Abstract
Background
The adult myeloid diseases, myelodysplastic syndrome and acute myeloid leukemia, have been reported to be associated with cigarette smoking, but the results have been conflicting. Previous studies may have ignored the relationship between myelodysplastic syndrome and acute myeloid leukemia, where approximately one-third of myelodysplastic syndrome cases will progress to acute myeloid leukemia, which could induce a serious bias in independent analyses. For the purposes of researching pathogenesis, we suggest that myelodysplastic syndrome and acute myeloid leukemia should be regarded as a single class of adult myeloid disease, and herein assessed the relationship between cigarette smoking and the risk of adult myeloid disease.
Methods
The PubMed, Cochrane Library, EBSCO, and EMBASE databases were systematically searched for reports published from 1990 to 2015. Two authors independently assessed the methodological quality and the extracted data. The odds ratios and adjusted odds ratios (OR), a sensitivity analysis, and the publication bias were analyzed using the CMA v2 (Comprehensive Meta Analysis Version 2) software program.
Results
Twenty-five studies were included in this meta-analysis. The publication dates ranged from 1990 to 2014. The pooled OR in current smokers and ever-smokers showed an increased risk of adult myeloid disease, with ORs of 1.45 (95% CI, 1.30–1.62; p<0.001) and 1.23 (95% CI 1.15–1.32; p<0.001) versus non-smokers, respectively. In the subset analyses, the OR of adult myeloid disease was increased regardless of the form of disease, geographical region, NOS (Newcastle Ottawa Scale) score, and source of controls. The smoking status was divided into <20 and ≥20 cigarettes per day, and these groups had ORs of developing adult myeloid disease of 1.24 (95% CI, 1.09–1.40; p = 0.001) and 1.32 (95% CI, 1.14–1.53; p<0.001), respectively. In the groups divided based on the number of years the subjects had smoked (<20 and ≥20 years), the ORs were 1.05 (95% CI, 0.90–1.23; p = 0.25) and 1.30 (95% CI, 1.16–1.45; p<0.001), respectively. Similarly, <20 and ≥20 pack-years were associated with ORs of 1.15 (95% CI, 1.03–1.29; p = 0.017) and 1.34 (95% CI, 1.18–1.52; p<0.001), respectively.
Conclusions
This meta-analysis, for the first time, combined myelodysplastic syndrome with acute myeloid leukemia to assess the overall risk of adult myeloid disease, and it demonstrated that cigarette smoking is associated with a significantly increased risk of adult myeloid disease.
Introduction
Adult myeloid diseases are a group of clonal diseases that affect the stem cells in bone marrow. Among the adult myeloid diseases, myelodysplastic syndrome (MDS) and acute myeloid leukemia (AML) have high incidence rates of 4 and 3.7 per 100,000 people, respectively. Moreover, the number of MDS cases reaches 40–50 per 100,000 in patients older than 70 years old [1, 2]. The median age at diagnosis is approximately 67 and 76 years for AML and MDS, and the conditions tend to occur earlier in Asian populations [2–5]. In addition, men have a significantly higher incidence rate than women [4, 5]. A striking feature of MDS is its genetic instability, and approximately one-third of MDS cases result in AML [2, 6–10]. The pathogenesis of MDS or AML is uncertain, particularly why MDS can transform into AML.
Tobacco is an established factor that can cause carcinogenicity, teratogenicity and mutagenicity. Up to half of current smokers will eventually die of a tobacco-related disease [11]. The monograph by the International Agency for Research on Cancer (IARC), the National Comprehensive Cancer Network Clinical Practice Guidelines (NCCN Guidelines) and the European Society for Medical Oncology Practice Guidelines (ESMO Guidelines) reported that adult myeloid disease is linked to smoking [3, 10, 12]. Attributable risk calculations suggest that about 15% of all leukemia deaths and 24% of myeloid leukemia deaths are accounted for as a result of cigarette smoking[13].
Since the strongest evidence comes from cohort studies, some data were also available from case-control studies. Early in 1978, Paffenbarger [14] found that cigarette smoking was related to AML. Many subsequent case-control studies focused on investigating the relationship between cigarette smoking and the risk of AML or MDS, but the results had significant bias [15–18]. Fircanis [19] evaluated the relationship between smoking and AML, and Tong [20] investigated the relationship between smoking and MDS. However, neither of these researchers examined the interrelationship between MDS and AML, wherein approximately one-third of MDS cases transform into AML. Independent analyses of AML or MDS alone cannot accurately assess the association with smoking. In fact, both AML and MDS show identical cellular morphology, clonal hyperplasia of myeloblast. The number of myeloblasts is considered as one of important differential features between them. Myeloblasts are less than 20% in MDS, nevertheless more than 20% in AML [21]. We thought that MDS and AML should be grouped together as a single class of “adult myeloid disease” for the purposes of researching pathogenesis, and we herein assessed the relationship between cigarette smoking and the risk of developing adult myeloid disease.
Materials and Methods
Literature search and study selection
A systematic literature search was conducted by two independent reviewers (Wang and Liu) of the PubMed, Cochrane Library, EMBASE and EBSCO databases for papers published from 1990 to 2015. The following search terms were used: (1) “AML” OR “acute myeloid leukemia” or “myelodysplastic syndrome” OR “MDS” OR “myelodysplastic” OR “myelodysplasia” OR “preleukemia”; (2) “smoking” OR “tobacco” OR “cigarette”. These search themes were combined using the Boolean operator “and” in several combinations without restrictions. In addition, the references reported in the identified studies were used to complete the search.
Studies eligible for inclusion in this meta-analysis met the following criteria: (1) the study design was a case-control study; (2) investigated the association between smoking and the risk of AML or MDS; (3) the case and control of studies must have been based on adults; (4) the diagnoses of AML and MDS were confirmed either histologically, pathologically, cytologically or by detailed medical records; (5) the odds ratios (OR) and the number of events could be calculated from the data presented;(6) published as a full text document in English. Two reviewers (Liu and Jiang) determined the study eligibility independently. Disagreements were resolved by consensus.
Data extraction and quality assessment
Two investigators (Liu and Jiang) read the full text of the manuscripts independently and extracted the following data from each eligible study: first author’s name, publication year, country of origin, study period, source of controls, sample size, method of ascertainment of smoking, method of ascertainment of adult myeloid disease and the Newcastle Ottawa Scale (NOS) score [22]. The NOS score usually is used for assessing the quality of nonrandomized studies (case-control and cohort studies) in meta-analyses. To assess the quality of these studies, two reviewers (Liu and Jiang) independently read and scored each study according to the NOS [22]. NOS scores of 1–3, 4–6, and 7–9 were considered to indicate low, medium and high quality, respectively.
Statistical analysis
We calculated the pooled odds ratios (OR) with the 95% CI by using the Comprehensive Meta-Analysis software program (Version 2.2.064 July 27, 2011). The statistical heterogeneity within studies was evaluated using a χ2-based Cochran’s Q statistic [23] and was further quantified using I 2 statistics (I 2 = 0–25%, no heterogeneity; I 2 = 25–50%, moderate heterogeneity; I 2 = 50–75%, large heterogeneity; and I 2 = 75–100%, extreme heterogeneity. For values of I 2 ≤ 50%, the fixed-effects model was used; I 2 ≥ 50%, the random-effects model was used) [23]. To investigate the potential heterogeneity, we also conducted a subgroup analysis based on the following four aspects: forms of disease, geographical region, source of controls and the NOS score. Publication bias was examined by Egger’s regression and Begger’s funnel plot (p ≤ 0.05 was considered to indicate the presence of significant publication bias) [24] and was adjusted by Duval and Tweedie’s trim-and-fill method [25]. A sensitivity analysis was performed to evaluate the potential effects of the removal of one study in each turn. If the outcome was significantly changed after one study was removed, then the study was excluded from the included studies due to selection bias, and a new analysis was conducted.
