Abstract
National surveys are relevant for the study of sleep epidemiology since they can provide specific data about sleep in large dimension with important implications for the health system. Thus, the aim of this study was to investigate the prevalence of sleep complaints among the Brazilian population using a randomized cluster sample according to region and socioeconomic class. For this, a 3-stage sampling technique was used to randomly select Brazilian subjects of both genders older than 16 years. A total of 2017 subjects, from 132 different cities, were selected to estimate prevalence in the Brazilian population with a sampling error of ±2%. Questions about sleep complaints were administered face-to-face by Instituto Datafolha interviewers on April 10 and 16, 2012. Data were expanded using a weighted variable. The results showed that 76% of the study population suffers from at least 1 sleep complaint, indicating that approximately 108 million Brazilians may be affected by sleep disorders. On average, each subject had 1.9 sleep problems with the most common complaints being light and insufficient sleep, snoring, moving a lot during sleep, and insomnia, which usually occurred more than 3 times per week. Low income was associated with higher number of sleep complaints only in Northeast and Southeast regions. In conclusion, this study showed a high prevalence of sleep complaints in a sample of the Brazilian population, suggesting that sleep disorders may be markedly frequent in the Brazilian population with a possible correlation with the socioeconomic situation of the interviewed subjects.
Keywords: Epidemiology, Sleep, Sleep disorder, Socioeconomic factors, Population
1. Introduction
Worldwide populations, especially those living in industrialized countries, experience sleep curtailment, which is rapidly becoming a hallmark of modern society associated with significant social, financial, and human cost [23]. Chronic sleep restriction is often related to the changes due to modern life, such as work-related demands, social and domestic responsibilities, and current lifestyles [5]. In addition, sleep disorders are becoming more and more common, resulting in a clinically significant impact on public health [15]. Ten percent of the American population is reported to suffer from chronic sleep disorders with health and safety consequences [32]. Similarly, over 3 decades, an increase in sleep complaints such as snoring, insomnia, and bruxism has been observed in the population of São Paulo, the largest city in Brazil [35]. Snoring is the most prevalent complaint, with increase of 20% in the last 2 decades [35].
National and epidemiological studies provide scientific knowledge about sleep for the population as well as the development of public health policies. In 2008, a national survey with a sample of 2110 subjects from 150 different cities estimated the prevalence of sleep disorders in the Brazilian population, indicating that 63% reported at least 1 sleep related complaint [6]. Brazil in particular has experienced continuous changes in lifestyle and environment recently, as the Brazilian economy develops and the middle class increases within an underlying context of social inequality, limited access to specialized support services, scarce financial resources, and a lack of structural adaptations [9].
Thus, in order to clarify the health and social challenges represented by the last 4 years on the sleep quality of the Brazilian population, we investigated subjectively the prevalence of sleep complaints in a representative sample of Brazil. We expect with this survey to understand how sleep complaints are influenced by socioeconomic factors in order to target high-risk groups for future interventions.
2. Material and methods
2.1. Study design
This is an observational cross-sectional study. The sample design was based on data from the 2010 Brazilian census, considering the projected population for 2011 (142,448,650 inhabitants) (www.ibge.gov.brr), and following a 3-stage cluster sampling technique described elsewhere [16]. First, Federal Units were proportionally stratified by population and city sizes. Then, cities were randomly selected as well as the research points. After data collection through structured interviews, checking in person (in situ) and by phone covered at least 20% of each survey [6]. There was no incentive for the subjects to participate in the study. This study was approved by Ethical Committee of UNIFESP (Protocol number # 573181).
2.2. Participants
This study was part of a national survey which included other topics besides sleep. Study questions about sleep complaints were asked in face-to-face sessions by non-specialized interviewers from Instituto Datafolha for all selected subjects on April 10 and 16, 2012. On these days, the interviewers went to the participants׳ home selected in the study. Subjects older than 16 years old, representing both genders and all socioeconomic classes according to the Brazilian Economic Classification Criteria (CCEB) (http://www.abep.org/new/criterioBrasil.aspx), were selected to represent Brazilian population in the current study. A total of 2017 subjects from 132 different cities were selected to estimate Brazilian population characteristics with a sampling error of ±2%, considering a 95% confidence interval. For 0.5% or lower estimates, zero was assumed. Frequencies lower than 30 were not enough for statistical analysis.
2.3. Questionnaires
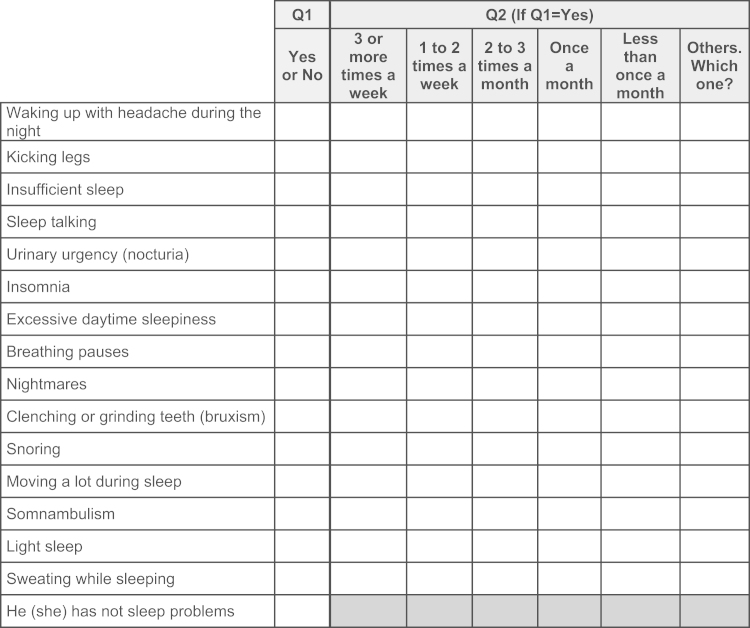
Screening questions of a non-validated questionnaire were asked about the presence of waking up with headache, kicking legs, insufficient sleep, sleep talking, nocturia, insomnia, excessive daytime sleepiness, breathing pauses, nightmares, bruxism, snoring, moving a lot during sleep, somnambulism, light sleep, sweating while sleeping, or other complaints during sleep. Answers were categorized in frequencies of occurrence: ≥3 times a week, 1–2 times a week, 2–3 times a month, once a month and less than once a month (Fig. 1). The questions were focused to the present, but no time frame was offered for the 15 sleep symptoms, representing the lifetime prevalence.
