Abstract
Background
Heart surgery has developed with increasing patient complexity.
Objective
To assess the use of resources and real costs stratified by risk factors of patients submitted to surgical cardiac procedures and to compare them with the values reimbursed by the Brazilian Unified Health System (SUS).
Method
All cardiac surgery procedures performed between January and July 2013 in a tertiary referral center were analyzed. Demographic and clinical data allowed the calculation of the value reimbursed by the Brazilian SUS. Patients were stratified as low, intermediate and high-risk categories according to the EuroSCORE. Clinical outcomes, use of resources and costs (real costs versus SUS) were compared between established risk groups.
Results
Postoperative mortality rates of low, intermediate and high-risk EuroSCORE risk strata showed a significant linear positive correlation (EuroSCORE: 3.8%, 10%, and 25%; p < 0.0001), as well as occurrence of any postoperative complication EuroSCORE: 13.7%, 20.7%, and 30.8%, respectively; p = 0.006). Accordingly, length-of-stay increased from 20.9 days to 24.8 and 29.2 days (p < 0.001). The real cost was parallel to increased resource use according to EuroSCORE risk strata (R$ 27.116,00 ± R$ 13.928,00 versus R$ 34.854,00 ± R$ 27.814,00 versus R$ 43.234,00 ± R$ 26.009,00, respectively; p < 0.001). SUS reimbursement also increased (R$ 14.306,00 ± R$ 4.571,00 versus R$ 16.217,00 ± R$ 7.298,00 versus R$ 19.548,00 ± R$935,00; p < 0.001). However, as the EuroSCORE increased, there was significant difference (p < 0.0001) between the real cost increasing slope and the SUS reimbursement elevation per EuroSCORE risk strata.
Conclusion
Higher EuroSCORE was related to higher postoperative mortality, complications, length of stay, and costs. Although SUS reimbursement increased according to risk, it was not proportional to real costs.
Keywords: Cardiac Surgical Procedures / economics, Hospital Costs, Unified Health System, Risk Groups, Preoperative Care, Hospital Mortality, Morbidity
Introduction
During the last four decades, cardiac surgery has developed with the increase in complex procedures in progressively critically-ill patients1. Evidence shows that this scenario proportionally increases with morbimortality and hospital costs2,3.
In Brazil, most of the highly complex procedures are performed with funding from the Unified Health System (SUS). This system is responsible for 80% of CABG surgeries performed in the country4. The reimbursement for hospitals that belong to SUS uses SUS own price list for the Hospitalization Authorization (AIH). The payment of this value is little yielding in its composition and may not reflect correct fund allocation that correspond to the Actual Cost (AC) of the procedure5. Thus, the AIH paid by SUS for the procedure may have no direct association with patient severity.
An unequal association between the AC of these procedures and SUS reimbursement may discourage hospital care provided to high-risk surgical patients, which are the cases that would benefit the most from these procedures6.
On the other hand, international guidelines advise about the use of risk scores to identify patients at higher risk of morbimortality7. In Brazil, the EuroSCORE is the most used model and the only one that has been validated in significant samples8.
The objective of this study was to evaluate the use of resources by risk group, comparing the AC of cardiovascular procedures with SUS reimbursement in a hospital.
Methods
Sample
A prospective observational study carried out at the Cardiovascular Surgery Division and SUS Billing Unit of Instituto do Coração do Hospital das Clínicas da Faculdade de Medicina da Universidade de São Paulo (InCor-HC/FMUSP) (Heart Institute of the Faculty of Medicine, University of São Paulo (InCor-HC / USP)).
Data from consecutive patients were obtained from the institution’s database (SI3). All demographic data that could identify patients were removed. Clinical data and use of resources were exported to an Excel spreadsheet for analysis. By cross-checking patients’ data with the registry of the participating units, it was verified that there were no errors and no patients loss due to lack of data.
Inclusion and exclusion criteria
The inclusion criteria were: adult patients consecutively operated between January and July 2013, in the elective, urgent or emergency mode, at the Cardiovascular Surgery Division of InCor-HC/FMUSP.
Patients not hospitalized by SUS were excluded from the study.
Data collection, definition and organization
Data were collected prospectively in the electronic medical file system of InCor-HC/FMUSP (SI3). After exporting data to a single worksheet in Excel and removal of demographic data that could identify patients, this worksheet was adapted to take into account all the variables described in the first EuroSCORE model (additive version)9. All definitions assigned to variables by EuroSCORE were accomplished, together with their values, according to their relevance to the death event.