Results
Literature search
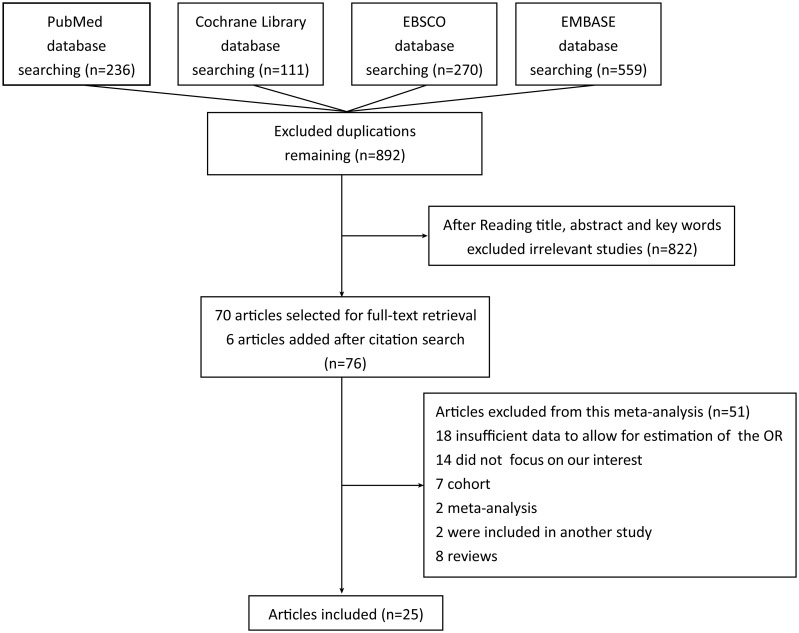
There were twenty-five articles included in our meta-analysis [15–18, 26–46]. Two reviewers assessed seventy-six articles independently and excluded fifty-one articles. The reasons for exclusion of the articles were as follows: insufficient data to allow for estimation of the OR for eighteen studies, fourteen studies did not focus on our topic of interest, seven were based on cohort studies, ten were meta-analyses or reviews, and two were included in another article. Our search flow is shown in Fig 1.
Fig 1. A flowchart of the study selection process.
Characteristics of the included studies
The main characteristics of the included studies are shown in Table 1. Studies were published from 1990 to 2014. There were ten [16–18, 30, 32–35, 40, 41] studies performed in Europe, ten [26–29, 36–39, 45, 46] in North America and five [15, 31, 42–44] performed in Asia. A total of 8,074 adult myeloid disease cases and 31,805 controls were included in our meta-analysis. The controls of twenty-five studies came from different sources: fourteen [15, 16, 18, 26–29, 33, 34, 36, 38, 41, 45, 46] were population-based, ten [30–32, 35, 37, 39, 40, 42–44] were hospital-based, and only one [17] came from both a population and hospital. Cases in all included studies were confirmed mainly according to one method or several methods combined based on medical records, pathological and cytogenetic findings. Smoking factors were evaluated using the medical records in six [18, 27, 31, 35, 37, 44] studies, questionnaires in three [15, 39, 46] studies, personal interviews in twelve [16, 17, 28, 30, 32, 34, 36, 40–43, 45] studies, telephone interviews in three [26, 29, 33] studies and one [38] study included both a questionnaire and telephone interview. The data about matching were extracted from all of the included studies. According to the Newcastle-Ottawa Scale quality assessment system, sixteen [16, 17, 27–29, 34–36, 38–43, 45, 46] studies were high quality (NOS score ≥7), eight [15, 18, 26, 30, 32, 33, 37, 44] studies were medium quality (NOS score ≥4 and ≤6) and one study [31] was low quality (NOS = 3). Overall, the average score of all included studies was 6.68.
Table 1. Characteristics of the included studies.
| Study | Year | Country | Period | Groups | Source of controls | Age (years) | No. of subjects | Adult myeloid disease confirmation | Smoking evaluation | Matching | NOS |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Wilson | 2014 | UK | 1990–2009 | Control | PB | 20–79 | 3417 | Medical records | Medical records | Age, sex, index date | 6 |
| MDS | 849 | ||||||||||
| Musselman | 2013 | USA | 2005–2009 | Control | PB | 20–79 | 692 | Cytogenetic results integrated with pathologically confirmed | Self-administered questionnaire | Age, sex, and BMI | 9 |
| AML | 414 | ||||||||||
| Strom | 2012 | USA | 2003–2007 | Control | PB | 18–80 | 636 | Pathologically confirmed | Personal interviews | Age, sex, race, county of residence | 7 |
| AML | 638 | ||||||||||
| Kim | 2012 | Korea | 1997–2008 | Control | HB | 50.5±16.9 | 1700 | Pathologically confirmed | Medical records | Age, sex | 5 |
| AML | 415 | ||||||||||
| Lv | 2011 | China | 2003–2006 | Control | HB | ≥18 | 806 | Pathologically confirmed | Face-to-face interviews | Age, sex | 7 |
| MDS | 403 | ||||||||||
| Wong | 2009 | China | 2003–2007 | Control | HB | ≥18 | 1444 | Pathologically and cytogenetic confirmed | Personal blinded interviews | Age, sex | 8 |
| AML | 722 | ||||||||||
| Bjork | 2009 | Sweden | 2001–2004 | Control | PB&HB | ≥20 | 278 | Medical records | Face-to-face interviews | Age, sex, county of residence | 8 |
| AML | 104 | ||||||||||
| MDS | 75 | ||||||||||
| Richardson | 2008 | Germany | 1986–1998 | Control | PB | 53.5±14 | 266 | Medical records | Face-to-face interviews | Year of birth, sex, region | 8 |
| ANLL | 120 | ||||||||||
| Pekmezovic | 2006 | Serbia, Montenegro | 2000–2003 | Control | HB | 20–85 | 160 | Pathologically confirmed supplemented by medical records | Personal interviews, supplemented by medical records | Age, sex | 7 |
| MDS | 80 | ||||||||||
| Kasim | 2005 | Canada | 1994–1997 | Control | PB | 20–74 | 5039 | Pathologically confirmed | Mailed questionnaires with telephone follow-up | Age, sex, body mass index | 8 |
| AML | 307 | ||||||||||
| Strom | 2005 | USA | 1999–2003 | Control | HB | 24–89 | 452 | Pathologically confirmed | Mailed questionnaires | Age, sex, ethnicity | 7 |
| MDS | 354 | ||||||||||
| Speer | 2002 | USA | 1984–1993 | Control | HB | Median age (65) | 7107 | Medical records | Medical records | Age, sex | 5 |
| AML | 604 | ||||||||||
| Pogoda | 2002 | USA | 1987–1994 | Control | PB | 25–75 | 412 | Pathologically confirmed | Non-blinded interviews | Birth year, sex, race | 7 |
| AML | 412 | ||||||||||