Fig. 1.
Questions about sleep complaints asked to all subjects: Q1. Do you have any of the following problems during sleep? Do you have other problems during sleep that are not presented on this card? Q2. How frequent is this problem?
2.4. Sleep complaint definitions
The definition used for presence of 1 or more sleep complaints was based on the answer of the volunteer in the first question (Q1, Fig. 1 – 15 sleep complaints asked), independent of frequency of occurrence. The presence of any sleep complaint was defined based on the occurrence of at least 1 positive answer for the 15 sleep complaints asked in the first question (Q1).
2.5. Statistical analysis
To guarantee the representativeness, the data were expanded using a weighted variable based on population profiles of gender, region and socioeconomic class considering the census data from 2010. The weight was pre-specified based on population profiles of the region (Center-West and North, Northeast, South and Southeast), including small and metropolitan cities, and socioeconomic class using Taylor׳s linearization method. From the 2017 participants, 564 participants did not know or refused to answer the question about their family monthly income, leading to missing data for this variable. To evaluate the statistical significance between proportions, weighted χ2 test was used. For analysis of total sleep complaints according to gender, age, years of schooling, family monthly income and socioeconomic class categories, a T-test or one-way analysis of variance (ANOVA), followed by Bonferroni׳s post hoc test when necessary, was used. To understand the interactions between region and income on sleep, two-way ANOVA was used for the total number of sleep complaints, followed by Bonferroni׳s post hoc test. Significance level was set at p≤0.05. All analyzes were performed using SPSS 20 (Chicago, IL, USA).
3. Results
A total of 2017 subjects were selected according to the Brazilian regions: 16% from the Center-West and North, 29% from Northeast, 41% from the Southeast and 14% from the South. The mean age was 39 years (SD 17). Only 1 person refused to answer the sleep questions and the response rate was 99.95%. Thirty-nine percent of the study population was located in metropolitan areas and 61% in smaller cities. The study population from the 4 regions was homogeneous for age, gender, occupational status, and years of schooling. However, the Northeast and Center-West and North regions were associated with lower family income (χ2=94.4, df=9, p<0.0001) and socioeconomic class (χ2=144.5, df=6, p<0.0001). The South and Southeast regions were associated with higher family income and socioeconomic class. Significant association was found between socioeconomic status and education level (χ2=528.4, df=4, p<0.0001). The sociodemographic characteristics of the sample are represented in Table 1.
Table 1.
Sociodemographic characteristics of population (N=2017). Percentages (95% CI) were expanded using a weighted variable.
| Variables | % (95% CI) | N |
|---|---|---|
| Gender | ||
| Male | 48 (47.4–49.3) | 974 |
| Female | 52 (50.7–52.6) | 1043 |
| Age (years) | ||
| 16–24 | 22 (21.4–23.2) | 447 |
| 25–34 | 24 (22.7–24.7) | 477 |
| 35–44 | 19 (18.4–20.4) | 389 |
| 45–59 | 21 (19.8–21.8) | 420 |
| 60 or more | 14 (13.2–14.8) | 284 |
| Years of schooling (years) | ||
| ≤8 | 41 (38.4–44.3) | 843 |
| 8–12 | 50 (47.5–51.9) | 991 |
| >12 | 9 (7.5–10.7) | 183 |
| Family monthly income | ||
| <R$1244.00 | 40 (35.8–43.6) | 637 |
| R$1245.00–6220.00 | 48 (45–50.9) | 756 |
| >R$6220.00 | 5 (4.1–6.9) | 86 |
| Refused | 7 (5.3–9.5) | 110 |
| Socioeconomic classes | ||
| Upper (A+B) | 30 (26.0–33.2) | 601 |
| Middle (C) | 52 (49–54.5) | 1015 |
| Lower (D+E) | 19 (16.4–21.5) | 401 |
| Occupational status | ||
| Not working | 31 (29.3–33.0) | 627 |
| Working | 69 (67.0–70.7) | 1390 |
CI: confidence interval.
On average, each subject complained of 1.9 sleep symptoms. Sleep complaints were more frequent in women than in men (Table 2). No significant differences were found in the total number of sleep complaints according to years of schooling, family monthly income, socioeconomic class and occupational status. However, a region effect was observed in the total number of sleep complaints (F3,1983=6.4, p<0.0001), showing that in the South region, subjects complained less than in Northeast (p<0.0001) and Southeast (p<0.05). The number of sleep complaints significantly increased with age (F4,1982=5.1, p<0.0001). No subject reported any sleep complaint other than those covered by the 15 items on the questionnaire.
Table 2.
Number of sleep complaints in the population (N=2017) according to gender, years of schooling, family monthly income, socioeconomic class, occupation and region.
|
Mean±SEM |
|
|---|---|
| Total (95% CI) | 1.9±0.1 (1.8-2.1) |
| Age (years) | |
| 16–24 | 1.7±0.1 |
| 25–34 | 1.8±0.1 |
| 35–44 | 2.0±0.1 |
| 45–59 | 2.1±0.1⁎ |
| 60 or more | 2.2±0.1⁎,# |
| Gender | |
| Male | 1.8±0.1 |
| Female | 2.1±0.1⁎ |
| Years of schooling | |
| ≤8 | 2.1±0.1 |
| 8–12 | 1.9±0.1 |
| >12 | 1.7±0.1 |
| Family monthly income | |
| <R$1244.00 | 1.9±0.1 |
| R$1245.00–6220.00 | 1.9±0.1 |
| >R$6220.00 | 1.9±0.2 |
| Refused | 1.8±0.2 |
| Socioeconomic class | |
| Upper (A+B) | 1.9±0.1 |
| Middle (C) | 1.9±0.1 |
| Lower (D+E) | 2.1±0.1 |
| Occupation | |
| Working | 2.0±0.1 |
| Not working | 1.9±0.1 |
| Region | |
| Center-west and North | 1.8±0.1 |
| Northeast | 2.1±0.1 |
| Southeast | 2.0±0.1 |
| South | 1.6±0.1#,+ |
CI: confidence interval; SEM: standard error of mean.
p<0.05 compared to 16–24 years of age or male gender;
p<0.05 compared to 25–34 years of age or Northeast region;
p<p<0.05 compared to the Southeast region.
