Abstract
Introduction. Hospital readmission within 30 days of discharge is a target for health care cost savings through the medicare Value Based Purchasing initiative. Because of this focus, hospitals and health systems are investing considerable resources into the identification of patients at risk of hospital readmission and designing interventions to reduce the rate of hospital readmission. Malnutrition is a known risk factor for hospital readmission.
Materials and Methods. All medical patients 65 years of age or older discharged from Memorial Medical Center from January 1, 2012 to March 31, 2012 who had a determination of serum albumin level and total lymphocyte count on hospital admission were studied retrospectively. Admission serum albumin levels and total lymphocyte counts were used to classify the nutritional status of all patients in the study. Patients with a serum albumin less than 3.5 grams/dL and/or a TLC less than 1,500 cells per mm3 were classified as having protein energy malnutrition. The primary outcome investigated in this study was hospital readmission for any reason within 30 days of discharge.
Results. The study population included 1,683 hospital discharges with an average age of 79 years. The majority of the patients were female (55.9%) and had a DRG weight of 1.22 (0.68). 219 patients (13%) were readmitted within 30 days of hospital discharge. Protein energy malnutrition was common in this population. Low albumin was found in 973 (58%) patients and a low TLC was found in 1,152 (68%) patients. Low albumin and low TLC was found in 709 (42%) of patients. Kaplan–Meier analysis shows any laboratory evidence of PEM is a significant (p < 0.001) predictor of hospital readmission. Low serum albumin (p < 0.001) and TLC (p = 0.018) show similar trends. Cox proportional-hazards regression analysis showed low serum albumin (Hazard Ratio 3.27, 95% CI [2.30–4.63]) and higher DRG weight (Hazard Ratio 1.19, 95% CI [1.03–1.38]) to be significant independent predictors of hospital readmission within 30 days.
Discussion. This study investigated the relationship of PEM to the rate of hospital readmission within 30 days of discharge in patients 65 years of age or older. These results indicate that laboratory markers of PEM can identify patients at risk of hospital readmission within 30 days of discharge. This risk determination is simple and identifies a potentially modifiable risk factor for readmission: protein energy malnutrition.
Keywords: Malnutrition, Hospital readmission, Value based purchasing, Quality improvement
Introduction
Hospital readmission within 30 days of discharge is a target for health care cost savings in the Medicare Value Based Purchasing (VBP) program through reductions in payments to hospitals with higher than expected readmission rates (Centers for Medicare and Medicaid Services, 2015). Because of the VBP initiative, health care organizations are investing considerable resources into efforts to reduce hospital readmission. Identifying patients at risk of hospital readmission can be accomplished with a variety of risk assessment tools that range from multidisciplinary patient interviews to simple screening tools using a handful of variables (Kansagara et al., 2011; Silverstein et al., 2008; Smith et al., 2000). These tools use risk factors such as age, ethnicity, socioeconomic status, severity of illness, previous hospitalizations and other factors to predict who is likely to be readmitted. Unfortunately, many risk factors for hospital readmission are not modifiable. Protein energy malnutrition (PEM) is a known and potentially modifiable risk factor for hospital readmission (Lim et al., 2012; Fontes, Generoso & Toulson Davisson Correia, 2013; Sullivan, 1992).
