Percutaneous coronary intervention of Chronic Total Occlusions (CTOs) represents the most technically challenging procedure in contemporary Interventional Cardiology.1,2 Although large definitive randomized trials are lacking, a growing body of evidence suggests that successful percutaneous CTO revascularization relieves symptoms, improves left ventricular systolic function, reduces the need for surgical coronary bypass, and in the context of complete coronary revascularization improves survival.3-5 Yet, compared to patients with severely stenotic, but patent vessels, patients with a CTO are more likely to be referred for coronary bypass surgery or medical therapy, and in a recently published Canadian registry only one in ten patients with a CTO underwent PCI.6 Historically the success rate of CTO PCI was in the range of 70%6-8. This uncertainty regarding the likelihood of success, mixed with the fear of unacceptably high complication rates and prohibitive procedural costs, contribute to the reluctance to percutaneously revascularize CTOs.
The J-CTO Score (Japanese Multicenter CTO Registry)9 was originally developed to predict the likelihood of successful guidewire crossing within 30 minutes. Independent angiographic predictors of failure (each given one point) that made up the J-CTO score included prior failed attempt, angiographic evidence of heavy calcification, bending within the occluded segment, blunt proximal stump, and occlusion length >=20 mm.9 CTOs were then graded as easy, intermediate, difficult and very difficult (JCTO Scores of 0, 1, 2 and ≥3 respectively). Since then the J-CTO score has been found to predict the overall likelihood of CTO PCI success. High J-CTO scores have been shown to correlate with lesions complexity,10 and may account for the paradox of stagnant CTO PCI success rate over time, which was due to intervening on increasingly complex CTOs.11
In this issue of the journal, Opolski et al use coronary computed tomography angiography (CCTA) to improve on the J-CTO score. They report on a CCTA -derived scoring system in a cohort of 240 CTO PCI lesions from 4 European centers. They assigned 1 point for each independent predictor of successful guidewire crossing within 30 minutes. The points are then summed to yield the CT-RECTOR Score. CTO lesions were categorized as easy (score 0), intermediate (score 1), difficult (score 2), and very difficult (score >=3). In this study, independent predictors of failure derived from CCTA analysis included occlusion length >=20 mm, multiple occlusions, blunt stump, bending, and severe calcification in the CTO segment. Clinical predictors of failure included previously failed attempt at percutaneous revascularization and duration of CTO >= 12 month or unknown duration of occlusion. Using this score, the probability of successful guidewire crossing within 30 minutes for each group (from easy to very difficult) was 95%, 88%, 57%, and 22%, respectively. By combining CCTA and clinical characteristics the area under the receiver-operating curve for the CT-RECTOR score was greater than that of the J-CTO score (0.83 versus 0.71, p<0.001), suggesting superior discrimination between straightforward and complex CTO procedures.
There are several important considerations that are required before applying the CT-RECTOR score to contemporary CTO angioplasty, particularly if it will eventually be studied and evolve as a predictor of procedural success. With new technologies and techniques, success rates in expert centers consistently above 90% are possible with very acceptable complication rates.12,13 Of note in the U.S series,13 with adoption of the “Hybrid” approach,14 the use of CCTA is very limited. Therefore the decision to revascularize a CTO is a clinical one, based on symptoms, myocardial viability, and patient preference and should not be based on the ease or difficulty of the case. As such the CT-RECTOR score is useful by identifying highly complex cases that should be avoided by operators early in their CTO PCI learning curve and rather referred to expert centers.
The study cohort had modest success rate of only 62%, very low percentage of retrograde CTO PCI, and no cases of controlled antegrade dissection re-entry. In addition the percentage of prior CABG was 17% which is comparable to prior series from Europe12, Japan15 but significantly lower than US series,13 reflecting revascularization patterns that are different across the world. Patients with prior CABG represent a particularly challenging population because of extent of disease, calcification and distortion of anatomy (vessel tenting). Historically the success rate in prior CABG was lower than in non-CABG patients (78.1% versus 87.2%, p<0.001),16 and only recently the success rates became comparable between CABG and non-CABG patients (87.5% vs 92.5%, p=0.07).13,16 Therefore, the applicability of the CT-RECTOR score to U.S centers and operators that perform high end CTO PCI is unclear.