As observed in Table 3, 76% (95% CI: 73–79%) of subjects had at least 1 sleep complaint. The most common sleep complaints were light sleep (27%), snoring (25%), insufficient sleep (23%), moving a lot during sleep (22%), and insomnia (21%). The less frequent complaints were somnambulism (1%), breathing pauses (3%), urinary urgency (5%), kicking legs (6%), and bruxism (7%). Most sleep problems were associated with insomnia, which in turn was significantly associated with light and insufficient sleep, snoring and nightmares. People who snored also complained about light and insufficient sleep, moving a lot during sleep, excessive daytime sleepiness and insomnia.
Table 3.
Sleep complaints in the Brazilian population sample (N=2017). Percentages (95% CI) were expanded using a weighted variable.
| Total | Male | Female | 16–24 (years) | 25–34 (years) | 35–44 (years) | 45–59 (years) | >60 (years) | |
|---|---|---|---|---|---|---|---|---|
| Any sleep complaint | 76 (72.9–78.6) | 76 (72.1–79.1) | 76 (72.4–79.2) | 73 (67.8–77.6) | 73 (67.8–77.0) | 80 (74.8–83.8)* | 79 (74.3–82.5) | 76 (71.3–81.4) |
| Waking up with headache | 9 (7.9–11.0) | 6 (4.2–7.3) | 13 (10.7–15.4)# | 7 (4.4–9.6) | 10 (7.7–13.5) | 10 (7.3–12.8) | 12 (8.3–15.5) | 9 (5.8–12.7) |
| Kicking legs | 6 (4.7–7.1) | 6 (4.5–7.9) | 6 (4.2–7.2) | 7 (4.8–9.9) | 6 (3.6–8.4) | 4 (2.4–6.1) | 5.9 (3.8–9.1) | 7 (4.1–10.5) |
| Insufficient sleep | 23 (21.1–25–8) | 22 (18.5–24.8) | 25 (22.2–28.4) | 22 (18.1–25.9) | 20 (16.2–24.2) | 27 (22.5–31.1) | 25 (20.7–29.6) | 25 (20.1–30.9) |
| Sleep talking | 10 (0.8–11.8) | 9.2 (7.5–11.3) | 11 (9.1–13.3) | 16 (12.7–19.5)* | 12 (9.5–15.8) | 7 (4.9–10.9) | 6 (4.3–9.5) | 7 (4.5–10.3) |
| Urinary incontinence | 5 (0.6–6.5) | 4 (2.9–5.7) | 6 (4.7–8.0) | 3 (1.4–4.8) | 3 (1.4–4.7) | 4 (2.4–6.5) | 6 (4.0–9.6) | 13 (9.7–18.0)* |
| Insomnia | 21 (19.2–23.4) | 18 (15.6–20.9) | 24 (21.7–26.8)# | 15 (11.5–18.4) | 18 (15.2–22.0) | 24 (19.0–28.8) | 24 (20.3–28.2) | 30 (24.0–35.3)* |
| Excessive daytime sleepiness | 12 (10.4–13.8) | 9 (7.1–11.5) | 14.8 (12.7–17.1)# | 16 (12.5–20.0)* | 10 (7.4–13.1) | 11 (7.9–14.0) | 10 (7.2–14.8) | 14 (10.4–17.9) |
| Breathing pauses | 3 (2.4–3.9) | 3 (2.0–4.3) | 3 (2.3–4.4) | 2 (0.9–3.5) | 2 (1.0–3.7) | 4 (2.7–6.6) | 5 (3.3–7.1)* | 3 (1.4-5.5) |
| Nightmares | 12 (10.1–13.8) | 11 (8.7–13.5) | 12.7 (10.5–15.3) | 16 (12.5–19.4)* | 14 (10.3–17.6) | 8 (5.2–11.1) | 11 (8.0–14.6) | 10 (6.9–14.2) |
| Bruxism | 7 (5.5–7.8) | 5 (3.9–6.9) | 8 (6.3–9.8)# | 6 (3.7–8.9) | 5 (3.5–7.1) | 8 (5.8–11.4) | 8 (5.7–11.3) | 6 (3.7–9.4) |
| Snoring | 25 (22.6–27) | 31 (27.6–34.5)# | 19 (16.2–21.9) | 11 (7.9–13.8) | 20 (16.5–24.7) | 31 (26.2–35.8) | 34 (29.5–39.2)* | 33 (26.7–38.9) |
| Moving a lot during sleep | 22 (19.9–25.0) | 22 (19.0–25.6) | 23 (20.0–25.4) | 25 (20.9–29.1) | 23 (18.7–26.9) | 23 (18.4–27.2) | 20 (15.9–24.6) | 22 (17.3–27.0) |
| Somnambulism | 1 (1.0–2.0) | 1 (0.5–1.8) | 2 (1.2–2.8) | 2 (1.2–4.5)* | 2 (1.0–3.5) | 2 (0.8–3.4) | 0.8 (0.2–2.4) | 0.4 (0.1–2.8) |
| Superficial sleep | 27 (24.3–30.0) | 23 (19.8–26.7) | 31 (27.3–34.4)# | 20 (16.4–24.3) | 24 (20.0–28.2) | 30 (25.7–35.6) | 29 (24.9–34.3) | 35 (28.7–42.0)* |
| Sweating while sleeping | 9 (7.7–11.1) | 9 (7.4–11.7) | 9 (7.2–11.5) | 7 (4.7–10) | 8 (5.9–11.5) | 9 (6.6–12.6) | 12 (9.4–16.2) | 10 (6.6–14.1) |
| No answer | 0.1 (0–0.4) | 0 | 0.1 (0.0–0.8) | – | – | – | – | 0.4 (0.1–2.8) |
p<0.05 increased observed frequency compared to expected frequency;
p<0.05 compared with the other gender.