The prevalence of PEM in general medical inpatients is 20–45% depending on the method used to assess PEM (Bistrian et al., 1976; Willard, Gilsdorf & Price, 1980; Persson et al., 2002; Barker, Gout & Crowe, 2011). Similar rates of PEM can be found in surgical and intensive care patients (O’Daly et al., 2010; Fontes, Generoso & Toulson Davisson Correia, 2014; Drevet et al., 2014). The subset of patients with PEM have a greater likelihood of inpatient mortality (Bonilla-Palomas et al., 2014; Persson et al., 2002; Barker, Gout & Crowe, 2011; O’Daly et al., 2010; Aziz et al., 2011; Correia & Waitzberg, 2003; Lim et al., 2012), longer length of hospital stay (Barker, Gout & Crowe, 2011; Jeejeebhoy et al., 2015; Aziz et al., 2011; Correia & Waitzberg, 2003; Lim et al., 2012), hospital readmission (Fontes, Generoso & Toulson Davisson Correia, 2014; Jeejeebhoy et al., 2015; Lim et al., 2012; Fontes, Generoso & Toulson Davisson Correia, 2013; Sullivan, 1992; Aziz et al., 2011; Friedmann et al., 1997), and inpatient costs (Correia & Waitzberg, 2003; Lim et al., 2012). Several studies have shown that inpatient nutritional interventions can improve outcomes such as mortality (Barchel et al., 2013), length of stay (Holyday et al., 2012), and hospital readmission (Holyday et al., 2012).
Unfortunately, identifying patients with PEM is complex and there is no clear consensus method of identifying patients with PEM (Kyle et al., 2006; Schneider & Hebuterne, 2000). Pablo and colleagues conducted an analysis of four commonly used nutritional assessment tools and identified the Instant Nutritional Assessment (INA) as the most sensitive and specific tool for identifying people with malnutrition at the time of hospital admission (Pablo, Izaga & Alday, 2003). The INA has a sensitivity of 100% and a specificity of 92% in this study, and relies on only two commonly obtained laboratory tests: the serum albumin level and the total lymphocyte count (Seltzer et al., 1981).
The simplicity and objectivity of the INA as a nutrition screening tool is compelling. These laboratory tests are inexpensive and are likely to be performed on the majority of patients ill enough to be admitted to a hospital. Several studies have shown good accuracy of the INA in predicting outcomes for femur fracture (Symeonidis & Clark, 2006; O’Daly et al., 2010). We hypothesize that the INA will also effectively identify medical patients at risk of hospital readmission within 30 days of discharge.
Materials and Methods
All medical patients 65 years of age or older discharged from Memorial Medical Center from January 1, 2012 to March 31, 2012 who had a determination of serum albumin level and total lymphocyte count on hospital admission were studied retrospectively. Memorial Medical Center is a 507 bed university-affiliated tertiary care center located in Springfield, Illinois, USA. Data on gender, age, serum albumin, DRG weight, total lymphocyte count (TLC), and hospital readmission within 30 days was extracted from the hospital electronic medical record system in a de-identified manner.
Admission serum albumin levels and total lymphocyte counts were used to classify the nutritional status of all patients in the study. Patients with a serum albumin less than 3.5 grams/dL and/or a TLC less than 1,500 cells per mm3 were classified as having PEM. Serum albumin and TLC were examined individually and together as predictors of outcome.
Diagnosis Related Group (DRG) weight was used as a marker of severity of illness. DRG weights are defined by the Centers for Medicare and Medicaid Services on an annual basis and are related to the cost and complexity of inpatient medical care for a specific DRG.
The primary outcome investigated in this study was hospital readmission for any reason within 30 days of discharge.
Institutional review board review for this study was obtained from the Springfield Committee for Research Involving Human Subjects. This study was determined to not meet criteria for research involving human subjects according to 45 CFR 46.101 and 45 CFR 46.102.
Statistical analysis
Serum albumin and TLC were investigated as predictors of hospital readmission within 30 days. Qualitative variables were compared using Pearson chi2 or Fisher’s exact test and reported as frequency (%). Quantitative variables were compared using the non-parametric Mann–Whitney U or Kruskal–Wallis tests and reported as mean ± standard deviation. Rates of survival were evaluated by the Kaplan–Meier method and compared using the log-rank test. Demographic and clinical variables were included as explanatory variables in a Cox proportional-hazards regression analysis in the following manner:
-
1.
Age, gender, DRG weight
-
2.
Age, gender, DRG weight, low albumin
-
3.
Age, gender, DRG weight, low TLC
-
4.
