Abstract
Objective
The objective of this study was to determine the relationships between adverse childhood experiences (ACEs) and mental health, chronic medical conditions and social development among young children in the child welfare system.
Methods
This was a cross-sectional study, using a nationally representative sample of children investigated by child welfare (National Survey of Child and Adolescent Well-Being II) from 2008–2009. Our analysis included caregiver interviews and caseworker reports about children age 18–71 months who were not in out-of-home care (N=912). We examined the associations between ACEs and mental health (measured by the Child Behavior Checklist (CBCL)), reported chronic medical conditions, and social development (measured by the Vineland Socialization Scale), in bivariate and multivariate analyses.
Results
Nearly all children (98.1%) were reported to have had an ACE in their lifetime; the average number of ACEs was 3.6. For every additional reported ACE there was a 32% increased odds of having a problem score on the CBCL (Odds Ratio (OR)=1.32, 95% Confidence Interval (CI): 1.14, 1.53), and a 21% increased odds of having a chronic medical condition (OR=1.21, 95% CI: 1.05, 1.40). Among children 36–71 months, for every additional reported ACE there was a 77% increased odds of a low Vineland Socialization score (OR=1.77, 95% CI: 1.12, 2.78).
Conclusion and Relevance
ACEs were associated with poor early childhood mental health and chronic medical conditions, and, among children age 3–5, social development. Efforts are needed to examine whether providing early intervention to families with multiple stressors mitigates the impact of ACEs on children’s outcomes.
Keywords: Adverse childhood experiences, ACEs, child welfare, mental health
Introduction
Toxic stress has been defined as exposure to chronic, severe and prolonged stress, occurring in the absence of protective factors.1 Excessive stress in early childhood is a particular risk because it can disrupt developing brain circuits and increase levels of stress hormones, both of which can lead to problems lasting into adulthood.2
The Adverse Childhood Experiences (ACE) study, a collaboration between the U.S. Centers for Disease Control and Kaiser Permanente, was a retrospective study examining the long-term impact of adverse experiences, such as childhood abuse, neglect and household dysfunction, that may cause stress.3 This study demonstrated that greater numbers of stressors experienced early in life were associated with later-in-life risk-taking and unhealthy lifestyles, as well as with disease,4 suggesting that cumulative stress, or allostatic load,5 can have lifetime effects on health. Subsequent research has shown ACEs to be linked to neurobiological changes, as well as both structural and functional alterations in the brain.6,7 However, most ACEs research has occurred retrospectively among individuals already living with exposure to stress for years.8–10 While some research has found relationships between adverse experiences and health outcomes among children,11–14 the literature is unclear as to whether early exposure to multiple stressors has relatively immediate and measurable consequences among young children at risk for removal from the home. Further, although there is research showing that more than half of children in the child welfare system have experienced four or more ACEs,15 little attention has been specifically paid to the prevalence of ACEs among the at-risk group of children who have been referred to child welfare services but not removed from the home.
In this study, we examine the adverse experiences of young children investigated by US child welfare agencies using data from the National Survey of Child and Adolescent Well-Being (NSCAW) II. Specifically, this paper examines the prevalence of ACEs among young children who have remained in their homes, as well as the relationships between ACEs and mental health, chronic medical conditions, and social development among those children. The ability to identify the children most at risk in this highly vulnerable population will better enable limited resources to be appropriately targeted.
Methods
Design and Analytic Sample
We used data from the baseline interviews of NSCAW II, a study of 5,872 youth ages 0 to 17.5 years referred to US child welfare agencies for whom an investigation of potential maltreatment was completed between February 2008 and April 2009.16 Interviews were conducted with caregivers and child welfare workers. Initial interviews were conducted approximately 4–5 months after completed child welfare investigations.17
NSCAW II, like its predecessor NSCAW I, used a two-stage national probability sample. In the first stage, primary sampling units (PSUs, most often single counties) were sampled. Of the 92 original PSUs in NSCAW I, 71 were eligible and agreed to participate in NSCAW II; 10 additional PSUs were added to replace the PSUs that declined to participate or were no longer eligible.17 In the second stage, children were sampled from lists of closed child welfare investigations within participating PSUs. At the child level, only one child was sampled from each home.
Measures
Adverse Childhood Experiences
ACEs, as defined in the original research on this topic, consist of 10 adverse events including exposure to maltreatment, and to specific caregiver and household characteristics,3 all of which were available in the NSCAW II data (Table 1). To create ACEs categories that match the originals as closely as possible, we followed the categorization used by Stanbaugh et al. (2013)15 with a few exceptions (see Table 1). For example, while Stambaugh included abandonment and deceased parent in the “parental separation or divorce” ACE we did not, based on the original definition of this ACE.3 Further, Stambaugh included forced sex as reported by youth, but this measure was only used among children age >11 in this dataset so it was not possible to analyze this variable with our young sample.
Table 1.