Therefore, after calculating the value of the variables in each patient, the patients were classified according to the risk groups established by the model. In addition to the clinical and laboratory variables included in the EuroSCORE, the economic variables were considered. The total value of AC included fixed and variable costs per patient. The AC was calculated by analysis of variable costs accounted by the micro-costing methodology10 and by the full costing method for the fixed costs. The mean unit cost of each material item and medications was estimated from the purchases of these items during this period, being considered, in each category, the individual units costs. The mean unit cost of each diagnostic service, daily hospital stay costs or therapy was estimated by total inclusion of fixed costs (pro-rata of general consumption fixed costs – water, electricity and telephone, auxiliary services – maintenance contracts, cleaning services, air conditioning, etc., and administrative services) from the cost centers, divided by unit of produced outcome. Thus, we considered the quantitative variables ICU length of stay (days), hospitalization length of stay (days) and time of orotracheal intubation (hours). Similarly, it was considered the total value of SUS reimbursement, adding hospital service, professional service, ICU and compatible materials.
The primary outcomes were in-hospital mortality and morbidity (cerebrovascular accident, Renal Replacement Therapy - RRT, pneumonia, atrial fibrillation, mediastinitis/osteomyelitis and reoperation for bleeding). The definitions of the study variables outside the EuroSCORE were taken from the glossary of the American Heart Association11. All patients were followed until hospital discharge.
Statistical analysis
Continuous variables were expressed as mean ± standard deviation or median, and categorical variables as percentages. Logistic regression analysis for the hospital morbidity and mortality outcome was performed by using the value provided by EuroSCORE for each patient. Patients were subdivided by the EuroSCORE as low (1-4), intermediate (5-7), and high (≥ 8) risk.
The three categories were analyzed to highlight the differences related to the morbimortality, resource use, AC and SUS reimbursement. Variable distribution was tested for normality using the Kolmogorov-Smirnov test. Variables with normal distribution were compared between the risk categories using analysis of variance. Paired comparisons were corrected using the Bonferroni-Dunn test.
Student’s t test was used for parametric distributions, and the Mann-Whitney and Kruskal-Wallis tests were used for non-parametric distributions. Categorical variables were compared using Pearson’s chi-square test. The null hypothesis was rejected when p < 5% (p < 0.05). This study made a comparison, in the “real world”, between the mean costs of the risk categories, reducing the possibility of bias in patient selection12. The analysis was performed using the Statistical Package for the Social Sciences (SPSS) software, version 20.0.0 (Chicago, IL).
Ethics and Consent Form
This study was approved by the Ethics Committee for Analysis of Research Projects (CAPPesq) HC/FMUSP, under number 1575, being exempt from the need to use the Free and Informed Consent form, due to the use of analysis of non-identified data only.
Results
Sample
The characteristics of patients in the different risk groups are shown in Table 1. The low-risk group consisted of 131 (34%) patients, the intermediate risk group, of 150 (39%) and the high-risk group of 104 (27 %) patients. There were significant differences in EuroSCORE means according to the risk group: 2.91 ± 1.03, 5.89 ± 0.84 and 10.32 ± 2.6 in the lower, intermediate and high-risk categories, respectively. The mean age was 61 ± 12.29 years.
Table 1.
Patient characteristics
| Characteristics | Sample (n = 385) | Low Risk (n = 131) | Intermediate Risk (n = 150) | High Risk (n = 104) | p |
|---|---|---|---|---|---|
| Age | 61 ± 12.3 | 56.1 ± 10.3 | 61.2 ± 12.5 | 65.3 ± 12.5 | < 0.001* |
| Female gender | 160 (41.6) | 48 (36.6) | 69 (46) | 43 (41.3) | 0.28 |
| EuroSCORE | 6.1 ± 3.3 | 2.9 ± 1 | 5.9 ± 0.8 | 10.3 ± 2.6 | < 0.001* |
| Creatinine > 2mg/dL | 39 (10.1) | 2 (1.5) | 11 (7.3) | 26 (25) | < 0.001‡ |
| Ejection fraction < 30% | 32 (8.3) | 7 (5.3) | 16 (10.7) | 9 (8.7) | 0.27 |
| Recent Infarction | 42 (10.9) | 7 (5.3) | 18 (12) | 17 (16.3) | 0.012† |
| Reoperation | 68 (17.7) | 5 (3.8) | 25 (16.7) | 38 (36.5) | < 0.001* |
| CABG | 188 (48.8) | 78 (59.5) | 78 (52) | 32 (30.8) | < 0.001‡ |
| HVS | 173 (44.9) | 50 (38.2) | 63 (42) | 60 (57.7) | 0.002‡ |
| CABG + HVS | 21 (5.5) | 3 (2.3) | 7 (4.7) | 11 (10.6) | 0.007‡ |
| Others (Not CABG + HVS) | 3 (0.8) | 0 | 1 (0.7) | 2 (1.9) | 0.28 |
| Urgency / Emergency | 17 (4.4) | 2 (1.5) | 6 (4) | 9 (8.7) | 0.014‡ |
| Events | 38 (9.9) | 0 | 4 (2.7) | 34 (32.7) | < 0.001‡ |
The item “events” includes at least one of the following situations prior to surgery: intra-aortic balloon, cardiogenic shock, ventricular tachycardia or fibrillation, orotracheal intubation, acute renal failure, use of inotropic drugs and cardiac massage.