Age, gender, DRG weight, low albumin, low TLC
Statistical analyses were performed using SPSS version 22 (SPSS Inc., Chicago, IL, USA). Two sided P-values <0.05 were considered significant.
Results
The study population included 1,683 hospital discharges with an average age of 79 years. The majority of the patients in this sample were female (55.9%) and had a DRG weight of 1.22 (0.68). In this sample, 219 patients (13%) were readmitted to the same hospital within 30 days of hospital discharge.
Protein energy malnutrition was common in this population. Low albumin was found in 973 (58%) patients and a low TLC was found in 1,152 (68%) patients. Low albumin and low TLC was found in 709 (42%) of patients. Patients with PEM were older, had a higher DRG weight, and were more likely to be readmitted to the hospital within 30 days than patients without evidence of PEM (Table 1).
Table 1. Patient characteristics.
| No PEM N = 267 | PEM N = 1,416 | ||
|---|---|---|---|
| Age in years (SD) | 77 (8.03) | 79 (8.42) | P < 0.001 |
| Female gender (%) | 161 (60%) | 780 (55%) | P = 0.115 |
| DRG weight (SD) | 1.00 (0.39) | 1.26 (0.72) | P < 0.001 |
| Serum albumin g/dL (SD) | 3.82 (0.23) | 3.12 (0.61) | P < 0.001 |
| Total lymphocyte count 1,000 cells/mm3 (SD) | 3.50 (14.50) | 1.12 (1.01) | P < 0.001 |
| Readmitted within 30 days (%) | 13 (4.9%) | 206 (14.5%) | P < 0.001 |
Kaplan–Meier analysis shows any laboratory evidence of PEM is a significant (p < 0.001) predictor of hospital readmission (Fig. 1 and Table 2). Low serum albumin (Fig. 2 and Table 3, p < 0.001) and TLC (Fig. 3 and Table 4, p = 0.018) show similar trends.
Figure 1. Kaplan-Meier plot comparing 30 day readmission rates between patients with and without PEM.
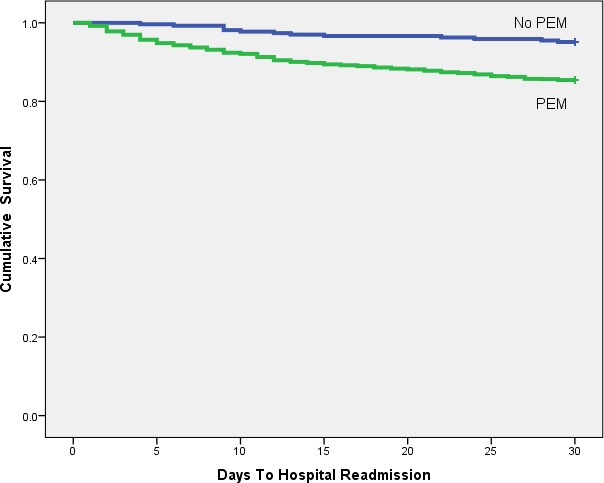
Table 2. Comparison of 30 day readmission-free survival between patients with normal and low albumin.
| Group | Discharged | 10 days | 20 days | 30 days |
|---|---|---|---|---|
| Normal albumin | 709 | 700 | 682 | 669 |
| Low albumin | 972 | 871 | 824 | 793 |
Figure 2. Kaplan-Meier plot comparing 30 day readmission rates between patients with low and normal albumin levels.