ACEs definitions in this NSCAW II study, compared to original CDC study constructs
| Original CDC study ACE Construct1 |
Current NSCAW II study |
|---|---|
| Physical abuse |
|
| Sexual abuse |
|
| Emotional abuse |
|
| Physical neglect |
|
| Emotional neglect |
|
| Mother treated violently |
|
| Household substance abuse |
|
| Household mental illness |
|
| Parental separation or divorce |
|
| Incarcerated household member |
|
Centers for Disease Control and Prevention. Adverse childhood experiences (ACE) study. http://www.cdc.gov/violenceprevention/acestudy/. Accessed April 12, 2014.
Parent-child conflict tactics scale
Conflict tactics scale
Composite international diagnostic interview short-form
In the NSCAW II data, current maltreatment type was based on information from the case file. Six variables representing different types of maltreatment over the lifetime were coded as having been reported (not necessarily substantiated) or not by caregiver or caseworker, and were collapsed into 5 variables: (1) any physical abuse ever, (2) any sexual abuse ever, (3) any emotional abuse ever, (4) any physical neglect/abandonment ever and (5) emotional neglect in past 12 months. The ACEs category “Mother treated violently” was measured systematically with 9 questions from the Physical Violence Scale of the Revised Conflict Tactics Scale, which assesses domestic violence against the caregiver in the past year (reliability α=.86).18 Household substance abuse was measured with risk assessment items on the caseworker questionnaire, or a score of 8 or higher on the AUDIT or an 11 or higher on the DAST-20, both of which were systematically implemented and have been shown to have high sensitivity and specificity;19.20 substance abuse was defined as alcohol or drug abuse by the primary or secondary caregiver. Household mental illness was measured by direct caseworker report of primary caregiver serious mental health or emotional problem, and by the CIDI-SF, which was systematically implemented and included problems experienced by both the primary and secondary caregiver in the last 12 months. The CIDI-SF is a self-report screening tool to assess for the presence of 8 mental health and substance use disorders. It was developed by the World Health Organization and adapted from the Composite International Diagnostic Interview, which has been shown to have an overall kappa of .77, diagnostic sensitivity of .74 and specificity of .98.21 Parental separation or divorce was based on caregiver status at the time of the baseline interview. Incarcerated household member was based on the recent arrest or detention of the primary and secondary caregivers as reported on the caseworker questionnaire or by the caregiver.
Demographics
Demographic information was collected from the caregiver at the baseline interview and included child age, gender, and race/ethnicity; caregiver age, education, and employment status; and family income. Federal poverty level (FPL) was calculated based on income and household size.
Dependent Variables
The Child Behavior Checklist (CBCL 1.5–5), a symptom checklist, was administered to caregivers of children 18–71 months of age. The CBCL provides reports from caregivers regarding a child's competencies and behavioral/emotional problems. A T-score of >= 64 is considered a clinically significant problem score. We did not include the sub-clinical range because preliminary analyses showed that its relationship to ACEs did not differ from the nonclinical range. Test-retest reliability for the Total Problem Score is .90 and the CBCL 1.5–5 correctly classifies 84.2% of children referred for mental health services as in need of those services (7.3% false positives and 8.6% false negatives).22
To determine chronic medical conditions, we used a measure developed by Stein et al. (2013) using NSCAW II data.17 The measure included diagnoses that are usually considered chronic, as well as others where chronicity is possible, but uncertain: asthma, attention-deficit/hyperactivity disorder, AIDS, autism, Down syndrome, diabetes, cystic fibrosis, mental retardation/developmental disabilities, cerebral palsy, muscular dystrophy, heart problems, hypertension, blood problems, migraines/frequent headaches, arthritis/joint problems, dental problems, repeated ear infections and back/neck problems, depression, anxiety and eating disorders, and other health problems. Children were considered to have a chronic medical condition if they had at least one of these reported diagnoses.
The Vineland Adaptive Behavior Scale (VABS) Screener, delivered to caregivers, was designed to measure daily living skills among children ages 1 to 18 years. The 45-item screener was developed from the 261-item VABS.23 NSCAW II included both the Daily Living Skills and Socialization domains, but only the latter is included in this analysis to measure social development. The Socialization scale includes interpersonal relationships, play and leisure time and coping skills, and has been shown to have high internal consistency (alpha=0.96), high intra-class correlation between parents (0.92) and high test-retest intra-class correlation (0.91).24 Children were considered to have low scores if their VABS was less than 70.
Analysis
NSCAW-developed probability weights were used in all analyses. Analysis weights were constructed in stages corresponding to the stages of the sample design, accounting for the probability of county selection and the probability of each child's selection within a county, given the youth's county of residence. Weights were further adjusted to account for small deviations from the original sampling plan, and for non-response patterns. All estimates were generated using the weights and therefore results can be inferred to the investigated U.S. child welfare population.