| Dalamaga | 2002 | Greek | 1995–2000 | Control | HB | 44–85 | 84 | Pathologically confirmed supplemented by cytogenetic | Medical records | Age, sex | 7 |
| MDS | 84 | ||||||||||
| Stagnaro | 2001 | Italy | 1990–1993 | Control | PB | 20–74 | 1779 | Pathologically confirmed | Blind interviews | Age, sex, area of residence, education level, type of interview | 8 |
| AML | 223 | ||||||||||
| Bjork | 2001 | Sweden | 1976–1993 | Control | PB | 35–76 | 351 | Pathologically confirmed supplemented by cytogenetic | Structured telephone interview | Age, sex, county of residence | 6 |
| AML | 333 | ||||||||||
| Nisse | 2001 | France | 1991–1996 | Control | PB | 62–74 | 204 | Pathologically confirmed | Personal interviews | Age, sex | 7 |
| MDS | 204 | ||||||||||
| Nagata | 1999 | Japan | 1995–1996 | Control | PB | 20–74 | 830 | Pathologically confirmed | Mailed questionnaire | Sex, region | 6 |
| MDS | 111 | ||||||||||
| West | 1995 | UK | NA | Control | HB | ≥15 | 399 | Pathologically confirmed | Personal interviews | Age, sex, region, hospital and year of diagnosis | 4 |
| MDS | 399 | ||||||||||
| Wakabayashi | 1994 | Japan | 1981–1990 | Control | HB | 51.3±15.8 | 150 | Medical records | Medical records | Age, sex | 3 |
| ANLL | 75 | ||||||||||
| Mele | 1994 | Italy | 1986–1989 | Control | HB | ≥30 | 467 | Medical records | Personal interviews | Age, education, residence | 6 |
| AML | 118 | ||||||||||
| Sandler | 1993 | USA/Canada | 1986–1989 | Control | PB | 18–79 | 618 | Pathologically confirmed | Telephone interviews | Age, sex, race, region | 7 |
| AML | 423 | ||||||||||
| Brown | 1992 | USA | 1981–1984 | Control | PB | ≥30 | 745 | Medical records | Personal interviews | Age, region, vital status | 9 |
| ANLL | 134 | ||||||||||
| Brownson | 1991 | USA | 1984–1990 | Control | PB | ≥20 | 3641 | Pathologically confirmed | Medical records | Age | 7 |
| AML | 367 | ||||||||||
| Severson | 1990 | USA | 1984–1986 | Control | PB | 20–79 | 128 | Pathologically confirmed | Telephone interviews | Age, sex, family income | 5 |
| ANLL | 106 |
Abbreviations: No. of subjects, Number of subjects; MDS, Myelodysplastic Syndrome; AML, Acute Myeloid Leukemia; ANNL, Acute Nonlymphocytic Leukemia; NOS, Newcastle-Ottawa Scale; PB, Population-Based; HB, Hospital-Based; BMI, Body Mass Index.
Meta-analysis
Current smokers
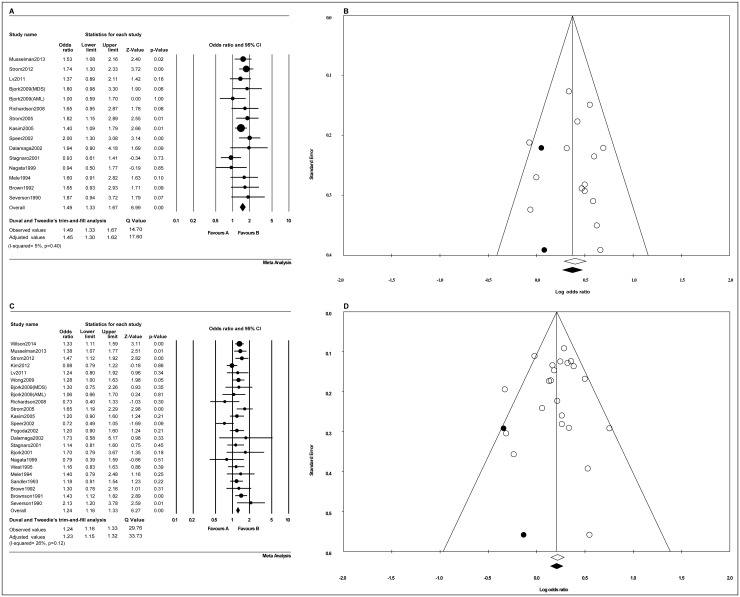
Thirteen [15, 16, 26, 28, 30, 35, 37–39, 41, 43, 45, 46] out of fourteen studies independently researched the relationship between MDS or AML and cigarette smoking, and one [17] study meanwhile researched MDS and AML. The pooled OR was 1.45 (95% CI, 1.30–1.62; p<0.001), and it was determined that current smokers had a 45% higher risk of developing adult myeloid disease compared with non-smokers, with low heterogeneity (Fig 2A). A funnel plot identified the presence of publication bias, and Duval and Tweedie’s trim-and-fill analysis was used to adjust the ORs (Fig 2B), with p = 0.46 in the Begg rank correction test and p = 0.89 in Egger’s linear regression test.
Fig 2. The odds ratio estimates of the risk of developing adult myeloid disease in smokers.
(A) A forest plot of the risk of developing adult myeloid disease in current smokers. (B) Duval and Tweedie’s trim-and-fill funnel plots were used to observe and adjust the publication bias in current smokers. (C) A forest plot of the risk of developing adult myeloid disease in ever-smokers. (D) Duval and Tweedie’s trim-and-fill funnel plots were used to observe and adjust the publication bias in ever-smokers. Among Fig B and D, The white circles represent observed studies, and black circles represent possibly missed studies imputed using Duval and Tweedie’s trim-and-fill method. White and black rhombuses represent observed and theoretical combined effect size, respectively.
Ever-smokers
Twenty-one [15, 16, 18, 26–30, 32, 33, 35–39, 41–46] out of twenty-two studies independently researched the relationship between MDS or AML and cigarette smoking, and one study [17] meanwhile researched MDS and AML. The pooled OR was 1.23 (95% CI, 1.15–1.32; p<0.001), which confirmed that ever-smokers had a 23% increased risk of developing adult myeloid disease compared with non-smokers, with moderate heterogeneity (Fig 2C). A funnel plot identified the presence of publication bias, so Duval and Tweedie’s trim-and-fill analysis was used to adjust the ORs (Fig 2D), with p = 0.75 in the Begg rank correction test and p = 0.83 in Egger’s linear regression test.
A sensitivity analysis was conducted, and the pooled OR was not significantly changed in the current smokers (S1 Fig) or ever-smokers (S2 Fig) when individual studies were removed in each turn.
Subgroup analysis
We performed subgroup analyses stratified by the forms of disease, geographical region, NOS score (high and medium quality studies) and the source of controls in this study (Table 2).