Significant difference between all risk groups;
significant difference between the low/intermediate risk groups and the high-risk group;
significant difference between the low-risk group and the intermediate/high risk group. CABG: coronary-artery bypass grafting; HVS: heart valve surgery.
Clinical outcomes and resource use
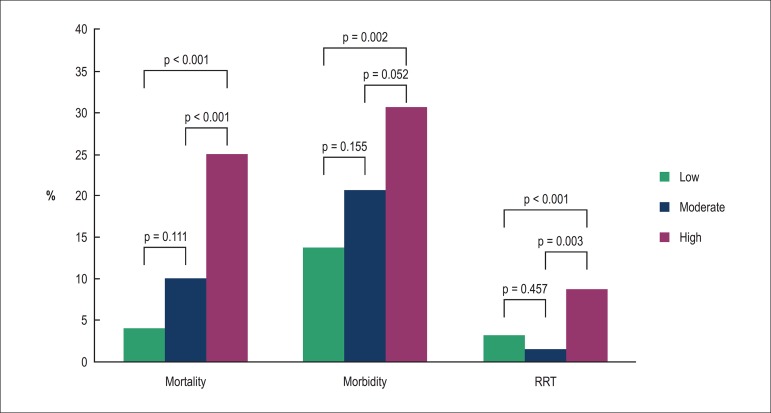
The clinical outcomes and resource use are shown in Table 2. The EuroSCORE was associated with death (p < 0.0001) and showed good calibration (p = 0.9744) in the Hosmer-Lemeshow test. Nevertheless, this model was associated with morbimortality (p < 0.0001) and also showed good calibration (p = 0.2221) in the Hosmer-Lemeshow test. Mortality, morbidity and morbimortality of 11.26, 21.41 and 27.15% were observed, respectively. There was 3.82% of mortality in low risk, 10% in intermediate risk and 25% in high risk (Figure 1). The low-risk group had the lowest percentage of deaths, which increased with the risk increase (p < 0.0001). There was 13.74% of morbidity in low risk, 20.67% in intermediate risk and 30.77% in the high risk. The low-risk group had a lower percentage of complications, which increased with the risk increase (p = 0.0063). There was 3.1% of RST in the low-risk, 1.3% in intermediate-risk and 8.7% in the high-risk group. The low-risk and intermediate-risk groups had the lowest percentage of RST, and the high-risk group had the highest percentage (p = 0.003). While one can observe that, regarding the length of stay, the high-risk group showed no significant difference compared to the intermediate risk, the low-risk group had a significantly lower value than the groups at high and intermediate risk. In the analysis of ICU length of stay, we observed that the low-risk group had significantly lower value than the groups with intermediate and high risk, and the group with intermediate risk had a significantly lower value than the high-risk group.
Table 2.
Clinical outcomes and resource utilization
| Variable | Sample (n = 385) | Low risk (n = 131) | Intermediate risk (n = 150) | High risk (n = 104) | p |
|---|---|---|---|---|---|
| Mortality | 56 (14.5) | 5 (3.8) | 15 (10) | 26 (25) | < 0.001* |
| Morbidity | 81 (21) | 18 (13.7) | 31 (20.7) | 32 (30.8) | 0.004* |
| CVA | 1 (0.3) | 1 (0.8) | 0 | 0 | 0.61 |
| Atrial fibrillation | 30 (7.8) | 6 (4.6) | 15 (10) | 9 (8.7) | 0.22 |
| RRT | 15 (3.9) | 4 (3.1) | 2 (1.3) | 9 (8.7) | 0.003* |
| Pneumonia | 12 (3.1) | 4 (3.1) | 3 (2) | 5 (4.8) | 0.46 |
| Reoperation x Bleeding | 17 (4.4) | 5(3.8) | 4 (2.7) | 8 (7.7) | 0.15 |
| OTI>24h | 22 (5.7) | 3 (2.3) | 9 (6) | 10 (9.6) | 0.055 |
| Time of ICU | 8.3 ± 10.1 days | 5.6 ± 5.9 days | 8.1 ± 10.4 days | 11.9 ± 12.6 days | < 0.001‡ |
| Hospital length of stay | 25 ± 17days | 21 ± 13.2days | 25 ± 13.25 days | 29 ± 16.3days | < 0.001† |
Significant difference between low / intermediate risk and high risk groups.