Differences in gender were observed only for waking up with headache (χ2=30.6, df=2, p<0.0001), insomnia (χ2=16.4, df=8, p<0.05), bruxism (χ2=6.4, df=2, p<0.05), excessive daytime sleepiness (χ2=15.5, df=2, p<0.001), light sleep (χ2=14.8, df=2, p<0.0001) and snoring (χ2=37.0, df=2, p<0.0001). Except for snoring, all of these complaints were more frequent in women. In general, the occurrence of sleep complaints was higher in subjects aged 35–44 years compared to the other age groups (χ2=15.2, df=8, p<0.05). Sleep talking (χ2=34.7, df=8, p<0.0001), excessive daytime sleepiness (χ2=16.5, df=8, p<0.05), nightmares (χ2=20.2, df=8, p<0.01) and light sleep (χ2=30.7, df=8, p<0.0001) were more common in younger (16–24 years) subjects compared to the others. Urinary urgency (χ2=54.9, df=8, p<0.0001), insomnia (χ2=33.3, df=8, p<0.0001) and light sleep (χ2=30.7, df=8, p<0.0001) were more observed in older subjects (more than 60 years) compared to the others. Breathing pauses (χ2=90.6, df=8, p<0.0001) and snoring (χ2=90.6, df=8, p<0.0001) were more reported by subjects aged 45–59 years compared to the others. Among those that reported sleep complaints, the percentage of frequencies greater than 3 times per week was higher than 50% for most sleep problems, including urinary urgency, moving a lot during sleep, insufficient sleep, light sleep, snoring, sweating while sleeping, excessive daytime sleepiness, bruxism, kicking legs, and insomnia.
The regional distribution of sleep complaints was largely similar among Brazilian regions, with exception of insufficient sleep, insomnia, bruxism, moving a lot during sleep, and light sleep. In general, considering the presence of any sleep complaint, there was more subjects from Northeast compared to South region (χ2=16.1, df=6, p<0.01). Table 4 shows the characterization of sleep complaints in the Brazilian population according to occupational status, years of schooling, family monthly income and socioeconomic classes. Regarding occupational status, subjects that were working complained more about waking up with headaches (χ2=8.4, df=2, p<0.05), urinary urgency (χ2=20.9, df=2, p<0.0001), insomnia (χ2=8.9, df=2, p<0.01) and light sleep (χ2=5.7, df=2, p<0.05) compared to those not working. In addition, there was an association between lower education level (<8 years) and occurrence of urinary urgency (χ2=15.3, df=4, p<0.01), insomnia (χ2=14.2, df=4, p<0.01) and light sleep (χ2=19.6, df=4, p<0.001). However, presence of bruxism was associated with higher degree of schooling (>12 years) (χ2=17.7, df=4, p<0.001).
Table 4.
Prevalence of sleep complaints in the Brazilian population sample according to occupational status, years of schooling, family monthly income and socioeconomic classes (N=2017). Percentages (95% CI) were expanded using a weighted variable.
| Occupational status | Years of schooling | Family monthtly income | Socioeconomic classes | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Working | Not working | <8 years | 8–12 years | >12 years | ≤R$1244.00 | R$1245.00–6220.00 | >R$6221.00 | Upper (A+B) | Middle (C) | Lower (D+E) | |
| Any sleep complaint | 75 (70.7–78.6) | 76 (73.0–79.4) | 76 (72.1–79.2) | 76 (72.0–79.3) | 77 (68.5–83.1) | 72 (67.1–76.2) | 75 (70.9–79.1) | 85 (72.9–92.0)⁎ | 78 (73.2–81.6) | 76 (71.8–78.8) | 74 (69.0–78.8) |
| Waking up with headache | 12 (9.0–15.3)⁎ | 8 (6.8–10.0) | 11 (8.7–13.9) | 8 (6.6–10.2) | 8 (4.4–13.2) | 11 (8.5–14.0) | 9 (6.8–11.5) | 11 (5.3–19.9) | 9 (6.6–11.9) | 8 (6.6–10.1) | 13 (9.6–17.7) |
| Kicking legs | 7 (5.2–9.3) | 5.2 (4.0–6.6) | 6 (4.6–8.5) | 6 (4.2–7.4) | 4 (1.9–7.9) | 6 (3.8–7.8) | 6 (4.1–7.5) | 5 (2.0–12.0) | 5 (3.7–7.1) | 6 (4.6–7.9) | 6 (4.0–8.5) |
| Insufficient sleep | 22 (19.0–25.9) | 24 (21.2–26.8) | 21 (17.9–24.6) | 25 (21.6–27.6) | 28 (21.6–35.1) | 23 (19.2–27.7) | 24 (20.1–27.4) | 26 (22.7–29.8) | 22 (19.5–25.5) | 22 (17.3–27.1) | |
| Sleep talking | 9 (7.1–11.5) | 11 (8.9–12.6) | 9 (6.7–11.2) | 12 (9.7–14.2) | 8 (4.9–12.6) | 10 (7.5–12.4) | 11 (9.0–13.9) | 10 (5.7–17.2) | 9 (6.9–12.7) | 10 (8.7–12.3) | 11 (7.7–14.4) |
| Urinary incontinence | 8 (6.3–11.2)⁎ | 4 (2.7–4.9) | 7 (5.4–9.9)⁎ | 3 (2.4–4.7) | 4 (2.2–8.6) | 5 (3.5–7.3) | 4 (2.6–5.7) | 4 (1.2–10.3) | 3 (1.9–5.6) | 5 (3.9–7.3) | 7 (5.0–10.9)⁎ |
| Insomnia | 25 (21.4–28.5)⁎ | 20 (17.4–22.1) | 25 (22.2–28.5)⁎ | 19 (16.0–21.6) | 17 (13.0–22.0) | 23 (19.3–26.9)⁎ | 19 (15.8–22.3) | 13 (7.1–23.3) | 21 (17.8–23.7) | 20 (17.4–23.2) | 25 (21.0–30.0) |
| Excessive daytime sleepiness | 13 (10.5–16.0) | 12 (9.6–13.8) | 12 (9.5–14.5) | 12 (10.2–14.5) | 12 (7.6–18.3) | 12 (9.7–15.8) | 11 (8.6–13.2) | 9 (4.9–17.4) | 10 (8.1–13.4) | 13 (10.7–15.4) | 12 (9.1–15.7) |