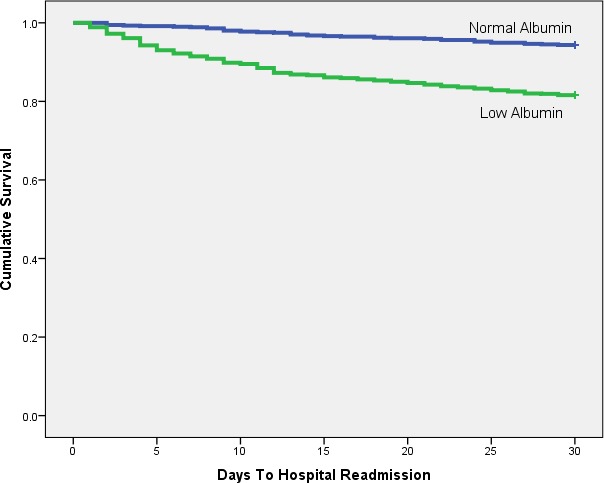
Table 3. Comparison of 30 day readmission-free survival between patients with and without PEM.
| Group | Discharged | 10 days | 20 days | 30 days |
|---|---|---|---|---|
| No PEM | 266 | 261 | 258 | 253 |
| PEM | 1,415 | 1,304 | 1,248 | 1,209 |
Figure 3. Kaplan-Meier plot comparing 30 day readmission rates between patients with low and normal TLC.
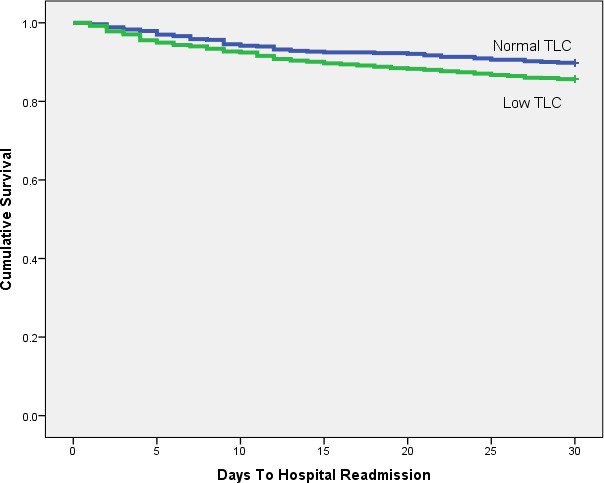
Table 4. Comparison of 30 day readmission-free survival between patients with normal and low TLC.
| Group | Discharged | 10 days | 20 days | 30 days |
|---|---|---|---|---|
| Normal TLC | 530 | 500 | 489 | 476 |
| Low TLC | 1,151 | 1,065 | 1,017 | 986 |
Multiple Cox proportional-hazards regression models were constructed to investigate the relationship of low albumin and low TLC to hospital readmission (Table 5). The regression model had C-statistics ranging from 0.562 to 0.653. The model that included age, gender, DRG weight, low albumin, and low TLC had the highest c-statistic at 0.653. Further analysis of this Cox proportional-hazards regression model showed low serum albumin (Hazard Ratio 3.27, 95% CI [2.30–4.63]) and higher DRG weight (Hazard Ratio 1.19, 95% CI [1.03–1.38]) to be significant independent predictors of hospital readmission within 30 days (Table 6).
Table 5. Cox proportional-hazard regression model characteristics for hospital readmission.
| Model components | −2 log likelihood | C-statistic |
|---|---|---|
| Age, gender, DRG weight | 3,209.726 | 0.562 |
| Age, gender, DRG weight, low albumin | 3,153.231 | 0.646 |
| Age, gender, DRG weight, low TLC | 3,204.440 | 0.570 |
| Age, gender, DRG weight, low albumin, low TLC | 3,150.560 | 0.653 |
Table 6. Cox proportional-hazards regression analysis of risk factors for hospital readmission.