Initial analyses examined the weighted distribution of demographic factors and ACEs in our sample. We then examined the association between ACEs and children’s mental health (CBCL), reported chronic medical conditions and social development (Vineland Socialization Scale) in bivariate and multivariable analyses. Weighted bivariate analyses were also stratified by age group to reflect potential differences in the relationship between ACEs and our outcomes in toddlers and pre-school/school-aged children (18–35 months vs. 36–71 months). Weighted multivariable logistic regression models predicting a problem CBCL score, chronic medical conditions, and a low Vineland Socialization score were constructed in a stepwise fashion, and demographic factors, including child’s age and race/ethnicity, caregivers’ age and FPL, were individually deleted from the model if they were not significant at alpha=.05; demographic factors were also tested as confounders. Based on the bivariate analyses, an interaction term between ACE count and child age was tested in the models as well. Full models resulted in similar findings to the reduced models, so only the reduced models are presented here.
All procedures for NSCAW II were approved by the Research Triangle Institute's IRB and all analytic work on the NSCAW II de-identified data has been approved by the Rady Children's Hospital IRB. All analyses used SAS callable SUDAAN, version 11.
Results
Sample
Our sample is restricted to young children (ages 18–71 months) in order to examine stressors experienced in early childhood. Although measures were available for 12–17 month-olds, in some instances they were different than the measures used for older children so we did not include them due to difficulties making comparisons across measures. Analyses were further restricted to children and families in which the child did not experience an out-of-home placement from the time of the index child welfare report to the time of the baseline interview. This restriction was applied in order to focus on this particular vulnerable group of children, and because the stress of a current out-of-home placement may confound the relationship between ACEs and children’s health.25 The total sample for these analyses was 912 children (317 age 18–35 months; 595 age 36–71 months) and their caregivers.
Just over half (55.4%) of the sampled children were male; almost a quarter were black (23.6%), almost a third Hispanic (30.3%), and 40.2% white. More than two-thirds of the children were 36–71 months old (69.3%). Most caregivers were under 35 years old (81%), and more than one-quarter (28.5%) had less than a high school degree. Half were unemployed (50.6%) and nearly two-thirds (62.8%) had incomes under 100% of the federal poverty level (Table 2).
Table 2.
Baseline characteristics and mean adverse childhood events (ACEs), Baseline NSCAW II, 2008–2009 (N=912)
| Number of ACEs | ||||
|---|---|---|---|---|
| Weighted % |
Weighted Mean |
SE Means |
Lower mean, Upper mean |
|
| Total Sample | 3.61 | .11 | 3.40, 3.83 | |
| Child’s gender | ||||
| Male | 55.4 | 3.63 | .11 | 3.40, 3.85 |
| Female | 44.6 | 3.60 | .19 | 3.22, 3.98 |
| Child’s race/ethnicity | ||||
| Black | 23.6 | 3.57 | .18 | 3.22, 3.92 |
| White | 40.2 | 3.77 | .15 | 3.47, 4.08 |
| Hispanic | 30.3 | 3.48 | .19 | 3.10, 3.86 |
| Other | 5.8 | 3.50 | .42 | 2.67, 4.34 |
| Child’s Age | ||||
| 18–35 mo | 30.7 | 3.29 | .19 | 2.90, 3.68 |
| 36–71 mo | 69.3 | 3.76 | .13 | 3.49, 4.02 |
| Caregiver’s agea | ||||
| <=24 | 33.9 | 3.41 | .18 | 3.05, 3.77 |
| 25–34 | 47.1 | 3.90 | .14 | 3.61, 4.19 |
| 35+ | 19.0 | 3.27 | .22 | 2.82, 3.71 |
| Caregiver’s degree | ||||
| Less than HS | 28.5 | 3.48 | .21 | 3.06, 3.90 |
| HS | 47.2 | 3.60 | .12 | 3.36, 3.85 |
| HS plus | 24.3 | 3.79 | .15 | 3.50, 4.09 |
| Caregiver’s employment | ||||
| Any employment | 47.3 | 3.57 | .12 | 3.34, 3.80 |
| Unemployed | 50.6 | 3.63 | .17 | 3.30, 3.97 |
| Other | 2.1 | 3.99 | .25 | 3.50, 4.49 |
| Federal Povertya | ||||
| <100% | 62.8 | 3.74 | .15 | 3.45, 4.04 |
| 100–200% | 25.4 | 3.73 | .16 | 3.41, 4.05 |
| >200% | 11.8 | 3.16 | .19 | 2.78, 3.53 |
| CBCLc | ||||
| >=64 | 13.6 | 4.30 | .24 | 3.82, 4.77 |
| <64 | 86.4 | 3.51 | .10 | 3.31, 3.71 |
| Chronic Medical Conditionb | ||||
| Yes | 35.5 | 3.93 | .10 | 3.72, 4.14 |
| No | 64.5 | 3.44 | .15 | 3.13, 3.74 |
| Vineland Socialization | ||||
| Severe | 8.0 | 3.67 | .63 | 2.43, 4.92 |
| Moderate | 92.0 | 3.61 | .09 | 3.42, 3.79 |
p<.05
p<.01
p<.001
Thirteen point six percent of these young children scored over the problem score cutoff (>=64) on the CBCL. More than one-third (35.5%) were reported to have a chronic medical condition, and 8% had a low score (<70) on the Vineland.