Table 2. The results of subgroup analyses performed according to the potential sources of heterogeneity.
| Outcome | Form of disease | Geographical region | NOS score | Source of control | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| AML | MDS | Asia | Europe | Nor A | High | Medium | PB | HB | PB&HB | |
| Current smokers | ||||||||||
| No. of datasets | 10 | 5 | 2 | 6 | 7 | 11 | 4 | 8 | 5 | 2 |
| OR (95% CI) | 1.49 (1.31–1.69) | 1.52 (1.19–1.94) | 1.22 (0.85–1.74) | 1.31 (1.05–1.63) | 1.62 (1.41–1.86) | 1.47 (1.30–1.66) | 1.62 (1.23–2.14) | 1.44 (1.26–1.65) | 1.71 (1.37–2.13) | 1.32 (0.74–2.34) |
| P value | <0.001 | 0.001 | 0.29 | 0.02 | <0.001 | <0.001 | 0.001 | <0.001 | <0.001 | 0.35 |
| I 2 | 18% | 0% | 0% | 27% | 0% | 4% | 23% | 20% | 0% | 51% |
| Pub. bias | YES | YES | CBC | YES | YES | YES | NO | YES | NO | CBC |
| AOR (95% CI) | 1.43 (1.27–1.61) | 1.48 (1.17–1.86) | 1.09 (0.90–1.31) | 1.54 (1.36–1.75) | 1.43 (1.27–1.61) | 1.43 (1.25–1.63) | ||||
| Ever-smokers | ||||||||||
| No. of datasets | 16 | 7 | 4 | 9 | 10 | 15 | 8 | 13 | 8 | 2 |
| OR (95% CI) | 1.21 (1.12–1.31) | 1.32 (1.16–1.50) | 1.10 (0.95–1.28) | 1.24 (1.10–1.40) | 1.31 (1.19–1.44) | 1.29 (1.19–1.41) | 1.16 (0.94–1.43) | 1.30 (1.19–1.41) | 1.17 (0.97–1.41) | 1.16 (0.81–1.66) |
| P value | <0.001 | <0.001 | 0.21 | <0.001 | <0.001 | <0.001 | 0.01 | <0.001 | 0.10 | 0.429 |
| I 2 | 37% | 0% | 19% | 0% | 47% | 0% | 60% | 2% | 51% | 0% |
| Pub. bias | YES | NO | NO | NO | YES | NO | YES | NO | YES | CBC |
| AOR (95% CI) | 1.20 (1.11–1.30) | 1.29 (1.17–1.42) | 1.13 (1.01–1.26) | 1.06 (0.88–1.28) | ||||||
Abbreviations: No. of datasets, Number of datasets (papers); MDS, Myelodysplastic Syndrome; AML, Acute Myeloid Leukemia; Nor A, North America; NOS, Newcastle-Ottawa Scale; Pub. bias, Publication bias; CBC, cannot be calculated; OR, odds ratio; AOR, Adjusted OR; CI, Confidence interval; PB, Population-based; HB, Hospital-based.
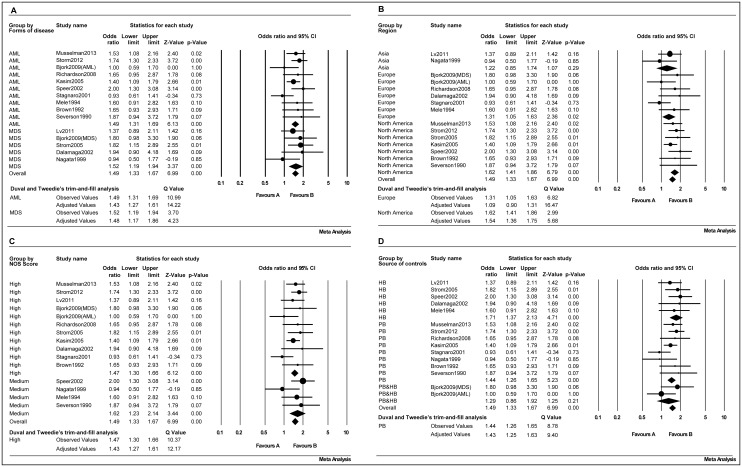
Current smokers
Group stratified by the form of disease showed a pooled OR of 1.43 (95% CI, 1.27–1.61; p<0.001) for AML and 1.48 (95% CI, 1.17–1.86; p = 0.001) for MDS (Fig 3A). When the subjects were grouped by region, the data showed that the pooled OR was 1.22 (95% CI, 0.85–1.74; p = 0.29) for Asia, 1.09 (95% CI, 0.90–1.31; p = 0.02) for Europe and was 1.54 (95% CI, 1.36–1.75; p<0.001) for North America (Fig 3B). In the data grouped by the NOS score, it was shown that the pooled OR was 1.43 (95% CI, 1.27–1.61; p<0.001) for high quality studies and was 1.62 (95% CI, 1.23–2.14; p = 0.001) for medium quality studies (Fig 3C). When the data were grouped based on the source of controls, the pooled OR was 1.43 (95% CI, 1.25–1.63; p<0.001) for population-based controls and was 1.71 (95% CI, 1.37–2.13; p<0.001) for hospital-based controls (Fig 3D).
Fig 3. Forest plots of the risk of adult myeloid disease in current smokers.
(A) Forms of disease, (B) geographical region, (C) NOS score (high and medium quality), (D) source of controls.
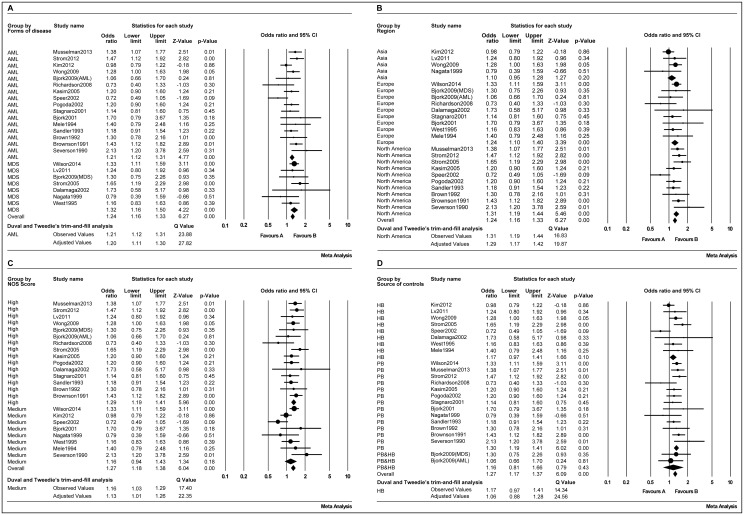
Ever-smokers
The subjects were also grouped based on the form of disease, geographical region, NOS score and source of control, all results indicated an significant increased OR, but a little less than current smokers. The results were shown in Table 2 and Fig 4.
Fig 4. Forest plots of the risk of adult myeloid disease in ever-smokers.
(A) Forms of disease, (B) geographical region, (C) NOS score (high and medium quality), (D) source of controls.