| Breathing pauses | 3 (2.0–4.9) | 3 (2.2–4.1) | 3 (2.3–5.0) | 3 (1.9–4.0) | 3 (1.4–7.0) | 3 (1.5–4.3) | 3 (1.9–4.1) | 3 (0.6–9.7) | 3 (1.7–4.2) | 3 (1.9–4.1) | 4 (2.7–7.0) |
| Nightmares | 13 (10.1–16.2) | 11 (9.2–13.9) | 13 (10.1–15.4) | 13 (10.2–15.3) | 5 (2.4–9.2) | 14 (10.8–17.0) | 11 (8.2–13.3) | 12 (5.8–22.8) | 9 (6.7–12.0) | 12 (9.6–14.90 | 16 (11.8–20.8)⁎ |
| Bruxism | 6 (4.5–8.6) | 7 (5.5–8.2) | 5 (3.8–7.0) | 6 (5.0–8.2) | 14 (9.6–19.0)⁎ | 5 (3.6–6.9) | 8 (6.5–10.5) | 13 (8.2–20.1)⁎ | 10 (7.9–12.7)⁎ | 6 (4.4–7.5) | 3 (1.8–5.9) |
| Snoring | 22 (18.7–25.6) | 26 (23.5–28.7) | 28 (24.5–31.5) | 22 (19.1–24.8) | 26 (20.2–33.4) | 20 (16.6–23.0) | 27 (22.9–30.4) | 32 (22.3–42.7)⁎ | 27 (23.4–30.6) | 23 (20.7–26.4) | 25 (20.3–30.4) |
| Moving a lot during sleep | 23 (20.0–27.2) | 22 (19.2–24.9) | 21 (17.9–25.4) | 24 (21.1–27.3) | 17 (12.4–23.4) | 22 (18.5–26.5) | 22 (18.4–25.5) | 16 (10.8–23.0) | 21 (17.9–24.4) | 23 (20.4–26.7) | 22 (17.2–27.3) |
| Somnambulism | 1 (0.5-2.2) | 2 (1.1–2.4) | 1 (0.6–2.2) | 2 (1.2–2.7) | 1 (0.1–4.3) | 1 (0.7–2.5) | 2 (0.9–2.8) | 1 (0.2–7.2) | 1 (0.7–2.6) | 2 (1.0–2.7) | 1 (0.3–2.5) |
| Superficial sleep | 30 (25.7)⁎ | 26 (22.7–29.0) | 32 (27.6–35.9)⁎ | 25 (21.7–28.2) | 18 (13.1–23.8) | 28 (23.7–33.2)⁎ | 23 (19.6–26.9) | 16 (9.5–26.8) | 22 (18.3–25.9) | 28 (24.7–31.6) | 32 (27.0–38.1)⁎ |
| Sweating while sleeping | 9 (6.8–12.2) | 9 (7.5–11.4) | 11 (8.9–14.5) | 8 (6.2–10.4) | 6 (3.0–10.4) | 8 (5.7–11.8) | 9 (7.2–12.0) | 8 (3.5–15.4) | 10 (7.3–12.1) | 9 (6.8–11.5) | 10 (6.9–13.5) |
| No answer | 0.2 (0.0–1.2) | – | 0.1 (0.0–0.9) | – | – | – | 1 (0.1–6.5) | – | – | 0.1 (0.0–0.7) | – |
p<0.05 increased observed frequency compared to expected frequency.
In general, the family monthly income influenced sleep complaints. An association was observed between higher family income and the presence of any sleep complaint (χ2=21.5, df=6, p<0.001) as well as insufficient sleep (χ2=24.9, df=6, p<0.0001), snoring (χ2=24.3, df=6, p<0.01) and bruxism (χ2=23.1, df=6, p<0.001). On the other hand, insomnia (χ2=23.3, df=6, p<0.001) and light sleep (χ2=21.0, df=6, p<0.01) were more observed in subjects with lower family income. Also, an association between lower socioeconomic class and sleep complaints such as urinary urgency (χ2=8.7, df=4, p<0.05), nightmares (χ2=10.5, df=4, p<0.05) and light sleep (χ2=14.1, df=4, p<0.01) was found. The presence of bruxism was associated with upper socioeconomic class (χ2=18.1, df=4, p<0.001).
To better understand the interaction effects between family income and region, a two-way ANOVA analysis was performed with the total number of complaints per person as dependent variable (Table 5) showing that within people who had lower family income, those living in Northeast and Southeast had more sleep complaints compared to the population from South.
Table 5.
Interaction between region and family monthly income in the number of sleep complaints in the population (N=1453).
| Region | Family monthtly income | Mean±SEM (95% CI) |
|---|---|---|
| Center-west and North | Up to R$ 1244.00 | 1.6±0.2 (1.3–2.0) |
| Between R$1245.00–6220.00 | 1.6±0.2 (1.3–2.0) | |
| More than R$ 6221,00 | 2.9±0.5 (1.9–4.0)⁎ | |
| Northeast | Up to R$1244.00 | 2.1±0.1 (1.9–2.4)# |
| Between R$1245.00 and 6220.00 | 1.9±0.1 (1.9–2.4) | |
| More than R$6221.00 | 1.7±0.6 (0.4–2.9) | |
| Southeast | Up to R$1244.00 | 2.0±0.1 (1.7–2.2)# |
| Between R$1245.00 and 6220.00 | 2.0±0.1 (1.8–2.2) | |
| More than R$6221.00 | 1.7±0.3 (1.2–2.2) | |
| South | up to R$1244.00 | 1.2±0.2 (0.7–1.6) |
| Between R$1245.00 and 6220.00 | 1.8±0.2 (1.4–2.1) | |
| More than R$6221.00 | 1.7±0.5 (0.6–2.7) | |
p<0.05 compared to up lower income in the Center-west and North region;
p<0.05 compared to South.
4. Discussion
The present study examined self-reported sleep complaints in a representative sample of the Brazilian population. The findings showed that each subject had approximately 2 sleep complaints on average, and 76% of the population presented at least 1 sleep related problem. In addition, the number of sleep complaints was higher in women and increased with age, being influenced by low income in Northeast and Southeast regions. The most common complaints were light and insufficient sleep, snoring, moving a lot during sleep and insomnia. Only insomnia and light sleep were associated with lower education and economic conditions while insufficient sleep, bruxism and snoring were associated with higher family income. In general, insufficient sleep and light sleep frequently occurred together with snoring and insomnia.