Distribution of ACEs
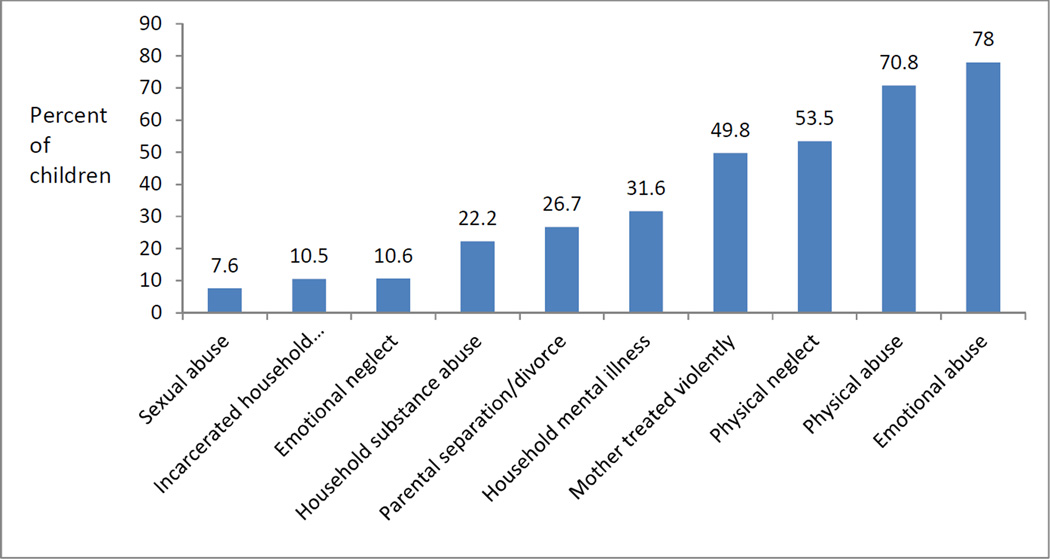
Nearly all children (98.1%) were reported to have experienced at least one ACE; 7.7% were reported to have one ACE, 39.9% two or three ACEs and 50.5% four or more ACEs. Around three-quarters of all young children were reported to have experienced emotional (78.0%) or physical (70.8%) abuse. About half were reported to have experienced physical neglect (53.5%) or caregiver violence (49.8%); more than a third were reported to have a caregiver with mental health or emotional problems (31.6%), and one quarter were reported to have a caregiver who was separated or divorced (26.7%). One in five reported household substance abuse (22.2%), and one in ten reported emotional neglect (10.6) or a caregiver with a recent history of arrest or detention (10.5%). Few children were reported to have experienced sexual abuse (7.6%) (Figure 1).
Figure 1.
Distribution of ACEs, baseline NSCAW II, 2008–2009
Variation in the mean number of ACEs
Children had a mean of 3.6 ACEs. Those whose caregivers were 25–34 years old had more reported ACEs than those with younger or older caregivers (3.9 vs. 3.4 and. 3.3, p<.05 for both comparisons), and children living in more than 200% of the federal poverty line (FPL) had fewer reported ACEs than those living in <100% or 100–200% of the FPL (3.2 vs. 3.7 and 3.7, p<.05 for both comparisons). There were no other differences in mean number of reported ACEs by demographic characteristics (Table 2).
There were differences in the numbers of reported ACEs by children’s mental health, chronic medical conditions, and social development. Children who scored over the CBCL problem score cutoff had more reported ACEs than those who did not (4.3 vs. 3.5, p<.001). However, stratified analyses showed that this relationship was only significant among older children (36–71 months) (4.4 vs. 3.6, p=.009). In addition, children with chronic medical conditions had more reported ACEs than those without chronic medical conditions (3.9 vs. 3.4, p=.009). Again, this relationship only held among older children (4.1 vs. 3.5, p=.011). In the full sample, average reported ACEs did not differ by Vineland score. However, among older children (36–71 months) low Vineland scores were associated with having more reported ACEs (5.4 vs. 3.7, p=.049). This relationship was not significant among younger children.
