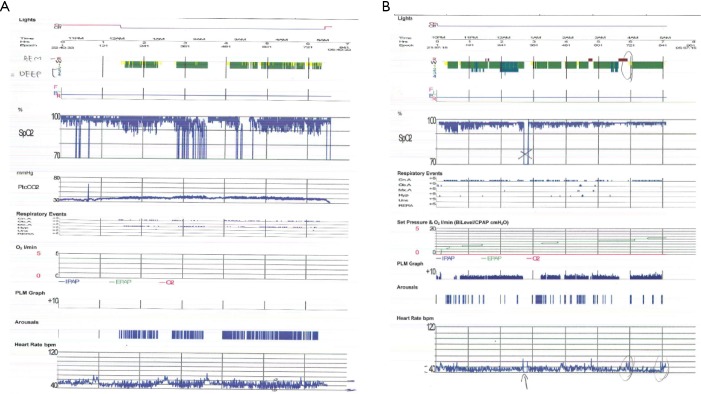
Figure 1.
Overnight diagnostic and CPAP implementation polysomnograms in a 71-year-old male with mitral valve prolapse, atrial fibrillation and normal systolic function. The diagnostic study (A) indicates modest central sleep apnoea (AHI, 46 eph; minimum SpO2, 75%) whilst 72 kg. Soon thereafter a CPAP study was performed in which oxygenation is much improved (minimum SpO2, 90%), yet AHI is still high (32 eph) due to persistent central apnoeas. He later proceeded to a mitral valve repair and ablation of cardiac accessory conducting pathways with pacemaker insertion. Follow-up polysomnogram (B) without CPAP in sinus rhythm was then normal (AHI <5 events per hour and minimum SpO2, 92%). This case highlights the difficulty in managing CSA-CSR with CPAP compared with the ease following mitral valve repair and abolition of atrial fibrillation. CPAP, continuous positive airway pressure; AHI, apnea hypopnea index; CSA-CSR, central sleep apnoea with cheyne stokes respiration.