Compared to the last national survey performed in 2008 [6], an apparent increase of 13% was observed in the frequency of sleep complaints after 4 years, corresponding approximately to an incidence of 29 million Brazilian inhabitants. However, due mainly to the differences in the quantity of screening questions about sleep problems presented for the subjects in the 2 surveys (5 versus 15 items), we cannot appropriately compare these results. Therefore, this may explain why the overall prevalence of sleep problems was higher, although the prevalence estimates for insomnia, snoring, nightmares, kicking legs and breathing pauses were lower in the current study compared to the last one [6].
In agreement with many studies [6,7,34], sleep complaints increased with age and were more prevalent in individuals within 35–44 years, which corresponds to the most economically active group in the current society. Moreover, we found that gender affected sleep, as women reported more sleep problems than men. Grandner and colleagues [13] also demonstrated more sleep problems in women, but in this study the authors showed that people between the ages of 18 and 24 years reported more sleep complaints than older people. Although sleep complaints generally increased with age, some sleep complaints such as sleep talking, excessive daytime sleepiness, nightmares and somnambulism were more prevalent in younger (16–24 years) than older subjects.
The prevalence of insomnia complaint in the current study was high (21%), more frequent in women (24%) and older subjects (30%), according to other studies [6,8,17,19,20,27,38]. In contrast, a recent study revealed a low prevalence of 5.7% for insomnia in Germany [36]. In this study, women were twice as likely to be affected by insomnia as men, but no significant age differences were observed. Additionally, persons with low socioeconomic status had 3 times greater risk of insomnia [36]. Our study also showed the influence of socioeconomics on the prevalence of insomnia complaint, since the majority of people with insomnia complaint had lower educational level (<8 years) and lower income. Indeed, a study by Lalluka and colleagues (2010) demonstrated that past and present economic difficulties were strongly associated with current complaints of insomnia. Also, some evidence has shown that individuals with fewer years of schooling experience greater subjective impairment because of their insomnia [11], and unemployment or socioeconomic deprivation are strongly associated with insomnia symptoms [30].
In the current study, working people complained more about insomnia than those not working, possibly due to higher levels of stress. In contrast, a recent study showed that subjective insomnia was associated with non-working people with lower education levels [8].
Snoring was the second more frequent sleep complaint after light sleep, with a prevalence of 25%, being significantly higher in subjects older than 45 years old (34%) and men, in agreement with the previous literature [3,7,6,28,37]. As expected, reports of breathing pauses were not frequent (3%) in the population, since they are more commonly reported by partners [2]. However, they were associated with snoring complaints due to its relationship with obstructive sleep apnea. In general, snoring was more prevalent in subjects with higher income (32%). However, Tufik and colleagues (2010) demonstrated that only in men, obstructive sleep apnea is associated with high socioeconomic status, while in women it is associated with lower income. Although compared with the first national survey [6] no increase was observed in snoring prevalence, Peppard et al. [31] found an increase of approximately 14% in the prevalence of respiratory sleep disorders in the past 2 decades.
We found a 7% prevalence of bruxism in the Brazilian population, which is in line with previous studies [24,29]. In the current study, women (8%) were more affected than men (5%), as already shown by others [1,26]. However, in a representative sample of São Paulo, Maluly and colleagues (2013) demonstrated no significant differences in bruxism prevalence between genders. In this study, besides the subjective evaluation of clenching or grinding teeth, the authors also used polysomnography as an objective and confirmatory criterion for bruxism diagnosis, reducing the prevalence from 12.5% (subjective only) to 5.5% (subjective+objective). Thus, it is plausible to expect that in the current study less than 7% did have a diagnosis of bruxism.
There is evidence of an association between bruxism and tension, stress, and emotional disturbance [33]; however the influence of socioeconomic status is less clear [4,25]. Of note, our study showed that the presence of bruxism was associated with higher income and socioeconomic class as well as increased educational level in Brazil. This agrees with the results of previous studies, which also showed that individuals with bruxism have on average higher degree of schooling (more than 9 years) and income [24]. Another sleep complaint that was also associated with higher income as well as the working population is waking up with a headache. Its prevalence (9%) was higher than bruxism in the Brazilian population, and it affected more women than men, in agreement with a previous study [22]. Nevertheless, other evidence has demonstrated an absence of gender predilection [12].
In relation to the general socioeconomic context, our study demonstrated an interaction with region, showing in general that individuals with lower income from Northeast and Southeast had more sleep complaints compared to those from South. Previous studies indicate that individuals with higher socioeconomic status and education levels sleep better than those of lower socioeconomic status [10,13]. Indeed, lower socioeconomic condition is related to many intrinsic factors that can cause poor sleep such as illness, fewer support systems, depression, anxiety, lower quality of life, and less motivation to see sleep as a priority [13]. A number of extrinsic factors may also negatively affect sleep as well, such as work schedules, family demands, limited access to healthcare, and unemployment [13]. Thus, the interaction found between region and income in the current study may be explained by the economic growth of Brazil, which since 2010 has been part of BRICS, the 5 newly emerging economies (Brazil, India, Russia, China and South Africa) [14]. This rapid and constant growth consequently led the country to a great expansion of life in large urban centers, associated with stressful situations such as traffic jams, crowded public transportation systems, and excessive workload, mainly in the Southeast region, which is the economic axis and contains the biggest metropolis of Brazil: São Paulo. These changes might increase the stress levels of many people, contributing to more sleep problems in the population. Thus, it is important to highlight that socioeconomic status effects on sleep also depended from the region. When considering the population with lower family income, we found that those living in Northeast (the poorest region of Brazil with the lowest education level) and in Southeast (the most populous and developed region of Brazil) had increased number of sleep complaints compared to the South region. In turn, in the South, which has the highest educational level and lowest poverty rate (www.ibge.com.br), people had fewer sleep complaints, possibly as a reflection of better sleep quality and more favorable socioeconomic status.