In multivariable logistic regression analyses, the number of ACEs reported for a child significantly predicted CBCL score (the interaction term between ACE count and child age was not significant). For every additional reported adverse experience there was a 32% increase in the odds of having a problem score on the CBCL (OR=1.32 95% CI: 1.14, 1.53; p<.001; Table 3). Similarly, each additional ACE increased the odds of having a chronic medical condition by 21% (OR=1.21, 95% CI: 1.05, 1.40, p=.01); again, the interaction term was not significant. When we examined social development, we found that the interaction between adverse experiences and child age was significant (p=.019). Among children age 36–71 months, for every additional reported adverse experience there was a 77% increase in the odds of a low Vineland socialization score (OR=1.77, 95% CI: 1.12, 2.78; p=.015). Among younger children, age 18–35 months, the relationship was not significant (OR: .81, 95% CI: .55, 1.18; p=.266).
Table 3.
Multivariable models predicting mental health, physical health, and development problems, baseline NSCAW II, 2008–2009
| Ods Ratio | 95% Confidence Interval |
P-Value | |
|---|---|---|---|
| Mental health problema | |||
| ACE Count | 1.32 | 1.14, 1.53 | <.001 |
| Chronic Medical Conditionb,c | |||
| ACE Count | 1.21 | 1.05, 1.40 | .010 |
| Social development problemd,e | |||
| Child age * ACE Count | 2.2 | 1.14, 4.26 | .019 |
Mental health problems are measured with the CBCL total score (mental health problem >=64).
Chronic medical conditions are measured with a composite score from Stein et al. (2013)17
Model also includes child gender and caregiver education
Social development problems are measured with the Vineland Socialization score (development problem <70).
Model also includes child race/ethnicity, caregiver employment and main effects for the statistically significant interaction.
Discussion
In this study of children in the child welfare system, we found high rates of adverse experiences. The number of ACEs children experienced varied by only a few demographic characteristics; children with caregivers age 25–34 years, on average, experienced more ACEs, as did children living in greater levels of poverty. Further, a greater number was found among those with mental health and chronic medical problems, and, among older children, social development problems. These data highlight the prevalence of adverse experiences among very young children in a most vulnerable population, and suggest that the physiological results of toxic stress may begin almost immediately.
On average, young children in our sample were reported to have more than 3 ACEs. This is troubling, as early childhood toxic stress has been shown to be related to physiologic disruptions, such as alterations in immune function26 and increases in inflammatory markers,27,28 which are associated with many significant poor health outcomes.29–31 Prior research has also shown that adolescents and adults who experienced multiple childhood adversities are more likely to experience mental illness and adopt unhealthy later-life behaviors as coping mechanisms.4,8–10
Further, half were reported to have 4 or more adverse experiences. This is similar to the 51% reported by Stambaugh and colleagues,15 who also used NSCAW II to examine adverse events among children in in-home and out-of-home care. Although data from the 2011–2012 National Survey of Children’s Health show that children living in out-of-home care report more adverse experiences,32 our data suggest that all children in contact with the child welfare system, not only those in out-of-home placements, are at higher risk for multiple adverse experiences.
Our analyses found high rates of mental health and chronic medical problems, compared to community samples,33,34 but children in our study had a similar prevalence of social development problems to the general population.35 Moreover, we found that a higher number of ACES before age 5 was associated with a greater likelihood of mental health and chronic medical problems. However, the association between ACEs and social development was only significant among 3–5 year-olds. This suggests that response to stress may develop over time as allostatic load increases.36,37 Alternatively, it may be that relationship between ACEs and social development changes over time, at different stages of development. Clearly, this study cannot establish directionality; while ACEs may lead to poor childhood outcomes, prior research has suggested that poor childhood health can lead to adverse childhood experiences.38 However, among very young children the latter is less likely, and our findings suggest that adverse experiences are associated with a range of proximal negative outcomes. That signs of poor health and social development are apparent in children this young suggests that stress may have an immediate impact and should be addressed by pediatric health care providers, who are usually the only health professionals to routinely interact with children this young.39 This will increasingly be true as more families have routine access to health care as a result of the Affordable Care Act.
Most previous studies have examined the association between ACEs and health outcomes retrospectively among adults who have lived with the effects of their adverse experiences for years. The few studies that have focused on children report findings similar to ours. For example, Marie-Mitchell and colleagues studied 4 and 5 year-olds in an urban health center and found a relationship between adverse experiences and developmental delays and injuries, but found mixed results regarding physical health.11 Similarly, Burke et al. showed that an increased number of ACEs was associated with an increased risk of learning or behavioral disorders and a high body mass index among children and adolescents in a child health center.12 Flaherty et al. followed young children at risk for abuse and neglect and found that an accumulation of 4 adverse experiences at 4 years tripled the risk of illness two years later;13 similar, although somewhat mixed, results were found when these children were examined at age 12.14 Our results suggest that the effects of adverse experiences may occur almost immediately and even the very youngest children are not immune.