Significant difference between the low risk and intermediate / high risk groups.
Significant difference between all risk groups. CVA: cerebrovascular accident; RRT: renal replacement therapy; OTI: orotracheal intubation; ICU: intensive care unit.
Figure 1.
In-hospital outcomes of morbidity, mortality and renal replacement therapy (RRT) by risk groups, according to the EuroSCORE
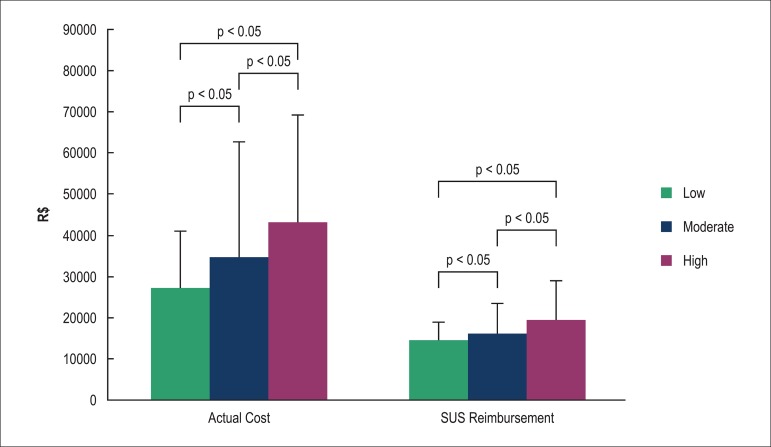
SUS reimbursement and actual cost
Risk groups differed in relation to the total value of the SUS reimbursement (low risk: R$ 14.306,00 ± R$ 4.571,00; intermediate risk: R$ 16.115,00 ± R$ 7.381,00, and high risk: R$ 19.548,00 ± R$ 9.355,00, p < 0.001), being higher in higher risk categories. Still, regarding the AC, the low risk group (R$ 27.116,00 ± R$ 13.928,00) showed a significantly lower value than the other groups, and the intermediate risk group had a significantly lower value than the high group risk (R$ 34,854.00 ± R$ 27,814.00 & R$ 43.234,00 ± R$ 26.009,00 ± R) (Figure 2).
Figure 2.
Total value of actual costs and the Unified Health System (SUS) reimbursement for risk groups, according to EuroSCORE.
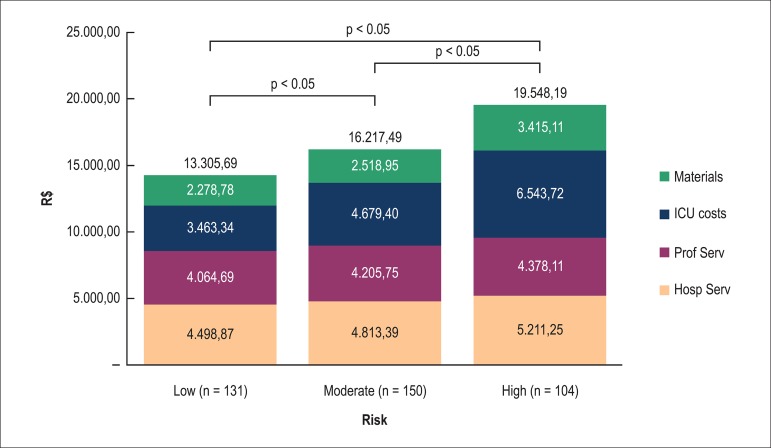
However, when we analyze the risk groups for specific values of SUS reimbursement, we found some discrepancies not demonstrated in the total sample (Figure 3). In reimbursement for hospital services, even if the high-risk group had significantly higher value than the low and intermediate-risk groups, the low-risk group showed no significant difference in relation to the intermediate risk group. Similarly, in relation to reimbursement for professional services, the low-risk group showed no significant difference in relation to the intermediate-risk group, although there was a lower significant difference in relation to the high-risk group.