Notably, the 2 most prevalent sleep symptoms were light and insufficient sleep, possibly as a consequence of increased sleep disorders and the modern 24/7 society, where sleep is highly neglected. In fact, sleep deprivation is a common occurrence in modern culture. Increased workloads due to socioeconomic pressure and decreased time to complete it result in extended periods of wakefulness, decreases in sleep quality and ultimately a condition of sleep restriction [23]. Indeed, less sleep is associated with increased workload as well as low education level and income [18].
This study has some limitations. First, the questions included in face-to-face interviews are not specific to a particular sleep symptom, which limits the ability to characterize sleep disorders, although the utility of this approach for epidemiology is high as it provides low-cost information on sleep pattern from distinct populations. Second, we cannot be sure of the increased trend of sleep complaints in comparison to the first national survey, since the number of questions differed between the 2 studies. Third, socioeconomic factors affecting sleep might be also influenced by confounding factors, such as medical treatment, obesity and other concomitant diseases, which were not evaluated in the current study. In addition, socioeconomic condition may also modulate some answers of the volunteers in the face-to-face questions. Finally, future study using a reliable and valid questionnaire as well as assessing medical condition, medication, and mental disorders would be worth.
In summary, sleep quality seems to be affected in the majority of Brazilian population and that they might interact with the socioeconomic factors. Since sleep insufficiency is linked to motor vehicle crashes, industrial disasters, and medical and other occupational errors, sleep has been recognized as important to public health. As people experiencing sleep insufficiency are more likely to suffer from chronic diseases, increased mortality, and reduced productivity [21], the current study adds to the evidence for the societal burden of sleep complaints, and suggests that distinct strategies for effective treatment and intervention are necessary and depend on sociodemographic factors.
Conflict of interest
All authors have no financial conflicts of interest to disclose.
Acknowledgments
This work was financially supported by Associação Fundo de Incentivo a Pesquisa (AFIP). We thank Altay Alves Lino de Souza and Instituto Datafolha for their important support in the current study. LB, MLA and ST are recipients of CNPq fellowship (#300674/2013-9 to LB, #305177/2013-3 to MLA, and #301974/2011-0 to ST).
References
- 1.Ahlberg J., Rantala M., Savolainen A., Suvinen T., Nissinen M., Sarna S. Reported bruxism and stress experience. Community Dent Oral Epidemiol. 2002;30:405–408. doi: 10.1034/j.1600-0528.2002.00007.x. [DOI] [PubMed] [Google Scholar]
- 2.American Academy of Sleep Medicine. International classification of sleep disorders: diagnostic and coding manual. Illinois: Westchester; 2005.
- 3.Ansarin K., Sahebi L., Sabur S. Obstructive sleep apnea syndrome: complaints and housing characteristics in a population in the United States. Sao Paulo Med J. 2013;131:220–227. doi: 10.1590/1516-3180.2013.1314451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Antonio A.G., Pierro V.S., Maia L.C. Bruxism in children: a warning sign for psychological problems. J Can Dent Assoc. 2006;72:155–160. [PubMed] [Google Scholar]
- 5.Banks S., Dinges D. Behavioral and physiological consequences of sleep restriction. J Clin Sleep Med. 2007;3:519–528. [PMC free article] [PubMed] [Google Scholar]
- 6.Bittencourt L.R., Santos-Silva R., Taddei J.A., Andersen M.L., de Mello M.T., Tufik S. Sleep complaints in the adult Brazilian population: a national survey based on screening questions. J Clin Sleep Med. 2009;5:459–463. [PMC free article] [PubMed] [Google Scholar]
- 7.Bixler E.O., Vgontzas A.N., Ten Have T., Tyson K., Kales A. Effects of age on sleep apnea in men: I. Prevalence and severity. Am J Respir Crit Care Med. 1998;157:144–148. doi: 10.1164/ajrccm.157.1.9706079. [DOI] [PubMed] [Google Scholar]
- 8.Castro L.S., Poyares D., Leger D., Bittencourt L., Tufik S. Objective prevalence of insomnia in the Sao Paulo, Brazil epidemiologic sleep study. Ann Neurol. 2013;74:537–546. doi: 10.1002/ana.23945. [DOI] [PubMed] [Google Scholar]
- 9.dos Santos A.A., Ceolim. M.F., Neri A.L. Sleep complaints among Brazilian senior citizens from municipalities with different human development indices. Rev Lat Am Enfermagem. 2012;20:917–926. doi: 10.1590/s0104-11692012000500014. [DOI] [PubMed] [Google Scholar]
- 10.Friedman E.M., Love G.D., Rosenkranz M.A., Urry H.L., Davidson R.J., Singer B.H. Socioeconomic status predicts objective and subjective sleep quality in aging women. Psychosom Med. 2007;69:682–691. doi: 10.1097/PSY.0b013e31814ceada. [DOI] [PubMed] [Google Scholar]
- 11.Gellis L.A., Lichstein K.L., Scarinci I.C., Durrence H.H., Taylor D.J., Bush A.J. Socioeconomic status and insomnia. J Abnorm Psychol. 2005;114:111–118. doi: 10.1037/0021-843X.114.1.111. [DOI] [PubMed] [Google Scholar]
- 12.Gori S., Lucchesi C., Morelli N., Maestri M., Bonanni E., Murri L. Sleep-related migraine occurrence increases with aging. Acta Neurol Belgica. 2012;112:183–187. doi: 10.1007/s13760-012-0049-6. [DOI] [PubMed] [Google Scholar]