These data are not without limitations. Our categorization of ACEs was slightly different from the original ACE study, and some of our variables did not capture events over the lifetime, as the original ACE study did. However, given the young age of our study population, the difference between these time frames is not great and the variables used here are conceptually comparable to the original study. Additionally, all data were taken from caregiver interviews or caseworker reports; no independent verification of the accuracy of the reporting was conducted, and since some measures were not gathered with a systematic protocol, using case file data to describe ACEs may not accurately capture each adverse experience. Further, caregivers with mental health or emotional issues may be more likely to report worse outcomes in their children. The number of children in some categories, such as older children with severe Vineland scores, was small; small numbers and the lack of a true no-risk group may have tempered some of our findings. In addition, the measures used are not comprehensive and without limitations. For example, although the CBCL and CIDI-SF correlate well with psychiatric diagnoses, neither is a diagnostic measure. As a result, these mental health measures should be considered indicators of potential mental health problems. Similarly, although the Vineland Socialization scale is a valid measure of social development, it captures only one domain of development and is sensitive to age effects. Finally, the data are cross-sectional and, thus, cannot determine causation or directionality.
Conclusion
This examination of a nationally representative sample of children in the child welfare system highlights the challenges facing even very young children who remain in their homes, and shows that early adverse childhood experiences may lead to early childhood mental health, chronic medical and social development problems. This suggests that even within the child welfare population, it may make sense to target prevention efforts to children who have experienced more adverse experiences. However, a rigorous, prospective study should be performed to prove the association between ACEs and poor childhood outcomes among young children. Once proven, efforts should be made to understand if early intervention can prevent adverse health outcomes. Assessments during prenatal and pediatric healthcare visits may be important to identifying at-risk caregivers and link them to needed services.40 In fact, recognizing that addressing behavioral and developmental concerns is essential to children’s health, the American Academy of Pediatrics suggests that the “boundaries of pediatric concern must move beyond the acute medical care of children,”41 and provides physicians with sample screening tools to use with their patients (https://www.aap.org/en-us/Documents/ttb_addressing_aces.pdf). With early intervention, some of the short- and long-term negative outcomes associated with ACEs may be averted.
What’s new.
Adverse childhood experiences (ACEs) were prevalent in 18–71 month-olds in child welfare, and were associated with poor mental health and chronic medical conditions, and, among 36–71 month-olds, social development. This suggests that ACEs may have short-term effects on young children.
Acknowledgments
Funding: National Institute of Mental Health P30MH090322, Principal Investigator: Kimberly Hoagwood
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Financial Disclosure Statement: No author has a financial relationship relevant to this article to disclose.
Conflict of Interest Statement: No author has a conflict of interest to disclose.
Contributor Information
Bonnie D. Kerker, Email: Bonnie.kerker@nyumc.org.
Jinjin Zhang, Email: jjzhang@rchsd.org.
Erum Nadeem, Email: Erum.nadeem@nyumc.org.
Ruth E. K. Stein, Email: ruth.stein@einstein.yu.edu.
Michael S. Hurlburt, Email: hurlburt@usc.edu.
Amy Heneghan, Email: HeneghA@pamf.org.
John Landsverk, Email: Jlandsverk@aol.com.
Sarah McCue Horwitz, Email: Sarah.horwitz@nyumc.org.
References
- 1.Shonkoff JP, Garner AS Committee on Psychosocial Aspects of Child and Family Health, Committee on Early Childhood, Adoption, and Dependent Care, Section on Developmental and Behavioral Pediatrics. The lifelong effects of early childhood adversity and toxic stress. Pediatrics. 2012;129(1):e232–e246. doi: 10.1542/peds.2011-2663. [DOI] [PubMed] [Google Scholar]
- 2.National Scientific Council on the Developing Child. Excessive stress disrupts the architecture of the developing brain. [Accessed September 19, 2013];Working Paper No. 3. http://developingchild.harvard.edu/resources/reports_and_working_papers/working_papers/wp3/. [Google Scholar]
- 3.Centers for Disease Control and Prevention. Adverse childhood experiences (ACE) study. [Accessed April 12, 2014]; http://www.cdc.gov/violenceprevention/acestudy/.