Smoking status analysis
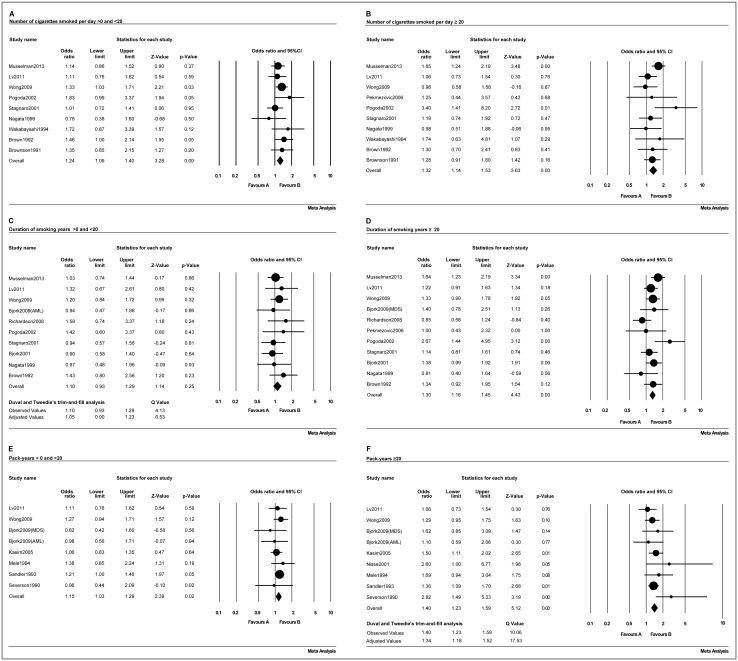
Cigarette smoking does not exert its carcinogenic effects via a single event, but is instead a cumulative process. To further investigate the relationship between cigarette smoking and adult myeloid disease, three aspects were analyzed: the number of cigarettes smoked per day, the number of years of smoking and the pack-years smoked. The outcomes are shown in Table 3. Patients who smoked < 20 (Fig 5A) and ≥20 (Fig 5B) cigarettes per day had 1.24 (95% CI, 1.09–1.40; p = 0.001) and 1.32 (95% CI, 1.14–1.53; p<0.001) increased risks of developing adult myeloid disease, respectively. For patients with <20 (Fig 5C) and ≥20 (Fig 5D) years of smoking, the risk of adult myeloid disease was 1.05 (95% CI, 0.90–1.23; p = 0.25) and 1.30 (95% CI, 1.16–1.45; p<0.001), respectively. Similarly those with <20 (Fig 5E) and ≥20 (Fig 5F) pack-years had a risk of adult myeloid disease of 1.15 (95% CI, 1.03–1.29; p = 0.017) and 1.34 (95% CI, 1.18–1.52; p<0.001), respectively.
Table 3. Odds ratio estimates of the risk of adult myeloid disease according to the smoking status.
| Outcome | Cigarettes per day | Duration of smoking (years) | Pack-years | |||
|---|---|---|---|---|---|---|
| >0 and<20 | ≥20 | >0 and<20 | ≥20 | >0 and<20 | ≥20 | |
| No. of datasets | 9 | 10 | 10 | 11 | 8 | 9 |
| OR (95% CI) | 1.24(1.09–1.40) | 1.32(1.14–1.53) | 1.10(0.93–1.29) | 1.30(1.16–1.45) | 1.15(1.03–1.29) | 1.40(1.23–1.59) |
| p Value | 0.001 | <0.001 | 0.25 | <0.001 | 0.017 | <0.001 |
| I 2 | 0% | 18% | 0% | 36% | 0% | 20% |
| Pub. bias | NO | NO | YES | NO | NO | YES |
| AOR | 1.05(0.90–1.23) | 1.34(1.18–1.52) | ||||
Abbreviations: No. of datasets, number of datasets; OR, Odds ratio; AOR, Adjusted OR; CI, Confidence interval; Pub. bias, Publication bias.
Fig 5. Forest plots of the association of adult myeloid disease with the smoking status based on cigarettes smoked per day (A-B), the duration of smoking (in years) (C-D), and the pack-years smoked (E-F).
Discussion
Recently, Fircanis [19] and Tong [20] analyzed association of smoking with AML and MDS by meta-analysis, respectively. Since approximately one-third of MDS cases could progress to AML, we supposed that the inclusion of some transformational cases (where the phenotype was AML but where the disease had developed from MDS) could have induced serious bias in independent analyses. Therefore, we conducted this meta-analysis that combined MDS with AML together as a single class of “adult myeloid disease” to eliminate bias.
To our knowledge, this study is the first meta-analysis that combined MDS with AML to assess the overall risk of adult myeloid disease due to cigarette smoking. We extracted twenty-five studies that included 8,074 cases and 31,805 controls, and demonstrated a statistically significant association between current smoking and an increased incidence of adult myeloid disease. Current smokers were shown to have a 45% higher risk of developing adult myeloid disease than non-smokers. Ever-smokers had a 23% higher risk of developing adult myeloid disease than non-smokers, indicating that current smokers had a higher risk of adult myeloid disease than ever-smokers. One possible reason was that current smokers might have a higher total cumulative dose such as nicotine, benzene and polycyclic aromatic hydrocarbon, and longer exposure time of smoking than ever smokers.
In addition, we found that the risk of myeloid disease had no significant drops after cessationin ever-smokers. As we known, tobacco is one of the most potent carcinogenic mixtures and the carcinogenic effect of cigarette smoking can persist for decades after smoking cessation. Few studies have reported on the dynamics and mechanism following cessation. Most recent two [47, 48] studies showed that DNA methylation levels in ever-smokers approached those of never smokers several years after smoking cessation. Therefore, the DNA methylation maybe one factor that the risk of myeloid disease had no significant drops after cessationin ever-smokers. The truly irreversible nature of smoking-related and associated biomarkers are needed to be investigated.
According to the sub-analysis of the smoking status, there was a dose-relationship between cigarette smoking and adult myeloid disease. First, the risk of adult myeloid disease increased from 24% to 32% when smokers smoked <20 vs.≥ 20 cigarettes per day. Second, the risk of adult myeloid disease increased from 5% to 30% in smokers who smoked <20 years compared with those who smoked ≥20 years. Finally, the risk of adult myeloid disease increased from 15% to 34% when the comparison was made of smokers who had smoked <20 vs.≥ 20 pack-years. Based on these results, we confirmed that there were close, positive, and cumulative effects of smoking on the development of adult myeloid disease. Moreover, we also found that cigarette smoking in North America was associated with a higher ORs than in Europe and Asia, but limited studies were inadequate for a clear conclusion that people who live in North America were susceptible population.
Now that cigarette smoking had a high risk to induce adult myeloid disease, Does it play a key role in MDS transformation? There have as yet been few detailed studies on the MDS transformation into AML by the individuals’ smoking habits, however, indirect studies may provide us related clues. Over the years, a large number of studies have been presented that indicate a causal link between MDS development and genetic abnormality, related genes liked bcl-2 [49], C-CBL [50], CD95 [51], HOXA9 [52], TNFα [53]. In addition, CpG methylation [54, 55], telomere shortening [56, 57] and microsatellite instability [58–60] also were found association with MDS progression to AML. Most importantly all above mentioned factors were affected by cigarette smoking [61–70]. Based on these studies, it indirectly indicated that cigarette smoking may be an induced factor on MDS development.
Benzene of smoking is a known clastogen, causing chromosomal aberrations in vitro, and prolonged exposure to mean concentrations of >64 mg/m3 may be associated with chromosomal aberrations. In addition, increased risks of developing all types of leukemias were found at all concentrations of exposure, while exposure to levels above 40 ppm increased the risk of acute nonlymphocytic leukemia [71]. Zhang [72] conducted a chromosome-wide aneuploidy study (CWAS) in workers exposed to benzene, and their findings suggested that the development of aneuploidy may be a potential mechanism underlying benzene-induced leukemia. Benzene is mainly found in the atmosphere, and almost all human exposure is through inhalation (95% of daily intake) [71]. Personal exposure assessment research has indicated that an average cigarette smoker inhales 6–10 times the benzene inhaled by average non-smokers, and approximately 90% of a smoker’s benzene exposure is from smoking [73]. Consequently, the tobacco use may lead to chromosomal and karyotype aberrations due to increased benzene exposure, thus resulting in MDS or AML.