| Variable | Regression coefficient | Standard error | Wald | P value | Hazard ratio (95% CI) |
|---|---|---|---|---|---|
| Age | −0.009 | 0.008 | 1.17 | 0.280 | 0.99 (0.98–1.01) |
| Gender | −0.026 | 0.137 | 0.04 | 0.849 | 0.97 (0.75–1.27) |
| DRG weight | 0.177 | 0.073 | 5.85 | 0.016 | 1.19 (1.03–1.38) |
| Low albumin | 1.184 | 0.178 | 44.16 | <0.001 | 3.27 (2.30–4.63) |
| Low TLC | 0.254 | 0.159 | 2.57 | 0.109 | 1.29 (0.95–1.76) |
Discussion
This study investigated the relationship of PEM to the rate of hospital readmission within 30 days of discharge in patients 65 years of age or older. These results indicate that laboratory markers of PEM can identify patients at risk of hospital readmission within 30 days of discharge. This risk determination is simple and identifies a potentially modifiable risk factor for readmission: protein energy malnutrition.
The results of this study show that PEM identified via the INA, is an independent risk factor for hospital readmission within 30 days even when controlling for age, gender and severity of illness. The INA is moderately good at predicting hospital readmission (c-statistic 0.653) which is comparable to other published methods for assessing readmission risk in real time (c-statistics range from 0.53 to 0.61, Kansagara et al., 2011). Malnutrition may not be the only cause of low serum albumin in this patient population because many illnesses can alter serum albumin values (Bachrach-Lindstrom et al., 2001; Fleck, 1988). Low serum albumin level alone is predictive of longer hospital stays (Herrmann et al., 1992; Numeroso, Barilli & Delsignore, 2008; Jellinge et al., 2014), readmission (Herrmann et al., 1992) and mortality (Herrmann et al., 1992; Lyons et al., 2010; Barchel et al., 2013; Jellinge et al., 2014; Cabrerizo et al., 2014) in medical inpatients.
More complex measures of nutritional status such as the Subjective Global Assessment (SGA) or Mini-nutritional Assessment (MNA) incorporate patient history, physical exam findings, and assessments of functional status (Dempsey & Mullen, 1987). These more complex measures of PEM are used in many studies of the clinical impact of nutritional interventions. However, the cost and time required to administer the SGA and MNA limits their widespread use. The INA, which we used in this study, was shown to be superior to the SGA in a small comparative study investigating the prevalence of PEM in hospitalized adults (Pablo, Izaga & Alday, 2003) and is suitable for adaptation as an automated clinical decision support tools within an electronic health record system to identify patients at increased risk of hospital readmission.
The generalizability of this investigation is limited because of the retrospective single center nature of this study. Hospital readmission data was only available from the study hospital, which could miss patients who were admitted at another hospital within 30 days of discharge. This would lead to a falsely low rate of hospital readmission. Unaccounted for local care delivery variables may have a significant impact on hospital readmissions within 30 days.
Conclusions
Protein energy malnutrition in medical inpatients is a significant predictor of hospital readmission within 30 days of discharge. Further investigation focusing on comorbid conditions is required to better understand the utility of laboratory tests of PEM for predicting hospital outcomes.
Supplemental Information
Funding Statement
The author received no funding for this work.
Additional Information and Declarations
Competing Interests
The author declares there are no competing interests.
Author Contributions
Robert Robinson conceived and designed the experiments, performed the experiments, analyzed the data, contributed reagents/materials/analysis tools, wrote the paper, prepared figures and/or tables, reviewed drafts of the paper.
Human Ethics
The following information was supplied relating to ethical approvals (i.e., approving body and any reference numbers):
Institutional review board approval for this study was obtained from the Springfield Committee for Research Involving Human Subjects. This study was classified as an exempt study because no individually identifiable information was collected.