- 4.Middlebrooks JS, Audage NC. The Effects of Childhood Stress on Health Across the Lifespan. Atlanta (GA): Centers for Disease Control and Prevention, National Center for Injury Prevention and Control; 2008. [Google Scholar]
- 5.McEwen BS, Seeman T. Protective and damaging effects of mediators of stress: elaborating and testing the concepts of allostasis and allostatic load. Ann NY Acad Sci. 1999;896:30–47. doi: 10.1111/j.1749-6632.1999.tb08103.x. [DOI] [PubMed] [Google Scholar]
- 6.Heim C, Nemeroff CB. The role of childhood trauma in the neurobiology of mood and anxiety disorders: Preclinical and clinical studies. Biological Psychiatry. 2001;49(12):1023–1039. doi: 10.1016/s0006-3223(01)01157-x. [DOI] [PubMed] [Google Scholar]
- 7.Kaufman J, Plotsky PM, Nemeroff CB, Charney DS. Effects of early adverse experiences on brain structure and function: Clinical implications. Biological Psychiatry. 2000;48(8):778–790. doi: 10.1016/s0006-3223(00)00998-7. [DOI] [PubMed] [Google Scholar]
- 8.Felitti VJ, Anda RF, Nordenberg D, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: The Adverse Childhood Experiences (ACE) Study. Am J Prev Med. 1998;14(4):245–258. doi: 10.1016/s0749-3797(98)00017-8. [DOI] [PubMed] [Google Scholar]
- 9.Anda RF, Croft JB, Felitti VJ, et al. Adverse childhood experiences and smoking during adolescence and adulthood. The Journal of the American Medical Association. 1999;282(17):1652–1658. doi: 10.1001/jama.282.17.1652. [DOI] [PubMed] [Google Scholar]
- 10.Rothman EF, Edwards EM, Heeren T, Hingson RW. Adverse childhood experiences predict earlier age of drinking onset: results from a representative US sample of current or former drinkers. Pediatrics. 2008;122:e298–e304. doi: 10.1542/peds.2007-3412. [DOI] [PubMed] [Google Scholar]
- 11.Marie-Mitchell A, O'Connor TG. Adverse childhood experiences: translating knowledge into identification of children at risk for poor outcomes. Acad Pediatr. 2013;13(1):14–19. doi: 10.1016/j.acap.2012.10.006. [DOI] [PubMed] [Google Scholar]
- 12.Burke NJ, Hellman JL, Scott BG, Weems CF, Carrion VG. The impact of adverse childhood experiences on an urban pediatric population. Child Abuse Negl. 2011;35(6):408–413. doi: 10.1016/j.chiabu.2011.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Flaherty EG, Thompson R, Litrownik AJ, et al. Effect of early childhood adversity on child health. Arch Pediatr Adolesc Med. 2006;160(12):1232–1238. doi: 10.1001/archpedi.160.12.1232. [DOI] [PubMed] [Google Scholar]
- 14.Flaherty EG, Thompson R, Litrownik AJ, et al. Adverse childhood exposures and reported child health at age 12. Acad Pediatr. 2009;9(3):150–156. doi: 10.1016/j.acap.2008.11.003. [DOI] [PubMed] [Google Scholar]
- 15.Stambaugh LF, Ringeisen H, Casanueva CC, Tueller S, Smith KE, Dolan M. Adverse childhood experiences in NSCAW. Washington, DC: Office of Planning, Research and Evaluation, Administration for Children and Families, U.S. Department of Health and Human Services; 2013. [Google Scholar]
- 16.Dowd K, Dolan M, Wallin J, et al. National Survey of Child and Adolescent Well-Being II: Combined Waves 1–2 Data File User's Manual Restricted Release Version. Ithaca, NY: Cornell University, National Data Archive on Child Abuse and Neglect; 2011. [Google Scholar]
- 17.Stein REK, Hurlburt MS, Heneghan AM, et al. Chronic conditions among children investigated by child welfare: a national sample. Pediatrics. 2013;131(3):455–462. doi: 10.1542/peds.2012-1774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Straus MA, Hamby SL, Boney-McCoy S, Sugarman DB. The revised conflict tactics scales (CTS2): development and preliminary psychometric data. J Fam Issues. 1996;17(3):283–316. [Google Scholar]
- 19.Reinert DF, Alen JP. The Alcohol use disorder identification test (AUDIT): A review of recent research. Alcoholism: Clinical and Experimental Research. 2002;26(2):272–79. [PubMed] [Google Scholar]
- 20.Yudko E, Lozhkina O, Fouts A. A comprehensive review of the psychometric properties of the drug use screening test. Journal of Substance use Treatment. 2007;32:189–198. doi: 10.1016/j.jsat.2006.08.002. [DOI] [PubMed] [Google Scholar]
- 21.Janca A, Robins LN, Cottler LB, Early TS. Clinical observation of assessment using the Composite International Diagnostic Interview (CIDI). An analysis of the CIDI Field Trials - Wave II at the St. Louis Site. Br J Psychiatry. 1992;160:815–818. doi: 10.1192/bjp.160.6.815. [DOI] [PubMed] [Google Scholar]
- 22.Achenbach TM, Rescorla LA. Manual for the ASEBA Preschool Forms & Profiles. [Accessed September 3, 2013]; http://www.aseba.org/ordering/ASEBA%20Reliability%20&%20Validity-Pre-school%20.pdf. [Google Scholar]