Our study is associated with some limitations that may have affected the results. First, the results were calculated from published studies, and our included studies cannot cover published studies that could have led to a publication bias. In addition, published studies are often positive, and the omission of unpublished studies (with negative findings) may lead to an overestimation of the pooled OR. Second, the methods used to evaluate the smoking habits were mainly questionnaires or reports, rather than based on determinations of the blood levels of cotinine. Third, some of the subset analyses, although specified a priori, were performed on small datasets. Finally, methodological differences and confounding factors in the included studies were unavoidable.
Conclusion
In summary, we herein demonstrated that cigarette smoking leads to a significantly increased risk of adult myeloid disease in adults. Cigarette smoking does not act as a carcinogenic factor via a single exposure, and instead leads to a cumulative process. We found that there was a positive risk between smoking and adult myeloid disease when a threshold smoking dose was crossed. More and larger prospective studies should be performed, and future studies should focus on investigating the pathway(s) by which cigarette smoking can induce adult myeloid disease.
Supporting Information
(TIF)
(TIF)
(DOC)
Acknowledgments
We sincerely thank Zhuoying Zoulin, Yinghan Jiang, Xiujuan Liu and Guiyun Li, for their help in polishing our paper.
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
The authors have no support or funding to report.
References
- 1.Surveillance E, and End Results. Surveillance, Epidemiology, and End Results (SEER) Sheets: Age Adjusted and US Death Rates and 5 year relative survival by Primary cancer site, sex and age. [Internet]. 2013 [cited October 23]. Available from: http://seer.cancer.gov/csr/1975_2010/results_single/sect_01_table.05_2pgs.pdf.
- 2. Ades L, Itzykson R, Fenaux P. Myelodysplastic syndromes. Lancet. 2014;383(9936):2239–52. 10.1016/S0140-6736(13)61901-7 . [DOI] [PubMed] [Google Scholar]
- 3.National Comprehensive Cancer Network (NCCN) Clinical Practice Guidelines in Oncology: Acute Myeloid Leukemia (Version 1.2015) [Internet]. 2014 [cited December 3]. Available from: http://www.nccn.org/professionals/physician_gls/pdf/aml.pdf.
- 4. Liu YQ Z F, Chen WQ. An analysis of incidence and mortality of leukemia in China, 2009. China Cancer. 2013;22(7):528–34. [Google Scholar]
- 5. Ma X, Does M, Raza A, Mayne ST. Myelodysplastic syndromes: incidence and survival in the United States. Cancer. 2007;109(8):1536–42. . [DOI] [PubMed] [Google Scholar]
- 6. Aul C, Bowen DT, Yoshida Y. Pathogenesis, etiology and epidemiology of myelodysplastic syndromes. Haematologica. 1998;83(1):71–86. . [PubMed] [Google Scholar]
- 7. Hofmann WK, Koeffler HP. Myelodysplastic syndrome. Annual review of medicine. 2005;56:1–16. 10.1146/annurev.med.56.082103.104704 . [DOI] [PubMed] [Google Scholar]
- 8. Corey SJ, Minden MD, Barber DL, Kantarjian H, Wang JC, Schimmer AD. Myelodysplastic syndromes: the complexity of stem-cell diseases. Nature reviews Cancer. 2007;7(2):118–29. . [DOI] [PubMed] [Google Scholar]
- 9. Ozcan MA, Ilhan O, Ozcebe OI, Nalcaci M, Gulbas Z. Review of therapeutic options and the management of patients with myelodysplastic syndromes. Expert review of hematology. 2013;6(2):165–89. 10.1586/ehm.13.7 . [DOI] [PubMed] [Google Scholar]
- 10. Fenaux P, Haase D, Sanz GF, Santini V, Buske C, Group EGW. Myelodysplastic syndromes: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Annals of oncology: official journal of the European Society for Medical Oncology / ESMO. 2014;25 Suppl 3:iii57–69. 10.1093/annonc/mdu180 . [DOI] [PubMed] [Google Scholar]
- 11.Fact sheets of Tobacco from the World Health Organization Accessed on: update May 2014. Available from: http://www.who.int/mediacentre/factsheets/fs339/en/.
- 12. Humans IWGotEoCRt. Tobacco smoke and involuntary smoking. IARC monographs on the evaluation of carcinogenic risks to humans / World Health Organization, International Agency for Research on Cancer. 2004;83:1–1438. . [PMC free article] [PubMed] [Google Scholar]
- 13. McLaughlin JK, Hrubec Z, Linet MS, Heineman EF, Blot WJ, Fraumeni JF Jr. Cigarette smoking and leukemia. Journal of the National Cancer Institute. 1989;81(16):1262–3. . [DOI] [PubMed] [Google Scholar]
- 14. Paffenbarger RS Jr., Brand RJ, Sholtz RI, Jung DL. Energy expenditure, cigarette smoking, and blood pressure level as related to death from specific diseases. American journal of epidemiology. 1978;108(1):12–8. . [PubMed] [Google Scholar]
- 15. Nagata C, Shimizu H, Hirashima K, Kakishita E, Fujimura K, Niho Y, et al. Hair dye use and occupational exposure to organic solvents as risk factors for myelodysplastic syndrome. Leukemia research. 1999;23(1):57–62. . [DOI] [PubMed] [Google Scholar]
- 16. Stagnaro E, Ramazzotti V, Crosignani P, Fontana A, Masala G, Miligi L, et al. Smoking and hematolymphopoietic malignancies. Cancer causes & control: CCC. 2001;12(4):325–34. . [DOI] [PubMed] [Google Scholar]
- 17. Bjork J, Johansson B, Broberg K, Albin M. Smoking as a risk factor for myelodysplastic syndromes and acute myeloid leukemia and its relation to cytogenetic findings: a case-control study. Leukemia research. 2009;33(6):788–91. 10.1016/j.leukres.2008.10.009 . [DOI] [PubMed] [Google Scholar]
- 18. Wilson AB, Neogi T, Prout M, Jick S. Relative risk of myelodysplastic syndromes in patients with autoimmune disorders in the General Practice Research Database. Cancer epidemiology. 2014;38(5):544–9. 10.1016/j.canep.2014.08.003 . [DOI] [PubMed] [Google Scholar]
- 19. Fircanis S, Merriam P, Khan N, Castillo JJ. The relation between cigarette smoking and risk of acute myeloid leukemia: an updated meta-analysis of epidemiological studies. American journal of hematology. 2014;89(8):E125–32. 10.1002/ajh.23744 . [DOI] [PubMed] [Google Scholar]
- 20. Tong H, Hu C, Yin X, Yu M, Yang J, Jin J. A Meta-Analysis of the Relationship between Cigarette Smoking and Incidence of Myelodysplastic Syndromes. PloS one. 2013;8(6):e67537 10.1371/journal.pone.0067537 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Swerdlow SH, Campo E., Harris N.L., Jaffe E.S., Pileri S.A., Stein H., Thiele J., Vardiman J.W. WHO Classification of Tumours of Haematopoietic and Lymphoid Tissues, Fourth Edition: IARC; 2008. 439 p. [Google Scholar]
- 22.The Newcastle-Ottawa Scale (NOS) for assessing the quality of non-randomised studies in meta-analyses Accessed on: January 1, 2014. Available from: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp.