References
- Aziz et al. (2011).Aziz EF, Javed F, Pratap B, Musat D, Nader A, Pulimi S, Alivar CL, Herzog E, Kukin ML. Malnutrition as assessed by nutritional risk index is associated with worse outcome in patients admitted with acute decompensated heart failure: an ACAP-HF data analysis. Heart International. 2011;6(1):e1181. doi: 10.4081/hi.2011.e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bachrach-Lindstrom et al. (2001).Bachrach-Lindstrom M, Unosson M, Ek AC, Arnqvist HJ. Assessment of nutritional status using biochemical and anthropometric variables in a nutritional intervention study of women with hip fracture. Clinical Nutrition. 2001;20:217–223. doi: 10.1054/clnu.2000.0383. [DOI] [PubMed] [Google Scholar]
- Barchel et al. (2013).Barchel D, Almoznino-Sarafian D, Shteinshnaider M, Tzur I, Cohen N, Gorelik O. Clinical characteristics and prognostic significance of serum albumin changes in an internal medicine ward. European Journal of Internal Medicine. 2013;24(8):772–778. doi: 10.1016/j.ejim.2013.08.004. [DOI] [PubMed] [Google Scholar]
- Barker, Gout & Crowe (2011).Barker LA, Gout BS, Crowe TC. Hospital malnutrition: prevalence, identification and impact on patients and the healthcare system. International Journal of Environmental Research and Public Health. 2011;8(2):514–527. doi: 10.3390/ijerph8020514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bistrian et al. (1976).Bistrian BR, Blackburn GL, Vitale J, Cochran D, Naylor J. Prevalence of malnutrition in general medical patients. Journal of the American Medical Association. 1976;235(15):1567–1570. doi: 10.1001/jama.1976.03260410023017. [DOI] [PubMed] [Google Scholar]
- Bonilla-Palomas et al. (2014).Bonilla-Palomas JL, Gámez-López AL, Moreno-Conde M, López-Ibáñez MC, Anguita-Sánchez M, Gallego de la Sacristana A, García-Catalán F, Villar-Ráez A. Hypoalbuminemia in acute heart failure patients: causes and its impact on hospital and long-term mortality. Journal of Cardiac Failure. 2014;20(5):350–358. doi: 10.1016/j.cardfail.2014.01.016. [DOI] [PubMed] [Google Scholar]
- Cabrerizo et al. (2014).Cabrerizo S, Cuadras D, Gomez-Busto F, Artaza-Artabe I, Marín-Ciancas F, Malafarina V. Serum albumin and health in older people: review and meta analysis. Maturitas. 2015;81(1):17–27. doi: 10.1016/j.maturitas.2015.02.009. [DOI] [PubMed] [Google Scholar]
- Centers for Medicare and Medicaid Services (2015).Centers for Medicare and Medicaid Services Hospital value based purchasing. 2015. Available at https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/hospital-value-based-purchasing/index.html (accessed 15 June 2015)
- Correia & Waitzberg (2003).Correia MI, Waitzberg DL. The impact of malnutrition on morbidity, mortality, length of hospital stay and costs evaluated through a multivariate model analysis. Clinical Nutrition. 2003;22(3):235–239. doi: 10.1016/S0261-5614(02)00215-7. [DOI] [PubMed] [Google Scholar]
- Dempsey & Mullen (1987).Dempsey DT, Mullen JL. Prognostic value of nutritional indices. Journal of Parenteral and Enteral Nutrition. 1987;11:109S–114S. doi: 10.1177/014860718701100517. [DOI] [PubMed] [Google Scholar]
- Drevet et al. (2014).Drevet S, Bioteau C, Mazière S, Couturier P, Merloz P, Tonetti J, Gavazzi G. Prevalence of protein-energy malnutrition in hospital patients over 75 years of age admitted for hip fracture. Orthopaedics and Traumatology: surgery and Research. 2014;100(6):669–674. doi: 10.1016/j.otsr.2014.05.003. [DOI] [PubMed] [Google Scholar]