- 13.Grandner M.A., Patel N.P., Gehrman P.R., Xie D., Sha D., Weaver T. Who gets the best sleep? Ethnic and socioeconomic factors related to sleep complaints. Sleep Med. 2010;11:470–478. doi: 10.1016/j.sleep.2009.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Harmer A., Xiao Y., Missoni E., Tediosi F. BRICS without straw? A systematic literature review of newly emerging economies’ influence in global health. Glob. Health. 2013;9:15. doi: 10.1186/1744-8603-9-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hillman D.R., Lack L.C. Public health implications of sleep loss: the community burden. Med J Aust. 2013;199:S7–S10. doi: 10.5694/mja13.10620. [DOI] [PubMed] [Google Scholar]
- 16.Kish L. John Wiley, Sons Inc; New York: 1965. Survey Sampling. [Google Scholar]
- 17.Klink M.E., Quan S.F., Kaltenborn W.T., Lebowitz M.D. Risk factors associated with complaints of insomnia in a general adult population. Influence of previous complaints of insomnia. Arch Intern Med. 1992;152:1634–1637. [PubMed] [Google Scholar]
- 18.Krueger P.M., Friedman E.M. Sleep duration in the United States: a cross-sectional population-based study. Am J Epidemiol. 2009;169:1052–1063. doi: 10.1093/aje/kwp023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lallukka T., Arber S., Rahkonen O., Lahelma E. Complaints of insomnia among midlife employed people: the contribution of childhood and present socioeconomic circumstances. Sleep Med. 2010;11:828–836. doi: 10.1016/j.sleep.2010.04.011. [DOI] [PubMed] [Google Scholar]
- 20.Lallukka T., Sares-Jaske L., Kronholm E., Saaksjarvi K., Lundqvist A., Partonen T. Sociodemographic and socioeconomic differences in sleep duration and insomnia-related symptoms in Finnish adults. BMC Public Health. 2012;12:565. doi: 10.1186/1471-2458-12-565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Leproult R., Van Cauter E. Role of sleep and sleep loss in hormonal release and metabolism. Endocr Dev. 2010;17:11–21. doi: 10.1159/000262524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lucchesi L.M., Speciali J.G., Santos-Silva R., Taddei J.A., Tufik S., Bittencourt L.R. Nocturnal awakening with headache and its relationship with sleep disorders in a population-based sample of adult inhabitants of Sao Paulo City, Brazil. Cephalalgia. 2010;30:1477–1485. doi: 10.1177/0333102410368440. [DOI] [PubMed] [Google Scholar]
- 23.Malik S.W., Kaplan J. Sleep deprivation. Prim Care. 2005;32:475–490. doi: 10.1016/j.pop.2005.02.011. [DOI] [PubMed] [Google Scholar]
- 24.Maluly M., Andersen M.L., Dal-Fabbro C., Garbuio S., Bittencourt L., de Siqueira J.T. Polysomnographic study of the prevalence of sleep bruxism in a population sample. J Dent Res. 2013;92:97S–103S. doi: 10.1177/0022034513484328. [DOI] [PubMed] [Google Scholar]
- 25.Manfredini D., Lobbezoo F. Role of psychosocial factors in the etiology of bruxism. J Orofac Pain. 2009;23:153–166. [PubMed] [Google Scholar]
- 26.Nekora-Azak A., Yengin E., Evlioglu G., Ceyhan A., Ocak O., Issever H. Prevalence of bruxism awareness in Istanbul, Turkey. Cranio. 2010;28:122–127. doi: 10.1179/crn.2010.017. [DOI] [PubMed] [Google Scholar]
- 27.Ohayon M.M. Epidemiology of insomnia: what we know and what we still need to learn. Sleep Med Rev. 2002;6:97–111. doi: 10.1053/smrv.2002.0186. [DOI] [PubMed] [Google Scholar]
- 28.Ohayon M.M., Guilleminault C., Priest R.G., Zulley J., Smirne S. Is sleep-disordered breathing an independent risk factor for hypertension in the general population, 13,057 subjects? J Psychosom Res. 2000;48:593–601. doi: 10.1016/s0022-3999(00)00142-2. [DOI] [PubMed] [Google Scholar]
- 29.Ohayon M.M., Li K.K., Guilleminault C. Risk factors for sleep bruxism in the general population. Chest. 2001;119:53–61. doi: 10.1378/chest.119.1.53. [DOI] [PubMed] [Google Scholar]
- 30.Paine S.J., Gander P.H., Harris R., Reid P. Who reports insomnia? Relationships with age, sex, ethnicity, and socioeconomic deprivation. Sleep. 2004;27:1163–1169. doi: 10.1093/sleep/27.6.1163. [DOI] [PubMed] [Google Scholar]
- 31.Peppard P.E., Young T., Barnet J.H., Palta M., Hagen E.W., Hla K.M. Increased prevalence of sleep-disordered breathing in adults. Am J Epidemiol. 2013 doi: 10.1093/aje/kws342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ram S., Seirawan H., Kumar S.K., Clark G.T. Prevalence and impact of sleep disorders and sleep habits in the United States. Sleep Breath. 2010;14:63–70. doi: 10.1007/s11325-009-0281-3. [DOI] [PubMed] [Google Scholar]
- 33.Renner A.C., da Silva A.A., Rodriguez J.D., Simoes V.M., Barbieri M.A., Bettiol H. Are mental health problems and depression associated with bruxism in children? Community Dent Oral Epidemiol. 2012;40:277–287. doi: 10.1111/j.1600-0528.2011.00644.x. [DOI] [PubMed] [Google Scholar]
- 34.Roepke S.K., Ancoli-Israel S. Sleep disorders in the elderly. Indian J Med Res. 2010;131:302–310. [PubMed] [Google Scholar]
- 35.Santos-Silva R., Bittencourt L.R., Pires M.L., de Mello M.T., Taddei J.A., Benedito-Silva A.A. Increasing trends of sleep complaints in the city of Sao Paulo, Brazil. Sleep Med. 2010;11:520–524. doi: 10.1016/j.sleep.2009.12.011. [DOI] [PubMed] [Google Scholar]
- 36.Schlack R., Hapke U., Maske U., Busch M., Cohrs S. Frequency and distribution of sleep problems and insomnia in the adult population in Germany: results of the German Health Interview and Examination Survey for Adults, DEGS1. Bundesgesundheitsblatt Gesundh Gesundh. 2013;56:740–748. doi: 10.1007/s00103-013-1689-2. [DOI] [PubMed] [Google Scholar]
- 37.Tufik S., Santos-Silva R., Taddei J.A., Bittencourt L.R. Obstructive sleep apnea syndrome in the Sao Paulo epidemiologic sleep study. Sleep Med. 2010;11:441–446. doi: 10.1016/j.sleep.2009.10.005. [DOI] [PubMed] [Google Scholar]
- 38.Wong W.S., Fielding R. Prevalence of insomnia among Chinese adults in Hong Kong: a population-based study. J Sleep Res. 2011;20:117–126. doi: 10.1111/j.1365-2869.2010.00822.x. [DOI] [PubMed] [Google Scholar]