- 23. Bowden J, Tierney JF, Copas AJ, Burdett S. Quantifying, displaying and accounting for heterogeneity in the meta-analysis of RCTs using standard and generalised Q statistics. BMC medical research methodology. 2011;11:41 10.1186/1471-2288-11-41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. Bmj. 1997;315(7109):629–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Duval S, Tweedie R. Trim and fill: A simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics. 2000;56(2):455–63. . [DOI] [PubMed] [Google Scholar]
- 26. Severson RK, Davis S, Heuser L, Daling JR, Thomas DB. Cigarette smoking and acute nonlymphocytic leukemia. American journal of epidemiology. 1990;132(3):418–22. . [DOI] [PubMed] [Google Scholar]
- 27. Brownson RC, Chang JC, Davis JR. Cigarette smoking and risk of adult leukemia. American journal of epidemiology. 1991;134(9):938–41. . [DOI] [PubMed] [Google Scholar]
- 28. Brown LM, Gibson R, Blair A, Burmeister LF, Schuman LM, Cantor KP, et al. Smoking and risk of leukemia. American journal of epidemiology. 1992;135(7):763–8. . [DOI] [PubMed] [Google Scholar]
- 29. Sandler DP, Shore DL, Anderson JR, Davey FR, Arthur D, Mayer RJ, et al. Cigarette smoking and risk of acute leukemia: associations with morphology and cytogenetic abnormalities in bone marrow. Journal of the National Cancer Institute. 1993;85(24):1994–2003. . [DOI] [PubMed] [Google Scholar]
- 30. Mele A, Szklo M, Visani G, Stazi MA, Castelli G, Pasquini P, et al. Hair dye use and other risk factors for leukemia and pre-leukemia: a case-control study. Italian Leukemia Study Group. American journal of epidemiology. 1994;139(6):609–19. . [DOI] [PubMed] [Google Scholar]
- 31. Wakabayashi I, Sakamoto K, Masui H, Yoshimoto S, Kanamaru A, Kakishita E, et al. A case-control study on risk factors for leukemia in a district of Japan. Internal medicine. 1994;33(4):198–203. . [DOI] [PubMed] [Google Scholar]
- 32. West RR, Stafford DA, Farrow A, Jacobs A. Occupational and environmental exposures and myelodysplasia: a case-control study. Leukemia research. 1995;19(2):127–39. . [DOI] [PubMed] [Google Scholar]
- 33. Bjork J, Albin M, Mauritzson N, Stromberg U, Johansson B, Hagmar L. Smoking and acute myeloid leukemia: associations with morphology and karyotypic patterns and evaluation of dose-response relations. Leukemia research. 2001;25(10):865–72. . [DOI] [PubMed] [Google Scholar]
- 34. Nisse C, Haguenoer JM, Grandbastien B, Preudhomme C, Fontaine B, Brillet JM, et al. Occupational and environmental risk factors of the myelodysplastic syndromes in the North of France. British journal of haematology. 2001;112(4):927–35. . [DOI] [PubMed] [Google Scholar]
- 35. Dalamaga M, Petridou E, Cook FE, Trichopoulos D. Risk factors for myelodysplastic syndromes: a case-control study in Greece. Cancer causes & control: CCC. 2002;13(7):603–8. . [DOI] [PubMed] [Google Scholar]
- 36. Pogoda JM, Preston-Martin S, Nichols PW, Ross RK. Smoking and risk of acute myeloid leukemia: results from a Los Angeles County case-control study. American journal of epidemiology. 2002;155(6):546–53. . [DOI] [PubMed] [Google Scholar]
- 37. Speer SA, Semenza JC, Kurosaki T, Anton-Culver H. Risk factors for acute myeloid leukemia and multiple myeloma: a combination of GIS and case-control studies. Journal of environmental health. 2002;64(7):9–16; quiz 35–6. . [PubMed] [Google Scholar]
- 38. Kasim K, Levallois P, Abdous B, Auger P, Johnson KC. Lifestyle factors and the risk of adult leukemia in Canada. Cancer causes & control: CCC. 2005;16(5):489–500. 10.1007/s10552-004-7115-1 . [DOI] [PubMed] [Google Scholar]
- 39. Strom SS, Gu Y, Gruschkus SK, Pierce SA, Estey EH. Risk factors of myelodysplastic syndromes: a case-control study. Leukemia. 2005;19(11):1912–8. 10.1038/sj.leu.2403945 . [DOI] [PubMed] [Google Scholar]
- 40. Pekmezovic T, Suvajdzic Vukovic N, Kisic D, Grgurevic A, Bogdanovic A, Gotic M, et al. A case-control study of myelodysplastic syndromes in Belgrade (Serbia Montenegro). Annals of hematology. 2006;85(8):514–9. . [DOI] [PubMed] [Google Scholar]
- 41. Richardson DB, Terschuren C, Pohlabeln H, Jockel KH, Hoffmann W. Temporal patterns of association between cigarette smoking and leukemia risk. Cancer causes & control: CCC. 2008;19(1):43–50. 10.1007/s10552-007-9068-7 . [DOI] [PubMed] [Google Scholar]
- 42. Wong O, Harris F, Yiying W, Hua F. A hospital-based case-control study of acute myeloid leukemia in Shanghai: analysis of personal characteristics, lifestyle and environmental risk factors by subtypes of the WHO classification. Regulatory toxicology and pharmacology: RTP. 2009;55(3):340–52. 10.1016/j.yrtph.2009.08.007 . [DOI] [PubMed] [Google Scholar]
- 43. Lv L, Lin G, Gao X, Wu C, Dai J, Yang Y, et al. Case-control study of risk factors of myelodysplastic syndromes according to World Health Organization classification in a Chinese population. American journal of hematology. 2011;86(2):163–9. 10.1002/ajh.21941 . [DOI] [PubMed] [Google Scholar]
- 44. Kim HN, Kim NY, Yu L, Tran HT, Kim YK, Lee IK, et al. Association of GSTT1 polymorphism with acute myeloid leukemia risk is dependent on smoking status. Leukemia & lymphoma. 2012;53(4):681–7. 10.3109/10428194.2011.625576 . [DOI] [PubMed] [Google Scholar]
- 45. Strom SS, Oum R, Elhor Gbito KY, Garcia-Manero G, Yamamura Y. De novo acute myeloid leukemia risk factors: a Texas case-control study. Cancer. 2012;118(18):4589–96. 10.1002/cncr.27442 . [DOI] [PubMed] [Google Scholar]
- 46. Musselman JR, Blair CK, Cerhan JR, Nguyen P, Hirsch B, Ross JA. Risk of adult acute and chronic myeloid leukemia with cigarette smoking and cessation. Cancer epidemiology. 2013;37(4):410–6. 10.1016/j.canep.2013.03.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Guida F, Sandanger TM, Castagne R, Campanella G, Polidoro S, Palli D, et al. Dynamics of smoking-induced genome-wide methylation changes with time since smoking cessation. Human molecular genetics. 2015;24(8):2349–59. 10.1093/hmg/ddu751 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Zeilinger S, Kuhnel B, Klopp N, Baurecht H, Kleinschmidt A, Gieger C, et al. Tobacco smoking leads to extensive genome-wide changes in DNA methylation. PloS one. 2013;8(5):e63812 10.1371/journal.pone.0063812 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Davis RE, Greenberg PL. Bcl-2 expression by myeloid precursors in myelodysplastic syndromes: relation to disease progression. Leukemia research. 1998;22(9):767–77. . [DOI] [PubMed] [Google Scholar]