It is important to note that in the present study, dual injection coronary angiography was performed in only two thirds of cases. Consequently, the incremental value of CCTA, above angiographic scoring systems that systematically employ dual injection, may be exaggerated due to suboptimal baseline angiography without contralateral coronary injection. Single-catheter angiography provides inadequate information. Dual injection is crucial for determining the lesion length, the size and location of the distal target vessel, evaluating whether there is a significant bifurcation at the distal cap, the presence, size, and tortuosity of collateral vessels and for deciding on the optimal CTO PCI strategy.17 We recommend performing the dual injection angiogram at the time of the diagnostic procedure once a CTO is identified and strongly discourage ad hoc CTO PCI.18 This allows for a thorough pre-procedural planning. By implementing the “Hybrid Algorithm” the operator who is familiar with all available CTO PCI techniques (antegrade wire escalation, antegrade dissection and re-entry, and retrograde wire escalation and dissection reentry) can decide on the initial, as well all as the alternative strategies, in case the initial approach fails, that will provide the safest, most efficient, and most effective way to re-canalize the CTO in a single procedure (see figure 1). It should be noted that CCTA has some advantages over the angiogram: it is more sensitive than the angiogram at detecting tortuosity in the occluded segment and calcification that may impact the treatment strategy. Future research on CCTA should focus in identifying additional anatomical characteristics that could assist in formulating a CTO PCI strategy in the context of comprehensive CTO PCI algorithm.
Figure 1. Algorithm for Crossing Chronic Total Occlusions.
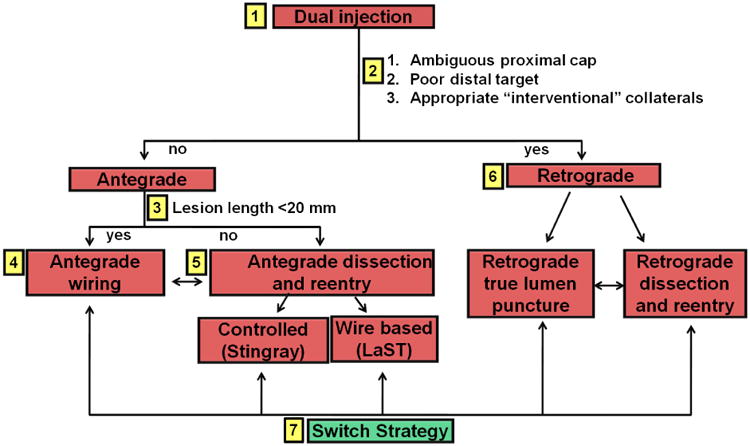
The algorithm starts with dual coronary injection (box 1) to allow assessment of several angiographic parameters (box 2) and allows selection of a primary antegrade (boxes 3 to 5) or primary retrograde (box 6) strategy. Strategy changes are made (box 7) depending on the progress of the case. LaST = limited antegrade subintimal tracking. Reproduced with permission from J Am Coll Cardiol Intv 2012;5:367–79 © 2012 by the American College of Cardiology Foundation.
In 2014 a new benchmark for CTO success rates of above 90% has been established. Anatomy dictates how and who should perform the CTO PCI, not whether the CTO PCI should be attempted. Similarly, lesion complexity no longer dictates the feasibility of CTO PCI, but the strategy for successful CTO revascularization.
Footnotes
Disclosures: Dr. Karmpaliotis: Honoraria Boston Scientific, Abbott Vascular, Medtronic, Asahi, Dr. Green: None
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Grantham JA, Marso SP, Spertus J, House J, Holmes DR, Jr, Rutherford BD. Chronic total occlusion angioplasty in the United States. JACC Cardiovasc Interv. 2009;2:479–86. doi: 10.1016/j.jcin.2009.02.008. [DOI] [PubMed] [Google Scholar]
- 2.Stone GW, Kandzari DE, Mehran R, et al. Percutaneous recanalization of chronically occluded coronary arteries: a consensus document: part I. Circulation. 2005;112:2364–72. doi: 10.1161/CIRCULATIONAHA.104.481283. [DOI] [PubMed] [Google Scholar]
- 3.Joyal D, Afilalo J, Rinfret S. Effectiveness of recanalization of chronic total occlusions: a systematic review and meta-analysis. Am Heart J. 2010;160:179–87. doi: 10.1016/j.ahj.2010.04.015. [DOI] [PubMed] [Google Scholar]
- 4.Mehran R, Claessen BE, Godino C, et al. Long-term outcome of percutaneous coronary intervention for chronic total occlusions. JACC Cardiovasc Interv. 2011;4:952–61. doi: 10.1016/j.jcin.2011.03.021. [DOI] [PubMed] [Google Scholar]
- 5.George S, Cockburn J, Clayton TC, et al. Long-term follow-up of elective chronic total coronary occlusion angioplasty: analysis from the u.k. Central cardiac audit database. J Am Coll Cardiol. 2014;64:235–43. doi: 10.1016/j.jacc.2014.04.040. [DOI] [PubMed] [Google Scholar]