Figure 3.
Detailed values of the of the Unified Health System (SUS) reimbursement for cardiovascular procedures by risk groups, according to EuroSCORE. Materials: reimbursement for cost of materials (excluding drugs); ICU costs: reimbursement for the intensive care unit services; Prof Serv: reimbursement for professional services; Hosp Serv: reimbursement for hospital services
In this item, the intermediate and high-risk groups were not significantly different. Similarly, on the reimbursement for the cost of materials, even if the high-risk group had significantly higher value than the low and intermediate-risk groups, the low risk group showed no significant difference in relation to the intermediate risk. Only in the reimbursement assessment for the ICU costs, the low-risk group had significantly lower value than the groups with intermediate and high risk, and the group with intermediate risk had a significantly lower value than the high-risk group.
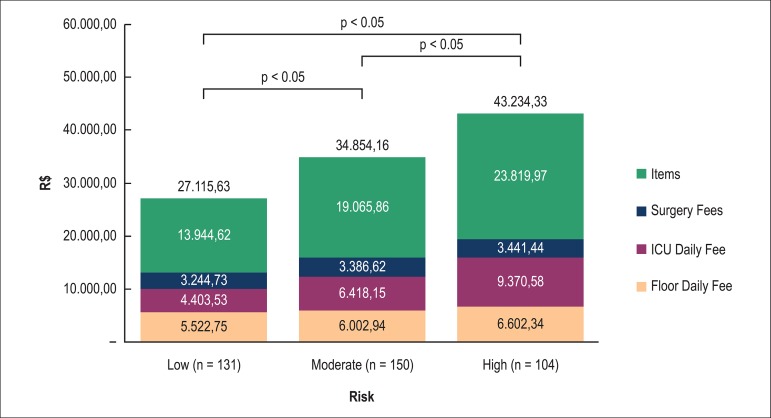
However, when we discriminately analyze the items established for the AC calculation (Figure 4), we can observe a significant difference as the risk increases by EuroSCORE.
Figure 4.
Detailed values of the actual costs for cardiovascular procedures by risk groups, according to the EuroSCORE. Items: includes the actual value of the materials and drugs; ICU: intensive care unit
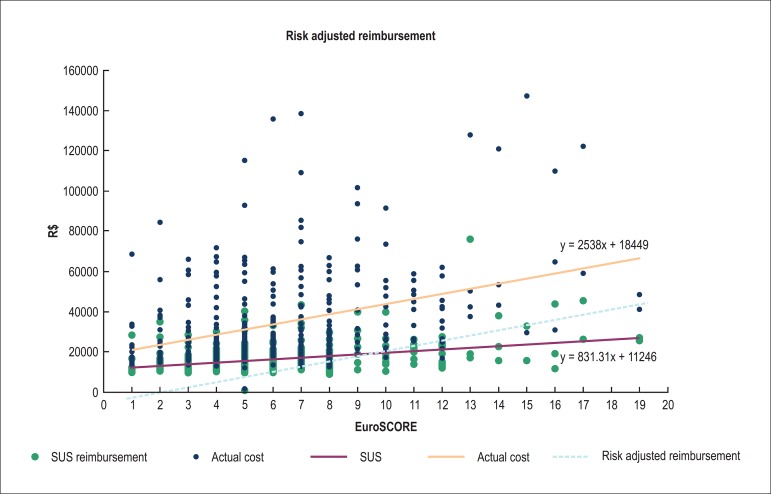
To confirm this, a logistic regression model was created for the SUS reimbursement value versus EuroSCORE (p < 0.0001):
11371 + 839.14*EuroSCORE
It was also a model for the AC value versus EuroSCORE (p < 0.0001):
18831 + 2577.69*EuroSCORE
Thus, with the estimates obtained from EuroSCORE (Table 3), the greater the patient risk, the greater the difference between the AC and the SUS reimbursement value.
Table 3.
Estimates obtained from the regression models for reimbursement by the Unified Health System (SUS) and the actual cost (AC), according to the EuroSCORE value.
| EuroSCORE | SUS (R$) | AC (R$) | Difference (R$) |
|---|---|---|---|
| 0 | 11,371.00 | 18,831.00 | -7,460.00 |
| 2 | 13,049.28 | 23,986.38 | -10,937.10 |
| 4 | 14,727.56 | 29,141.76 | -14,414.20 |
| 6 | 16,405.84 | 34,297.14 | -17,891.30 |
| 8 | 18,084.12 | 39,452.52 | -21,368.40 |
| 10 | 19,762.40 | 44,607.90 | -24,845.50 |
| 12 | 21,440.68 | 49,763.28 | -28,322.60 |
| 14 | 23,118.96 | 54,918.66 | -31,799.70 |
| 16 | 24,797.24 | 60,074.04 | -35,276.80 |
| 18 | 26,475.52 | 65,229.42 | -38,753.90 |
(R$) Values in Brazilian reais.