- Fleck (1988).Fleck A. Plasma proteins as nutritional indicators in the perioperative period. British Journal of Clinical Practice. 1988;63:20–24. [PubMed] [Google Scholar]
- Fontes, Generoso & Toulson Davisson Correia (2013).Fontes D, Generoso SD, Toulson Davisson Correia MI Subjective global assessment: a reliable nutritional assessment tool to predict outcomes in critically ill patients. Clinical Nutrition. 2013 doi: 10.1016/j.clnu.2013.05.004. Epub ahead of print May 13 2013. [DOI] [PubMed] [Google Scholar]
- Fontes, Generoso & Toulson Davisson Correia (2014).Fontes D, Generoso Sde V, Toulson Davisson Correia MI Subjective global assessment: a reliable nutritional assessment tool to predict outcomes in critically ill patients. Clinical Nutrition. 2014;33(2):291–295. doi: 10.1016/j.clnu.2013.05.004. [DOI] [PubMed] [Google Scholar]
- Friedmann et al. (1997).Friedmann JM, Jensen GL, Smiciklas-Wright H, McCamish MA. Predicting early nonelective hospital readmission in nutritionally compromised older adults. American Journal of Clinical Nutrition. 1997;65(6):1714–1720. doi: 10.1093/ajcn/65.6.1714. [DOI] [PubMed] [Google Scholar]
- Herrmann et al. (1992).Herrmann FR, Safran C, Levkoff SE, Minaker KL. Serum albumin level on admission as a predictor of death, length of stay, and readmission. Archives of Internal Medicine. 1992;152(1):125–130. doi: 10.1001/archinte.1992.00400130135017. [DOI] [PubMed] [Google Scholar]
- Holyday et al. (2012).Holyday M, Daniells S, Bare M, Caplan GA, Petocz P, Bolin T. Malnutrition screening and early nutrition intervention in hospitalised patients in acute aged care: a randomised controlled trial. The Journal of Nutrition, Health and Aging. 2012;16(6):562–568. doi: 10.1007/s12603-012-0022-3. [DOI] [PubMed] [Google Scholar]
- Jeejeebhoy et al. (2015).Jeejeebhoy KN, Keller H, Gramlich L, Allard JP, Laporte M, Duerksen DR, Payette H, Bernier P, Vesnaver E, Davidson B, Teterina A, Lou W. Nutritional assessment: comparison of clinical assessment and objective variables for the prediction of length of hospital stay and readmission. American Journal of Clinical Nutrition. 2015;101(5):956–965. doi: 10.3945/ajcn.114.098665. [DOI] [PubMed] [Google Scholar]
- Jellinge et al. (2014).Jellinge ME, Henriksen DP, Hallas P, Brabrand M. Hypoalbuminemia is a strong predictor of 30-day all-cause mortality in acutely admitted medical patients: a prospective, observational, cohort study. PLoS ONE. 2014;9(8):e1181. doi: 10.1371/journal.pone.0105983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kansagara et al. (2011).Kansagara D, Englander H, Salanitro A, Kagen D, Theobald C, Freeman M, Kripalani S. Risk prediction models for hospital readmission: a systematic review. Journal of the American Medical Association. 2011;306(15):1688–1698. doi: 10.1001/jama.2011.1515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kyle et al. (2006).Kyle UG, Kossovsky MP, Karsegard VL, Pichard C. Comparison of tools for nutritional assessment and screening at hospital admission: a population study. Clinical Nutrition. 2006;25(3):409–417. doi: 10.1016/j.clnu.2005.11.001. [DOI] [PubMed] [Google Scholar]
- Lim et al. (2012).Lim SL, Ong KC, Chan YH, Loke WC, Ferguson M, Daniels L. Malnutrition and its impact on cost of hospitalization, length of stay, readmission and 3-year mortality. Clinical Nutrition. 2012;31(3):345–350. doi: 10.1016/j.clnu.2011.11.001. [DOI] [PubMed] [Google Scholar]