- 6.Fefer P, Knudtson ML, Cheema AN, et al. Current perspectives on coronary chronic total occlusions: the Canadian Multicenter Chronic Total Occlusions Registry. J Am Coll Cardiol. 2012;59:991–7. doi: 10.1016/j.jacc.2011.12.007. [DOI] [PubMed] [Google Scholar]
- 7.Prasad A, Rihal CS, Lennon RJ, Wiste HJ, Singh M, Holmes DR., Jr Trends in outcomes after percutaneous coronary intervention for chronic total occlusions: a 25-year experience from the Mayo Clinic. J Am Coll Cardiol. 2007;49:1611–8. doi: 10.1016/j.jacc.2006.12.040. [DOI] [PubMed] [Google Scholar]
- 8.Stone GW, Colombo A, Teirstein PS, et al. Percutaneous recanalization of chronically occluded coronary arteries: procedural techniques, devices, and results. Catheter Cardiovasc Interv. 2005;66:217–36. doi: 10.1002/ccd.20489. [DOI] [PubMed] [Google Scholar]
- 9.Morino Y, Abe M, Morimoto T, et al. Predicting successful guidewire crossing through chronic total occlusion of native coronary lesions within 30 minutes: the J-CTO (Multicenter CTO Registry in Japan) score as a difficulty grading and time assessment tool. JACC Cardiovasc Interv. 2011;4:213–21. doi: 10.1016/j.jcin.2010.09.024. [DOI] [PubMed] [Google Scholar]
- 10.Nombela-Franco L, Urena M, Jerez-Valero M, et al. Validation of the J-chronic total occlusion score for chronic total occlusion percutaneous coronary intervention in an independent contemporary cohort. Circ Cardiovasc Interv. 2013;6:635–43. doi: 10.1161/CIRCINTERVENTIONS.113.000447. [DOI] [PubMed] [Google Scholar]
- 11.Syrseloudis D, Secco GG, Barrero EA, et al. Increase in J-CTO lesion complexity score explains the disparity between recanalisation success and evolution of chronic total occlusion strategies: insights from a single-centre 10-year experience. Heart. 2013;99:474–9. doi: 10.1136/heartjnl-2012-303205. [DOI] [PubMed] [Google Scholar]
- 12.Galassi AR, Tomasello SD, Reifart N, et al. In-hospital outcomes of percutaneous coronary intervention in patients with chronic total occlusion: insights from the ERCTO (European Registry of Chronic Total Occlusion) registry. EuroIntervention. 2011;7:472–9. doi: 10.4244/EIJV7I4A77. [DOI] [PubMed] [Google Scholar]
- 13.Michael TT, Karmpaliotis D, Brilakis ES, et al. Procedural outcomes of revascularization of chronic total occlusion of native coronary arteries (from a multicenter United States registry) Am J Cardiol. 2013;112:488–92. doi: 10.1016/j.amjcard.2013.04.008. [DOI] [PubMed] [Google Scholar]
- 14.Brilakis ES, Grantham JA, Rinfret S, et al. A percutaneous treatment algorithm for crossing coronary chronic total occlusions. JACC Cardiovasc Interv. 2012;5:367–79. doi: 10.1016/j.jcin.2012.02.006. [DOI] [PubMed] [Google Scholar]
- 15.Morino Y, Kimura T, Hayashi Y, et al. In-hospital outcomes of contemporary percutaneous coronary intervention in patients with chronic total occlusion insights from the J-CTO Registry (Multicenter CTO Registry in Japan) JACC Cardiovasc Interv. 2010;3:143–51. doi: 10.1016/j.jcin.2009.10.029. [DOI] [PubMed] [Google Scholar]
- 16.Christopoulos G, Menon RV, Karmpaliotis D, et al. Application of the “hybrid approach” to chronic total occlusions in patients with previous coronary artery bypass graft surgery (from a Contemporary Multicenter US registry) Am J Cardiol. 2014;113:1990–4. doi: 10.1016/j.amjcard.2014.03.039. [DOI] [PubMed] [Google Scholar]
- 17.Singh M, Bell MR, Berger PB, Holmes DR., Jr Utility of bilateral coronary injections during complex coronary angioplasty. J Invasive Cardiol. 1999;11:70–4. [PubMed] [Google Scholar]
- 18.Karmpaliotis D, Lembo N, Kalynych A, et al. Development of a high-volume, multiple-operator program for percutaneous chronic total coronary occlusion revascularization: procedural, clinical, and cost-utilization outcomes. Catheter Cardiovasc Interv. 2013;82:1–8. doi: 10.1002/ccd.24387. [DOI] [PubMed] [Google Scholar]