Discussion
Being a reference only in simple procedures should not give credit to an institution that does not make any effort to treat critically-ill patients that need complex surgeries. With an aging population and increasing life expectancy13, a larger population of frail patients is referred for cardiovascular procedures and improved quality of life. Evidence shows that critical patients are those that benefit the most from cardiovascular procedures, even if they have higher cost and morbimortality risk14.
This would explain why surgeons and hospitals that accept to operate more severe patients can have higher costs and greater morbimortality15,16. The use of risk scores allows the correction of the results according to patient severity for a more stringent cost-effectiveness analysis17. In Brazil, the most widely used risk model in cardiovascular surgery for outcome adjustment is the EuroSCORE18-22. Our study confirmed the direct association of the EuroSCORE with increased mortality and morbimortality.
SUS performs the majority of cardiovascular surgeries in Brazil, treating primarily patients with more unfavorable socioeconomic conditions. At InCor-HC/FMUSP, the number of cardiovascular surgeries by SUS corresponds to approximately 80% of the total. It is important to mention that the government allocates to the public health in Brazil a total of US$ 157.00 per inhabitant/year (I/Y). This is in sharp contrast with public health spending in Germany (US$ 3.521,00 I/Y), Canada (US$ 2.823,00 I/Y), United States (US$ 2.725,00 I/Y), Portugal (US$ 1,850,00 I/Y), Chile (US$ 720,00 I/Y), Argentina (US$ 380,00 I/Y) and Costa Rica (US$ 378,00 I/Y)6. We know that the value of public spending in the US is an emblematic example of a system segmented for the poor (Medicaid), elderly (Medicare) and war veterans (about 66 million of inhabitants), while Brazil is the source of funding for approximately 160 million of inhabitants23.
A publication on patients undergoing aortic valve replacement in the United States showed a direct correlation between the risk increase of patients and increased morbimortality and costs14. In Brazil, a study published by Instituto Dante Pazzanese de Cardiologia5 (Dante Pazzanese Institute of Cardiology) showed that the cost of coronary artery bypass surgery (primary, isolated and elective) is lower than the reimbursement supplied by SUS, showing that the mean cost of surgery was R$ 6.990,00 and the amount paid was R$ 5.551.41. These values are different from those found in our analysis, upon which the variety of procedures performed, including emergency care, the progressive worsening of the patients over time, and the current adjustment of costs and SUS reimbursement may have influenced.
This cost discrepancy has made university and philanthropic hospitals, and even private hospitals with social security-funded care suspend medical care due to accumulated debt. All this can worsen considering the global trend of increased high-risk patients referred to undergo cardiovascular procedures.
In this study, it was shown that AC increases progressively when the preoperative risk of the patient increases. Although the SUS reimbursement also increases with the patient’s risk, it is disproportionate to the AC, and this increases as the patient’s risk increases. This scenario could influence the selection of patients operated in SUS-funded hospitals. Unquestionably, the ideal would be that SUS-funded hospitals be reimbursed by an amount equivalent to the AC. However, the minimum to be done is a reimbursement proportional to the AC. In the current context and for the same budget, that would be to pay less for low-risk surgeries and more for higher-risk surgeries, according to what we call risk adjusted reimbursement (Figure 5). Therefore, for each EuroSCORE unit increase, there will be a fairer amount to be reimbursed by SUS.
Figure 5.
Unified Health System (SUS) reimbursement increase, actual cost (AC) and risk adjusted reimbursement, according to the EuroSCORE value
Study limitations
There are several limitations in this study. First, no follow-up was performed for long-term analysis, although a recent study showed that, in a follow-up of five years after aortic valve replacement, there was a higher cost for high-risk patients24. Second, a multicenter analysis could have found differences related to specific patterns of SUS reimbursement between hospital categories. Third, the sample size may have influenced some analyses, especially among the categories of intermediate and high risk. Fourth, some risk factors, such as frailty, were excluded from the study. However, this could increase differences in the high-risk patient group25.