- Lyons et al. (2010).Lyons O, Whelan B, Bennett K, O’Riordan D, Silke B. Serum albumin as an outcome predictor in hospital emergency medical admissions. European Journal of Internal Medicine. 2010;21(1):17–20. doi: 10.1016/j.ejim.2009.10.010. [DOI] [PubMed] [Google Scholar]
- Numeroso, Barilli & Delsignore (2008).Numeroso F, Barilli AL, Delsignore R. Prevalence and significance of hypoalbuminemia in an internal medicine department. European Journal of Internal Medicine. 2008;19(8):587–591. doi: 10.1016/j.ejim.2007.04.029. [DOI] [PubMed] [Google Scholar]
- O’Daly et al. (2010).O’Daly BJ, Walsh JC, Quinlan JF, Falk GA, Stapleton R, Quinlan WR, O’Rourke SK. Serum albumin and total lymphocyte count as predictors of outcome in hip fractures. Clinical Nutrition. 2010;29(1):89–93. doi: 10.1016/j.clnu.2009.07.007. [DOI] [PubMed] [Google Scholar]
- Pablo, Izaga & Alday (2003).Pablo AM, Izaga MA, Alday LA. Assessment of nutritional status on hospital admission: nutritional scores. European Journal of Clinical Nutrition. 2003;57(7):824–831. doi: 10.1038/sj.ejcn.1601616. [DOI] [PubMed] [Google Scholar]
- Persson et al. (2002).Persson MD, Brismar KE, Katzarski KS, Nordenström J, Cederholm TE. Nutritional status using mini nutritional assessment and subjective global assessment predict mortality in geriatric patients. Journal of the American Geriatrics Society. 2002;50(12):1996–2002. doi: 10.1046/j.1532-5415.2002.50611.x. [DOI] [PubMed] [Google Scholar]
- Schneider & Hebuterne (2000).Schneider SM, Hebuterne X. Use of nutritional scores to predict clinical outcomes in chronic diseases. Nutrition Reviews. 2000;58(2 Pt 1):31–38. doi: 10.1111/j.1753-4887.2000.tb07809.x. [DOI] [PubMed] [Google Scholar]
- Seltzer et al. (1981).Seltzer MH, Fletcher HS, Slocum BA, Engler PE. Instant nutritional assessment in the intensive care unit. Journal of Parenteral and Enteral Nutrition. 1981;5(1):70–72. doi: 10.1177/014860718100500170. [DOI] [PubMed] [Google Scholar]
- Silverstein et al. (2008).Silverstein MD, Qin H, Mercer SQ, Fong J, Haydar Z. Risk factors for 30-day hospital readmission in patients ≥65 years of age. Proceedings (Baylor University. Medical Center) 2008;21(4):363–372. doi: 10.1080/08998280.2008.11928429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith et al. (2000).Smith DM, Giobbie-Hurder A, Weinberger M, Oddone EZ, Henderson WG, Asch DA, Ashton CM, Feussner JR, Ginier P, Huey JM, Hynes DM, Loo L, Mengel CE. Predicting non-elective hospital readmissions: a multi-site study. Department of veterans affairs cooperative study group on primary care and readmissions. Journal of Clinical Epidemiology. 2000;53(11):1113–1118. doi: 10.1016/S0895-4356(00)00236-5. [DOI] [PubMed] [Google Scholar]
- Sullivan (1992).Sullivan DH. Risk factors for early hospital readmission in a select population of geriatric rehabilitation patients: the significance of nutritional status. Journal of the American Geriatrics Society. 1992;40(8):792–798. doi: 10.1111/j.1532-5415.1992.tb01851.x. [DOI] [PubMed] [Google Scholar]
- Symeonidis & Clark (2006).Symeonidis PD, Clark D. Assessment of malnutrition in hip fracture patients: effects on surgical delay, hospital stay and mortality. ACTA Orthopaedica Belgica. 2006;72(4):420–427. [PubMed] [Google Scholar]
- Willard, Gilsdorf & Price (1980).Willard MD, Gilsdorf RB, Price RA. Protein-calorie malnutrition in a community hospital. Journal of the American Medical Association. 1980;243(17):1720–1722. doi: 10.1001/jama.1980.03300430022015. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