- 50. Kao HW, Sanada M, Liang DC, Lai CL, Lee EH, Kuo MC, et al. A high occurrence of acquisition and/or expansion of C-CBL mutant clones in the progression of high-risk myelodysplastic syndrome to acute myeloid leukemia. Neoplasia. 2011;13(11):1035–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Ettou S, Audureau E, Humbrecht C, Benet B, Jammes H, Clozel T, et al. Fas expression at diagnosis as a biomarker of azacitidine activity in high-risk MDS and secondary AML. Leukemia. 2012;26(10):2297–9. 10.1038/leu.2012.152 . [DOI] [PubMed] [Google Scholar]
- 52. Heinrichs S, Berman JN, Ortiz TM, Kornblau SM, Neuberg DS, Estey EH, et al. CD34+ cell selection is required to assess HOXA9 expression levels in patients with myelodysplastic syndrome. British journal of haematology. 2005;130(1):83–6. . [DOI] [PubMed] [Google Scholar]
- 53. Stifter G, Heiss S, Gastl G, Tzankov A, Stauder R. Over-expression of tumor necrosis factor-alpha in bone marrow biopsies from patients with myelodysplastic syndromes: relationship to anemia and prognosis. European journal of haematology. 2005;75(6):485–91. 10.1111/j.1600-0609.2005.00551.x . [DOI] [PubMed] [Google Scholar]
- 54. Benetatos L, Hatzimichael E, Dasoula A, Dranitsaris G, Tsiara S, Syrrou M, et al. CpG methylation analysis of the MEG3 and SNRPN imprinted genes in acute myeloid leukemia and myelodysplastic syndromes. Leukemia research. 2010;34(2):148–53. 10.1016/j.leukres.2009.06.019 . [DOI] [PubMed] [Google Scholar]
- 55. Jiang Y, Dunbar A, Gondek LP, Mohan S, Rataul M, O'Keefe C, et al. Aberrant DNA methylation is a dominant mechanism in MDS progression to AML. Blood. 2009;113(6):1315–25. 10.1182/blood-2008-06-163246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Poloni A, Serrani F, Berardinelli E, Maurizi G, Mariani M, Costantini B, et al. Telomere length, c-myc and mad-1 expression could represent prognosis markers of myelodysplastic syndrome. Leukemia research. 2013;37(11):1538–44. 10.1016/j.leukres.2013.07.022 . [DOI] [PubMed] [Google Scholar]
- 57. Ohyashiki K, Iwama H, Yahata N, Tauchi T, Kawakubo K, Shimamoto T, et al. Telomere dynamics in myelodysplastic syndromes and acute leukemic transformation. Leukemia & lymphoma. 2001;42(3):291–9. 10.3109/10428190109064585 . [DOI] [PubMed] [Google Scholar]
- 58. Sheikhha MH, Tobal K, Liu Yin JA. High level of microsatellite instability but not hypermethylation of mismatch repair genes in therapy-related and secondary acute myeloid leukaemia and myelodysplastic syndrome. British journal of haematology. 2002;117(2):359–65. . [DOI] [PubMed] [Google Scholar]
- 59. Mori N, Morosetti R, Hoflehner E, Lubbert M, Mizoguchi H, Koeffler HP. Allelic loss in the progression of myelodysplastic syndrome. Cancer research. 2000;60(11):3039–42. . [PubMed] [Google Scholar]
- 60. Tasak T, Lee S, Spira S, Takeuchi S, Hatta Y, Nagai M, et al. Infrequent microsatellite instability during the evolution of myelodysplastic syndrome to acute myelocytic leukemia. Leukemia research. 1996;20(2):113–7. . [DOI] [PubMed] [Google Scholar]
- 61. Bell DA, Liu Y, Cortopassi GA. Occurrence of bcl-2 oncogene translocation with increased frequency in the peripheral blood of heavy smokers. Journal of the National Cancer Institute. 1995;87(3):223–4. . [DOI] [PubMed] [Google Scholar]
- 62. Kim DH, Nelson HH, Wiencke JK, Zheng S, Christiani DC, Wain JC, et al. p16(INK4a) and histology-specific methylation of CpG islands by exposure to tobacco smoke in non-small cell lung cancer. Cancer research. 2001;61(8):3419–24. . [PubMed] [Google Scholar]
- 63. Wang HY, Shin VY, Leung SY, Yuen ST, Cho CH. Involvement of bcl-2 and caspase-3 in apoptosis induced by cigarette smoke extract in the gastric epithelial cell. Toxicologic pathology. 2003;31(2):220–6. . [DOI] [PubMed] [Google Scholar]
- 64. Chia VM, Newcomb PA, Bigler J, Morimoto LM, Thibodeau SN, Potter JD. Risk of microsatellite-unstable colorectal cancer is associated jointly with smoking and nonsteroidal anti-inflammatory drug use. Cancer research. 2006;66(13):6877–83. 10.1158/0008-5472.CAN-06-1535 . [DOI] [PubMed] [Google Scholar]
- 65. Samowitz WS, Albertsen H, Sweeney C, Herrick J, Caan BJ, Anderson KE, et al. Association of smoking, CpG island methylator phenotype, and V600E BRAF mutations in colon cancer. Journal of the National Cancer Institute. 2006;98(23):1731–8. 10.1093/jnci/djj468 . [DOI] [PubMed] [Google Scholar]
- 66. Jenny N. Poynter RW. Associations between smoking, alcohol consumption and colorectal cancer, overall and by tumor microsatellite instability status. Cancer Epidemiol Biomarkers Prev. 2009;18(10):2745–50. 10.1158/1055-9965.EPI-09-0517 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Oka D, Yamashita S, Tomioka T, Nakanishi Y, Kato H, Kaminishi M, et al. The presence of aberrant DNA methylation in noncancerous esophageal mucosae in association with smoking history: a target for risk diagnosis and prevention of esophageal cancers. Cancer. 2009;115(15):3412–26. 10.1002/cncr.24394 . [DOI] [PubMed] [Google Scholar]
- 68. Sarir H, Mortaz E, Janse WT, Givi ME, Nijkamp FP, Folkerts G. IL-8 production by macrophages is synergistically enhanced when cigarette smoke is combined with TNF-alpha. Biochemical pharmacology. 2010;79(5):698–705. 10.1016/j.bcp.2009.10.001 . [DOI] [PubMed] [Google Scholar]
- 69. Huang J, Okuka M, Lu W, Tsibris JC, McLean MP, Keefe DL, et al. Telomere shortening and DNA damage of embryonic stem cells induced by cigarette smoke. Reproductive toxicology. 2013;35:89–95. 10.1016/j.reprotox.2012.07.003 . [DOI] [PubMed] [Google Scholar]
- 70. Verde Z, Reinoso-Barbero L, Chicharro L, Garatachea N, Resano P, Sanchez-Hernandez I, et al. Effects of cigarette smoking and nicotine metabolite ratio on leukocyte telomere length. Environmental research. 2015;140:488–94. 10.1016/j.envres.2015.05.008 . [DOI] [PubMed] [Google Scholar]
- 71. Duarte-Davidson R, Courage C, Rushton L, Levy L. Benzene in the environment: an assessment of the potential risks to the health of the population. Occupational and environmental medicine. 2001;58(1):2–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Zhang L, Lan Q, Guo W, Hubbard AE, Li G, Rappaport SM, et al. Chromosome-wide aneuploidy study (CWAS) in workers exposed to an established leukemogen, benzene. Carcinogenesis. 2011;32(4):605–12. 10.1093/carcin/bgq286 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Lichtman MA. Cigarette smoking, cytogenetic abnormalities, and acute myelogenous leukemia. Leukemia. 2007;21(6):1137–40. 10.1038/sj.leu.2404698 . [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(TIF)
(TIF)
(DOC)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.