In short, high-risk patients referred for cardiovascular surgery, in addition to the fact that they have higher cost, also show higher risk of morbimortality. Analyses in larger samples are needed to justify the cost-effectiveness of the procedures, to support SUS sustainability and funding, and improve the quality of outcomes and safety for patients.
Conclusions
Although the SUS reimbursement increases with the increase in patient risk, it is disproportionate to the real cost. Future directions in SUS reimbursement should be adopted so that care of an increasing number of high-risk surgical patients is not discouraged.
Acknowledgments
To FAFESP, for the limitless support in carrying out the present study.
Footnotes
Sources of Funding
There were no external funding sources for this study.
Study Association
This study is not associated with any thesis or dissertation work.
References
- 1.Pettersson GB, Martino D, Blackstone EH, Nowicki ER, Houghtaling PL, Sabik JF, 3rd, et al. Advising complex patients who require complex heart operations. J Thorac Cardiovasc Surg. 2013;145(5):1159–1169.: doi: 10.1016/j.jtcvs.2012.11.035. [DOI] [PubMed] [Google Scholar]
- 2.Engoren M, Arslanian-Engoren C, Steckel D, Neihardt J, Fenn-Buderer N. Cost, outcome, and functional status in octogenarians and septuagenarians after cardiac surgery. Chest. 2002;122(4):1309–1315. doi: 10.1378/chest.122.4.1309. [DOI] [PubMed] [Google Scholar]
- 3.Scott BH, Seifert FC, Grimson R, Glass PS. Octogenarians undergoing coronary artery bypass graft surgery: resource utilization, postoperative mortality, and morbidity. J Cardiothorac Vasc Anesth. 2005;19(5):583–588. doi: 10.1053/j.jvca.2005.03.030. [DOI] [PubMed] [Google Scholar]
- 4.Piegas LS, Bittar OJ, Haddad N. Myocardial revascularization surgery (MRS): results from national health system (SUS) Arq Bras Cardiol. 2009;93(5):555–560. doi: 10.1590/s0066-782x2009001100018. [DOI] [PubMed] [Google Scholar]
- 5.Haddad N, Bittar E, Marchi AF, Kantorowitz CS, Ayoub AC, Fonseca ML, et al. Hospital costs of coronary artery bypass grafting on elective coronary patients. Arq Bras Cardiol. 2007;88(94):418–423. doi: 10.1590/s0066-782x2007000400009. [DOI] [PubMed] [Google Scholar]
- 6.Gomes WJ, Mendonça JT, Braile DM. Cardiovascular surgery outcomes opportunity to rediscuss medical and cardiological care in the Brazilian public health system. Rev Bras Cir Cardiovasc. 2007;22(4):III–IVI. doi: 10.1590/s0102-76382007000400002. [DOI] [PubMed] [Google Scholar]
- 7.Kolh P, Wijns W. Essential messages from the ESC/EACTS guidelines on myocardial revascularization. Eur J Cardiothorac Surg. 2012;41(5):983–985. doi: 10.1093/ejcts/ezs023. [DOI] [PubMed] [Google Scholar]
- 8.Mejía OA, Lisboa LA, Dallan LA, Pomerantzeff PM, Moreira LF, Jatene FB, et al. Validation of the 2000 Bernstein-Parsonnet and EuroSCORE at the Heart Institute - USP. Rev Bras Cir Cardiovasc. 2012;27(2):187–194. doi: 10.5935/1678-9741.20120033. [DOI] [PubMed] [Google Scholar]
- 9.Nashef SA, Roques F, Michel P, Gauducheau E, Lemeshow S, Salamon R. European system for cardiac operative risk evaluation (EuroSCORE) Eur J Cardiothorac Surg. 1999;16(1):9–13. doi: 10.1016/s1010-7940(99)00134-7. [DOI] [PubMed] [Google Scholar]
- 10.Smith MW, Barnett PG, Phibbs CS, Wagner TH. Microcost methods of determining VA healthcare costs. Menlo Park, CA: Health Economics Resource Center; 2010. [Google Scholar]
- 11.Weintraub WS, Karlsberg RP, Tcheng JE, Boris JR, Buxton AE, Dove JT, et al. American College of Cardiology Foundation. American Heart Association Task Force on Clinical Data Standards ACCF/AHA 2011 key data elements and definitions of a base cardiovascular vocabulary for electronic health records: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Clinical Data Standards. Circulation. 2011;124(1):103–123. doi: 10.1161/CIR.0b013e31821ccf71. [DOI] [PubMed] [Google Scholar]
- 12.Polsky D, Glick H. Costing and cost analysis in randomized controlled trials: caveat emptor. Pharmacoeconomics. 2009;27(3):179–188. doi: 10.2165/00019053-200927030-00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Global Population Estimates by Age, 1950-2050. [Access in 2014 Dec 24]. Available from: http://www.pewglobal.org/2014/01/30/global-population.
