOI] [PubMed] [Google Scholar]
- 11.Centers for Disease Control and Prevention. Pregnancy Mortality Surveillance System. Available at: http://www.cdc.gov/reproductivehealth/MaternalInfantHealth/PMSS.html. Retrieved February 20, 2015.
- 12.Creanga AA, Berg CJ, Syverson C, Seed K, Bruce C, Callaghan WM. Pregnancy-related mortality in the United States, 2006–2010. Obstet Gynecol. 2015;125:5–12. doi: 10.1097/AOG.0000000000000564. [DOI] [PubMed] [Google Scholar]
- 13.Centers for Disease Control and Prevention. 2009 H1N1 flu. Available at: http://www.cdc.gov/h1n1flu/. Retrieved February 20, 2015.
- 14.Callaghan WM, Chu SY, Jamieson DJ. Deaths from seasonal influenza among pregnant women in the United States: 1998– 2005. Obstet Gynecol. 2010;115:919–23. doi: 10.1097/AOG.0b013e3181d99d85. [DOI] [PubMed] [Google Scholar]
- 15.Woolston WJ, Conley DO. Epidemic pneumonia (Spanish Influenza) in pregnancy: effect in one hundred and one cases. JAMA. 1918;71:1898–9. [Google Scholar]
- 16.Harris JW. Influenza occurring in pregnant women: a statistical study of thirteen hundred and fifty cases. JAMA. 1919;72:978–80. [Google Scholar]
- 17.Greenberg M, Jacobziner H, Pakter J, Weisl BA. Maternal mortality in the epidemic of Asian influenza, New York City, 1957. Am J Obstet Gynecol. 1958;76:897–902. doi: 10.1016/0002-9378(58)90027-9. [DOI] [PubMed] [Google Scholar]
- 18.Freeman DW, Barno A. Deaths from Asian influenza associated with pregnancy. Am J Obstet Gynecol. 1959;78:1172–5. doi: 10.1016/0002-9378(59)90570-8. [DOI] [PubMed] [Google Scholar]
- 19.DEATHS from Asian influenza, 1957; a report by the Public Health Laboratory Service based on records from hospital and public health laboratories. Br Med J. 1958;1:915–9. [PMC free article] [PubMed] [Google Scholar]
- 20.Rasmussen SA, Jamieson DJ, MacFarlane K, Cragan JD, Williams J, Henderson Z Pandemic Influenza and Pregnancy Working Group. Pandemic influenza and pregnant women: summary of a meeting of experts. Am J Public Health. 2009;99(suppl 2):S248–54. doi: 10.2105/AJPH.2008.152900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rasmussen SA, Jamieson DJ. 2009 H1N1 influenza and pregnancy–5 years later. N Engl J Med. 2014;371:1373–5. doi: 10.1056/NEJMp1403496. [DOI] [PubMed] [Google Scholar]
- 22.Centers for Disease Control and Prevention (CDC) Influenza vaccination coverage among pregnant women–29 states and New York City, 2009–10 season. MMWR Morb Mortal Wkly Rep. 2012;61:113–8. [PubMed] [Google Scholar]
- 23.Centers for Disease Control and Prevention (CDC) Update: influenza activity–United States, 2009–10 season. MMWR Morb Mortal Wkly Rep. 2010;59:901–8. [PubMed] [Google Scholar]