- 23.Sparrow SS, Carter AS, Cicchetti DV. Vineland Screener. [Accessed March 14, 2014];1993a, 1993b http://www.unc.edu/depts/sph/longscan/pages/measures/Ages12to14/writeups/Age%2012%20and%2014%20Vineland%20Screener%20FINAL%20(Public%20Site).pdf. [Google Scholar]
- 24.van Duijn G, Dijkxhoorn Y, Noens I, Scholte E, van Berckelaer-Onnes I. Vineland Screener 0–12 years research version (NL). Constructing a screening instrument to assess adaptive behaviour. Int J Methods Psychiatr Res. 2009;18(2):110–117. doi: 10.1002/mpr.282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Goldsmith DF, Oppenheim D, Wanlass J. Separation and reunification: using attachment theory and research to inform decisions affecting the placements of children in foster care. Juvenile Fam Court J. 2004;55(2):1–13. [Google Scholar]
- 26.Bierhaus A, Wolf J, Andrassy M, et al. A mechanism converting psychosocial stress into mononuclear cell activation. PNAS. 2003;100(4):1920–1925. doi: 10.1073/pnas.0438019100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Danese A, Pariante CM, Caspi A, Taylor A, Poulton R. Childhood maltreatment predicts adult inflammation in a life-course study. PNAS. 2007;104(4):1319–1324. doi: 10.1073/pnas.0610362104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Miller GE, Chen E. Harsh family climate in early life presages the emergence of a proinflammatory phenotype in adolescence. Psychol Sci. 2010;21(6):848–856. doi: 10.1177/0956797610370161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Berasain C, Perugorria MJ, Latasa MU, et al. The epidermal growth factor receptor: a link between inflammation and liver cancer. Exp Biol Med. 2009;234:713–725. doi: 10.3181/0901-MR-12. [DOI] [PubMed] [Google Scholar]
- 30.Chen E, Miller GE. Stress and inflammation in exacerbations of asthma. Brain Behav Immun. 2007;21(8):993–999. doi: 10.1016/j.bbi.2007.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Danese A, Moffitt TE, Pariante CM, Ambler A, Poulton R, Caspi A. Elevated inflammation levels in depressed adults with a history of childhood maltreatment. Arch Gen Psychiatry. 2008;65(4):409–415. doi: 10.1001/archpsyc.65.4.409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bramlett MD, Radel LF. Adverse family experiences among children in nonparental care, 2011–2012. National Health Statistics Reports. 2014;74(4):1–8. [PubMed] [Google Scholar]
- 33.Briggs-Gowan MJ, Carter AS, Skuban EM, Horwitz SM. Prevalence of Social-Emotional and Behavioral Problems in a Community Sample of 1- and 2-Year-Old Children. J of Am Academy of Child and Adolescent Psychiatry. 2001;40(7):811–819. doi: 10.1097/00004583-200107000-00016. [DOI] [PubMed] [Google Scholar]
- 34.Bethell CD, Read D, Blumberg SJ, Newacheck PW. What is the prevalence of children with special health care needs? Toward an understanding of variations in findings and methods across three national surveys. Matern Child Health J. 2008;12(1):1–14. doi: 10.1007/s10995-007-0220-5. [DOI] [PubMed] [Google Scholar]
- 35.Sukhodolsky DG, Scahill L, Zhang H, et al. Disruptive behavior in children with Tourette’s Syndrome: Association with ADHD comorbidity, TIC severity, and functional impairment. J of Am Academy of Child and Adolescent Psychiatry. 2003;42(1):98–105. doi: 10.1097/00004583-200301000-00016. [DOI] [PubMed] [Google Scholar]
- 36.Evans GW. A multimethodological analysis of cumulative risk and allostatic load among rural children. Dev Psychol. 2003;39(5):924–933. doi: 10.1037/0012-1649.39.5.924. [DOI] [PubMed] [Google Scholar]
- 37.Rogosch FA, Dackis MN, Cicchetti D. Child maltreatment and allostatic load: consequences for physical and mental health in children from low-income families. Dev Psychopathol. 2011;23(4):1107–1124. doi: 10.1017/S0954579411000587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sherrod KB, O'Connor S, Vietze PM, Altemeier WA., 3rd Child health and maltreatment. Child Dev. 1984;55(4):1174–1183. [PubMed] [Google Scholar]
- 39.Wertlieb D. Converging trends in family research and pediatrics: recent findings for the American Academy of Pediatrics Task Force on the Family. Pediatrics. 2003;111(6 pt 2):1572–1587. [PubMed] [Google Scholar]
- 40.Earls MF Committee on Psychosocial Aspects of Child and Family Health American Academy of Pediatrics. Incorporating recognition and management of perinatal and postpartum depression into pediatric practice. Pediatrics. 2010;126(5):1032–1039. doi: 10.1542/peds.2010-2348. [DOI] [PubMed] [Google Scholar]
- 41.Garner AS, Shonkoff JP Committee on Psychosocial Aspects of Child and Family Health, Committee on Early Childhood, Adoption, and Dependent Care, Section on Developmental and Behavioral Pediatrics. Early childhood adversity, toxic stress, and the role of the pediatrician: translating developmental science into lifelong health. Pediatrics. 2012;129(1):e224–e231. doi: 10.1542/peds.2011-2662. [DOI] [PubMed] [Google Scholar]