- 14.Osnabrugge RL, Speir AM, Head SJ, Fonner CE, Fonner E, Jr, Ailawadi G, et al. Costs for surgical aortic valve replacement according to preoperative risk categories. Ann Thorac Surg. 2013;96(2):500–506. doi: 10.1016/j.athoracsur.2013.04.038. [DOI] [PubMed] [Google Scholar]
- 15.Clark MA, Duhay FG, Thompson AK, Keyes MJ, Svensson LG, Bonow RO, et al. Clinical and economic outcomes after surgical aortic valve replacement in Medicare patients. Risk Manag Healthc Policy. 2012;5:117–126. doi: 10.2147/RMHP.S34587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bhamidipati CM, LaPar DJ, Fonner E, Jr, Kern JA, Kron IL, Ailawadi G. Outcomes and cost of cardiac surgery in octogenarians is related to type of operation: a multiinstitutional analysis. Ann Thorac Surg. 2011;91(2):499–505. doi: 10.1016/j.athoracsur.2010.10.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Smith CR, Leon MB, Mack MJ, Miller DC, Moses JW, Svensson LG, et al. PARTNER Trial Investigators Transcatheter versus surgical aortic-valve replacement in high-risk patients. N Engl J Med. 2011;364(23):2187–2198. doi: 10.1056/NEJMoa1103510. [DOI] [PubMed] [Google Scholar]
- 18.Moraes F, Duarte C, Cardoso E, Tenório E, Pereira V, Lampreia D, et al. Assessment of the Euroscore as a predictor for mortality in myocardial revascularization surgery at the Heart Institute of Pernambuco. Rev Bras Cir Cardiovasc. 2006;21(1):29–34. [Google Scholar]
- 19.Sá MP, Soares EF, Santos CA, Figueredo OJ, Lima RO, Escobar RR, et al. EuroSCORE and mortality in coronary artery bypass graft surgery at Pernambuco Cardiologic Emergency Medical Services. Rev Bras Cir Cardiovasc. 2010;25(4):474–482. doi: 10.1590/s0102-76382010000400010. [DOI] [PubMed] [Google Scholar]
- 20.Carvalho MRM, Silva NASe, Klein CH, Oliveira GMM. Aplicação do EuroSCORE na cirurgia de revascularização miocárdica em hospitais públicos do Rio de Janeiro. Rev Bras Cir Cardiovasc. 2010;25(2):209–217. doi: 10.1590/s0102-76382010000200013. [DOI] [PubMed] [Google Scholar]
- 21.Mejía OA, Lisboa LA, Puig LB, Dias RR, Dallan LA, Pomerantzeff PM, et al. The 2000 Bernstein-Parsonnet score and EuroSCORE are similar in predicting mortality at the Heart Institute, USP. Rev Bras Cir Cardiovasc. 2011;26(1):1–6. doi: 10.1590/s0102-76382011000100004. [DOI] [PubMed] [Google Scholar]
- 22.Lisboa LAF, Mejia OA, Moreira LF, Dallan LAO, Pomerantzeff PM, Dallan LR, et al. EuroSCORE II e a importância de um modelo local, InsCor e o futuro SP-SCORE. Rev Bras Cir Cardiovasc. 2014;29(1):1–8. doi: 10.5935/1678-9741.20140004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mendes EV. 25 anos do Sistema Único de Saúde: resultados e desafios. Estudos Avançados. 2013;27(78):27–34. [Google Scholar]
- 24.Clark MA, Duhay FG, Thompson AK, Keyes MJ, Svensson LG, Bonow RO, et al. Clinical and economic outcomes after surgical aortic valve replacement in medicare patients. Risk Manag Healthc Policy. 2012;5:117–126. doi: 10.2147/RMHP.S34587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kappetein AP, Head SJ, Genereux P, Piazza N, van Mieghem NM, Blackstone EH, et al. Valve Academic Research Consortium VARC)-2. Updated standardized endpoint definitions for transcatheter aortic valve implantation: the Valve Academic Research Consortium-2 consensus document (VARC-2) Eur J Cardiothorac Surg. 2012;42(5):S45–S60. doi: 10.1093/ejcts/ezs533. [DOI] [PubMed] [Google Scholar]